RichardCare


RichardCare


Pop-up Grocery Markets to Tackle Food Insecurity
Goodr, the innovative social impact company dedicated to ending food waste and hunger, and Wellstar Health System are teaming up for a fourth consecutive year to bring free, fresh food directly to communities throughout Metro Atlanta with a series of pop-up grocery markets.
The pop-ups will occur over five months: April, May, June, September and October.
For many Georgia families, accessing healthy food isn’t just a challenge—it’s a crisis. According to an October analysis by the Georgia Budget and Policy Institute, 1.6 million Georgians received benefits through the Supplemental Nutrition Assistance Program (SNAP, also known as food stamps).
Georgia is home to some of the largest food deserts in the country. Without nearby grocery stores, many residents rely on fast food and convenience stores, increasing their risk for chronic illnesses like diabetes, hypertension and heart disease. These mobile grocery pop-ups aren’t just about food—they deliver dignity, better health and hope.
“Health and wellness begin with access to nutritious food, which is a struggle for too many people in our community,” said Elise Lockamy-Kassim, assistant vice president for Wellstar Community Health and the Wellstar Center for Health Equity. “At Wellstar, we’ve found an exceptional partnership with Goodr and our network of community organizations to provide wholesome foods and health information.”
Each event will distribute approximately 20,000 pounds of fresh food, helping alleviate food insecurity for thousands of families. In addition to groceries, many events will offer free health screenings, nutrition education and wellness resources, reinforcing the connection between food and long-term health.
“These markets are more than just an opportunity for families to receive free groceries—they are a lifeline,” said Jasmine Crowe-Houston, founder and CEO of Goodr. “I’ve spoken with mothers who skip meals so their children can eat, seniors forced to ration what little they have and workers who spend most of their paycheck just to put food on the table. Thanks to Wellstar’s continued sponsorship, we serve those who need it most and work towards a future where no one must go hungry.”
All Wellstar Mobile Markets will be drive-thru events. Families must pre-register to attend (one registration per household) at wellstarmobilemarket.com or by emailing [email protected].
APRIL WELLSTAR MOBILE MARKET EVENTS:
Roswell
Thursday, April 3, 2025 | 5 – 6 PM
Roswell Organization for Community Development
Location: Zion Missionary Baptist Church
888 Zion Circle, Roswell, GA 30075
Registration now open
LaGrange
Saturday, April 5, 2025 | 10 – 11 AM
First Presbyterian Church - LaGrange
Location: AMC CLASSIC LaGrange 10
201 Main St., LaGrange, GA 30240
Registration now open
Griffin
Thursday, April 10, 2025 | 5 – 6 PM
New Mercy Baptist Church
730 Park Road, Griffin, GA 30224
Registration opens March 31
Douglasville
Thursday, April 17, 2025 | 10 – 11 AM
First Presbyterian Church of Douglasville
9190 Campbellton St., Douglasville, GA 30134
Registration opens April 7
Jackson
Tuesday, April 22, 2025 | 5 – 6 PM
Butts County Life Enrichment
Location: Jackson United Methodist Church
409 E 3rd St., Jackson, GA 30233
Registration opens April 14
Details on the May, June, September and October events will be released at a later time.
Wellstar and the Wellstar Foundation first partnered with Goodr in 2020 to tackle food insecurity during the pandemic. Initially focused on the pop-up Mobile Markets that provide food and fresh produce to thousands of families each year, the partnership has evolved to also include a Surplus Food Recovery service where unused food from hospitals is donated to community organizations.

Healing With Expertise: Comprehensive Wound Care & Hyperbaric Medicine at Wellstar

Personalized Heart Health Goes Beyond One Size Fits All


Wellstar and Colquitt Regional Medical Center Expand Training for Women’s Health Physicians
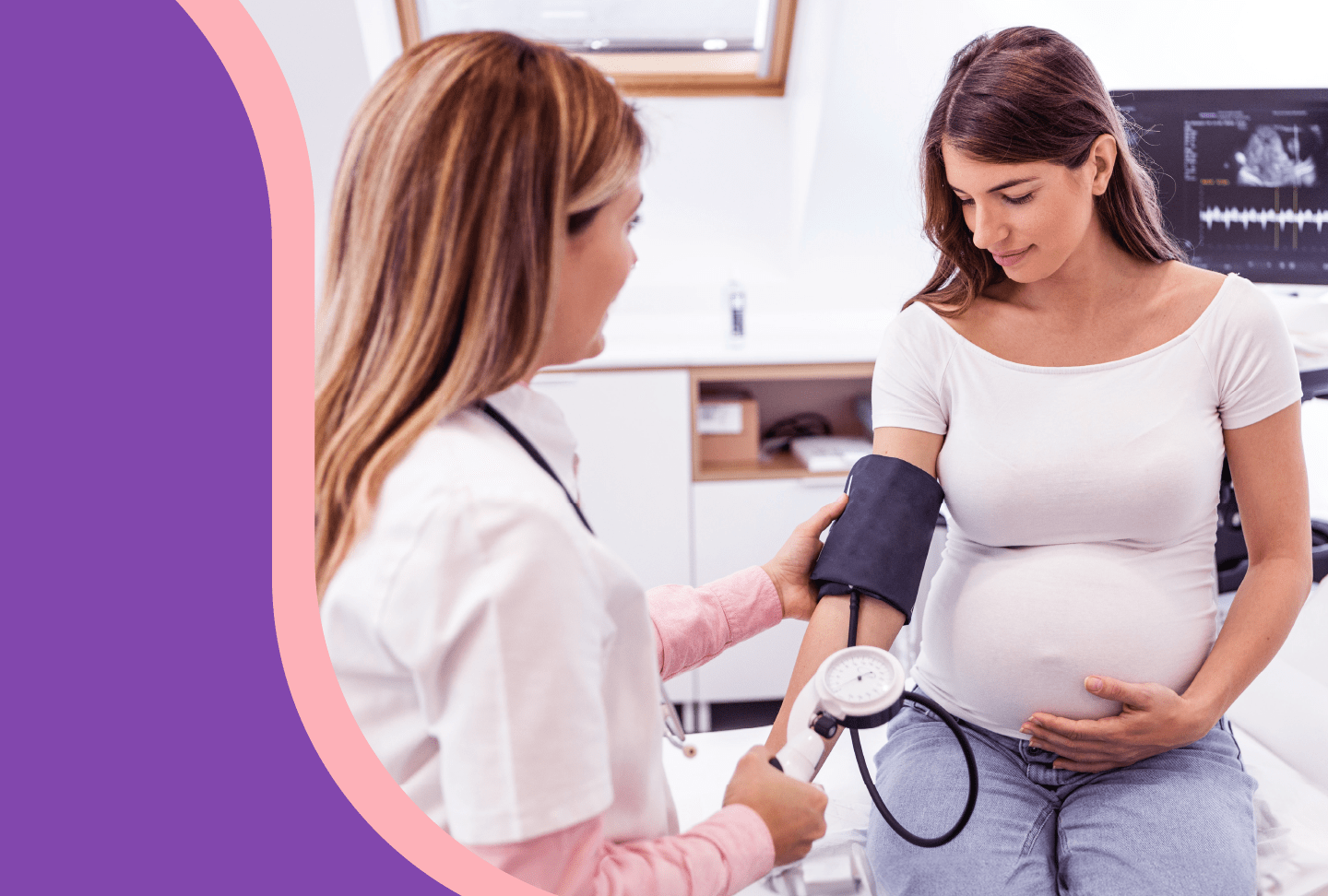
Wellstar Health System and Colquitt Regional Medical Center are launching a new residency track to train obstetrics and gynecology (OB/GYN) physicians in Marietta and Moultrie. The program is unique in that it will provide new physicians with the opportunity to train in both suburban and rural areas of Georgia.
Known as Graduate Medical Education (GME), Wellstar Kennestone Regional Medical Center's OB/GYN residency program has been approved for a rural track at Colquitt Regional in Moultrie. This rural track expansion will ultimately grow to a complement of four OB/GYN residents training on-site at Colquitt Regional at one time. Each resident physician in training will spend time at Wellstar Kennestone in Marietta, but the majority of their training will be completed at Colquitt Regional.
“This program will create opportunities for physicians specializing in women’s and maternal health to train and build their careers in rural Georgia,” said Colquitt Regional President and CEO James Matney. “It’s wonderful how Wellstar is reaching out to other health systems to help meet our local needs. Our community is encouraged and appreciative that Wellstar is helping train physicians who will care for people in rural areas across the state.”
Georgia currently ranks among the worst states in the nation for maternal care. According to the March of Dimes, more than one-third (34.6%) of Georgia counties are maternity care deserts and do not have a single obstetric healthcare provider. Additionally, Georgia is higher than the national average for maternal mortality and inadequate prenatal care. However, many maternal deaths are preventable by improving access to care.
Since 2015, 66% of physicians in training at Colquitt Regional have stayed in and near Moultrie to build their careers with residency programs that include Family Medicine, Psychiatry and General Surgery. Wellstar and Colquitt Regional aim to improve access to women’s health and maternal care in South Georgia through the new residency program.
“We have a shared goal of improving the health and wellness of every person in Georgia. This new program is another step toward meeting the critical need for physicians in rural Georgia,” said Wellstar President and CEO Candice L. Saunders. “Doctors are more likely to stay in communities where they train, which makes partnerships among health systems like Wellstar and Colquitt essential to our success.”
Including its partnership with Augusta University’s Medical College of Georgia (MCG) at Wellstar MCG Health Medical Center, Wellstar operates five teaching hospitals in the state—Wellstar Kennestone, Wellstar Cobb, Wellstar Douglas and Wellstar Spalding Medical Centers. Wellstar recently announced that its Wellstar Paulding and Wellstar West Georgia Medical Centers are also becoming designated teaching hospitals.
“Becoming a physician is an extremely rewarding experience, and that’s magnified in rural areas,” said Dr. Val Akopov, senior vice president of Wellstar Medical Group. “The physicians who train in this new program will see and feel the joy of working in a rural community.”
“Meeting the needs of people in South Georgia has always been our mission,” said Dr. Daniel York, director for OB/GYN residency at Colquitt Regional. “Our new women’s health program will go a long way to providing our region with qualified physicians in rural areas. We have enjoyed working with Wellstar to get this program approved.”
In the last decade, Wellstar has grown its GME program from 14 trainees in 2016 to nearly 300 today, many of whom have remained with Wellstar and in Georgia. Through Wellstar’s partnership with Augusta University’s Medical College of Georgia, Wellstar MCG Health is the primary clinical training site for more than 500 GME positions. With the new residencies, Wellstar will support more than 860 physicians in training.

Importance of Colon Cancer Screening
By Dr. Benjamin Renelus, Wellstar gastroenterologist
8 Heart Health Facts Moms-to-be Should Know
Wellstar Offers Advanced Colorectal Cancer Care Close to Home
When a Wellstar patient is diagnosed with colorectal cancer, their multidisciplinary care team works with them to create a personalized care plan with advanced treatment available at every step.
Patients are surrounded by a team of experts from the very beginning of their cancer care. To better prepare patients for treatment, Wellstar offers a “pre-hab” program with support services to care for patients’ overall well-being.
“Patients often ask what they can eat or do to prepare for treatment, and we want them to feel empowered,” said Wellstar Surgical Oncologist Dr. Sahir Shroff.
Patients can meet with team members including dietitians, physical therapists or behavioral healthcare providers so they feel their best both physically and mentally.
Learn more about cancer support services.
Robotic surgeries provide patients with benefits like less recovery pain, less blood loss, fewer complications and shorter hospital stays, or for some outpatient procedures, no hospital stay at all. That means patients can start living cancer-free sooner and get back to their routines and the activities they enjoy.
About 85% of colorectal cancer surgeries at Wellstar are now robotic procedures, according to Wellstar Surgical Oncologist Dr. Sartaj Sanghera.
“Robotic surgery has really provided us the tools as far as the instruments and vision so that a larger cohort of surgeons in general, colorectal surgeons and surgical oncologists have been able to adopt the technology,” Dr. Sanghera said.
Patients with smaller, early-stage tumors may be candidates for transanal minimally invasive surgery, known as TAMIS. Rather than making an incision in the abdomen to remove a tumor, the surgeon is able to access the tumor through the anus.
“It is working through a natural orifice, through the anus. It’s not actually poking a hole in the belly,” Dr. Sanghera said. “It’s really minimally invasive.”
TAMIS is usually offered as an outpatient surgery with no hospital stay. It has been especially helpful in treating patients who may be at higher risk with traditional surgery due to their age or other health conditions, Dr. Sanghera noted.
Clinicians also adapt treatment methods based on the location of the cancer, according to Dr. Shroff. For example, if one spot is near a blood vessel, the care team may opt to use radiation rather than surgery to prevent blood loss.
The colorectal cancer experts at Wellstar have adopted a relatively new approach to treatment called total neoadjuvant therapy, or TNT, which makes surgery the last step in the cancer treatment process. Patients receive chemotherapy and radiation first, then finish treatment with surgery.
“Recognizing that rectal cancer is a systemic disease, with risks of spreading to other parts of the body, we have evolved in our management of rectal cancer, offering an operation as the last step in the treatment process,” Dr. Shroff said.
Wellstar has seen positive results with this technique.
“We have adopted that approach for nearly all patients now,” said Wellstar Hematologist and Oncologist Dr. John French. “We are seeing that if you do that approach, it’s safe, more patients are able to complete all the therapy lines, and we are noticing an increase in pathologic complete response rates.”
Pathologic complete response describes the absence of any detectable cancer cells in a tissue sample following a particular treatment. It refers to the absence of cancer cells in the area of the body where the tumor was originally located, as well as anywhere the cancer may have spread.
Some patients at Wellstar don’t require surgery at all.
“There have been recent studies of a subgroup of patients who are treated pre-surgery through chemotherapy, immunotherapy and radiation and they are seeing great responses,” Dr. Shroff said.
The care team continues to monitor these patients for any signs of cancer.
“We're excited to offer this different pathway for patients,” Dr. Shroff said.
Immunotherapy is based on the concept that a patient’s own immune system can fight their cancer.
When given, immunotherapy drugs wake up the patient’s own immune system to recognize and fight the cancer. People with colorectal cancer are screened for four proteins that help with DNA repair. If these proteins are missing or mutated, the patient is more likely to respond to immunotherapy.
While immunotherapy has been groundbreaking in the treatment of stage 4 colorectal cancer, only about 15% of patients are found to be eligible for the treatment based on their protein screenings, Dr. French noted.
If you are interested in immunotherapy, ask your clinician about your care options.
Wellstar Kennestone Regional Medical Center has received accreditation from the National Accreditation Program for Rectal Cancer (NAPRC), a quality program of the American College of Surgeons.
To achieve voluntary NAPRC accreditation, a rectal cancer center must demonstrate compliance with the NAPRC standards that address program management, clinical services and quality improvement for patients. Centers are required to establish a multidisciplinary rectal cancer team that includes clinical representatives from surgery, pathology, radiology, radiation oncology and medical oncology.

Hand Surgery: Precision & Compassion
Dr. Justin Kunes, Wellstar pediatric orthopedic and hand surgeon
Hand surgery is a unique and intricate field that combines the precision of microsurgery with the compassion required to treat patients of all ages. My journey into this specialized area of medicine comes from a deep passion for helping individuals regain function and improve their quality of life. This article explores my dedication to pediatric hand surgery and minimally invasive adult hand surgery, including arthroscopy and ultrasound-guided procedures such as carpal tunnel and trigger finger release.
The Beginnings of a Passion
From an early age, I was fascinated by the complexity of machines, computers and tools. Until high school, I was convinced that I should become an engineer. However, in the last month of high school I shadowed an orthopedic surgeon and told myself, “I’ll go to medical school if I can do that!” During my medical training, I was fortunate to be able to help many patients in the emergency department to return to their lives and work by treating their hand injuries. I became enamored with the hand’s intricate network of bones, tendons, nerves and muscles that allow for an incredible range of motion and dexterity. Also, in treating children during residency, I wanted to learn more about the growing hand and how I could help children gain the most function. This fascination led me to direct my career in medicine toward a particular focus on hand surgery and pediatric orthopedics.
Pediatric Hand Surgery: A Delicate Balance
Pediatric hand surgery is a particularly rewarding aspect of my practice. Children with congenital hand differences or traumatic injuries require specialized care that addresses both their physical and emotional needs. The challenge lies in the delicate balance of performing intricate surgeries on tiny, developing hands while ensuring minimal disruption to their growth and development.
One of the most fulfilling aspects of pediatric hand surgery is witnessing the resilience and adaptability of young patients. Their ability to recover and adapt to new circumstances is truly remarkable. Whether it is correcting a congenital anomaly like syndactyly (webbed fingers) or repairing a traumatic injury, the goal is always to restore function and enable these children to lead active, fulfilling lives. My favorite pediatric hand surgery is the index pollicization, in which I convert the index finger into a thumb for children who are born without a thumb.
Minimally Invasive Techniques: The Future of Hand Surgery
In recent years, minimally invasive techniques have revolutionized the field of hand surgery. These approaches offer many benefits, including reduced pain, faster recovery times and smaller scars. My practice has increasingly incorporated these techniques, particularly arthroscopy and ultrasound-guided procedures, to provide the best possible outcomes for my patients.
Arthroscopy: Precision Through Small Incisions
Arthroscopy is a minimally invasive surgical technique that involves the use of a small camera, called an arthroscope, to visualize the inside of a joint. This allows for precise diagnosis and treatment of various hand conditions without the need for large incisions. In my practice, arthroscopy works well for conditions such as wrist ligament injuries, ganglion cysts and early-stage arthritis.
The advantages of arthroscopy are myriad. Patients experience less postoperative pain, shorter hospital stays and quicker return to daily activities. Additionally, the smaller incisions result in less scarring, which is particularly important for hand surgery, where stiffness can lead to delayed recovery since tissues must stretch to recover.
Ultrasound-Guided Procedures: Real-Time Precision
Ultrasound-guided procedures have also become a cornerstone of my practice. This technique involves using ultrasound imaging to guide the placement of needles or surgical instruments in real-time. It is particularly useful for conditions such as carpal tunnel syndrome and trigger finger, where precise targeting of the affected area is crucial.
For carpal tunnel syndrome, ultrasound guidance allows for accurate placement of the needle during corticosteroid injections or for the release of the transverse carpal ligament. This results in effective symptom relief with minimal discomfort for the patient. Similarly, for trigger finger, ultrasound guidance ensures precise release of the constricted tendon sheath, leading to improved outcomes and faster recovery.
The Human Connection: Building Trust and Empathy
While the technical aspects of hand surgery are undoubtedly important, the human connection is equally vital. Building trust and empathy with my patients is at the core of my practice. Each patient comes with their own unique story, and understanding their concerns and goals is essential for providing personalized care.
In pediatric hand surgery, this often involves working closely with both the child and their family. Explaining the surgical procedure in a way that is understandable and reassuring helps to alleviate anxiety and build confidence in the treatment plan. For adult patients, particularly those undergoing minimally invasive procedures, clear communication about the benefits and expectations of the surgery is crucial for informed decision-making.
Continuing Education and Innovation
The field of hand surgery is constantly evolving, with new techniques and technologies emerging regularly. Staying at the forefront of these advancements is a priority for me. I am committed to continuous education and regularly attend conferences, workshops and training sessions to refine my skills and learn about the latest developments in hand surgery.
Innovation is also a key aspect of my practice. I actively participate in research studies and collaborate with colleagues to explore innovative approaches and improve existing techniques. This commitment to innovation ensures that my patients receive the most advanced and effective treatments available.
Conclusion: A Lifelong Commitment
My passion for pediatric hand surgery and minimally invasive adult hand surgery comes from my desire to make a meaningful difference in the lives of my patients. The ability to restore function, alleviate pain and improve quality of life is incredibly rewarding. As I continue this journey, I remain dedicated to providing compassionate, cutting-edge care to all my patients, young and old.
Hand surgery is more than just a profession for me; it is a lifelong commitment to excellence, empathy and innovation. Each day brings new challenges and opportunities to gain experience and grow, and I am grateful for the privilege of being able to help my patients achieve their best outcomes.

Wellstar Delivers PeopleCare to our Communities
Wellstar is committed to enhancing the health and well-being of every person we serve, every time. While our clinical teams provide expert care at our facilities, our community outreach teams meet our neighbors where they are—in the communities where we live and work.
Wellstar Community Health and Wellstar Center for Health Equity (WCHE) bring PeopleCare everywhere, and the teams have now reached the impressive milestone of over 100,000 engagements with local households to help meet their health needs. WCHE, established in 2019, addresses social determinants of health. These are factors that affect someone’s well-being, such as access to food, housing and transportation.
“This work is driven by Wellstar team members who see beyond Wellstar’s walls,” said Elise Lockamy-Kassim, Wellstar assistant vice president for community health and WCHE.
A patient’s ZIP code, or the area where they live, is the top determinant of their health outcomes, according to Dr. Earl Stewart, Wellstar primary care physician and the health system’s medical director of health equity.
“Do people have access to affordable healthy food options, or in their ZIP code, is it only fast food? Do they have green space where they can walk and exercise? Do they have reasonable access to sustainable employment?” Dr. Stewart said. “In their ZIP code, are we dealing with environmental justice issues where there may be a fossil fuel burning power plant just down the street and there's contamination in their water or food supply?”
WCHE works to ensure everyone can live to their fullest potential and access the care they need, no matter where they’re located.
Shortly after the inception of WCHE, the team faced the challenge of the COVID-19 pandemic. By leveraging relationships with internal partners at Wellstar as well as external community organizations, the team expanded access to vital care and health information.
Programs included walk-up COVID-19 family testing and vaccination, distribution of masks and safety kits to at-risk communities, and dissemination of Spanish-language educational information. Teams administered more than 10,000 COVID-19 vaccines.
Through the Wellstar Congregational Health Network—our partnership with local faith communities—Wellstar made testing, vaccines and accurate health information more accessible to the people we serve by hosting events at places of worship and virtual town halls in collaboration with faith communities.
WCHE has continued partnerships with communities of worship to expand access to behavioral health resources. Wellstar’s Soul Support program, which also uses the Congregational Health Network, provides congregations with behavioral health education and resources like the Question, Persuade, Refer (QPR) suicide prevention workshop. This workshop trains congregation leaders and members to recognize signs of suicide and navigate mental health emergencies. Soul Support has trained more than 500 people to respond to mental health concerns.
Food insecurity and poor nutrition may lead to a higher risk of developing chronic diseases like obesity, hypertension and diabetes. To address this inequity, WCHE has several initiatives to expand access to healthy foods.
“You can tell a patient, 'You have to do better with your diabetes and eat healthy,' but if they don't have access to affordable healthy food options, they're going to get what they can afford,” Dr. Stewart said.
Wellstar Mobile Markets, in partnership with Goodr, bring fresh produce, meat, shelf-stable items, milk and other beverages to partner sites in the communities Wellstar serves. At the mobile markets, a benefit specialist from Wholesome Wave Georgia, another nonprofit increasing access to healthy foods, helps connect families with additional resources.
The Food as Medicine program, a collaboration with Feeding the Valley Food Bank, is another program combating food insecurity. Primary care patients in the LaGrange area are screened for food insecurity concerns, then if needed, connected with a meal program tailored to their health needs. Participants receive 10 healthy, prepared meals each week for 90 days. They also gain access to Cooking Matters classes held at Wellstar West Georgia’s Enoch Callaway Cancer Center, where they can learn to shop for and cook healthy meals on a budget.
While Wellstar provides comprehensive care at its own facilities, we also know the power in partnership. By teaming with other community clinics and nonprofits, we can have a greater impact and reach more people across our service area. Partner clinics within the Wellstar Community Clinic Network receive a variety of benefits from Wellstar partnership, including resource advocacy, reduced-cost lab and imaging services for patients, and community benefit programs.
“We aim to connect individuals—whether they’re insured or not—with a trusted healthcare provider, which may be a community clinic that is in partnership with Wellstar,” Lockamy-Kassim said.
WCHE is also expanding access to telehealth services so people can get care wherever they are. A partnership between Wellstar, Family Life Restoration Center in Mableton and Giving Health, a Georgia-based telemedicine provider, provides 24/7 access to primary care clinicians and mental health counselors. Over one year as a participant in Wellstar’s Community Transformation Program, Giving Health enrolled over 600 new patients, conducted over 850 telehealth visits and addressed over 250 social determinants of health needs through referrals. More than 450 patients reported accessing care they would have simply gone without had a telehealth option not been available.
WCHE has also facilitated more than 2,500 community-based cancer screenings. One example of these efforts is the ColoCare Connect Program, which aims to improve access to colorectal cancer education and screenings by providing fecal immunochemical tests to community clinics serving high-risk populations.
Through additional partnerships with Wellstar Cancer Care and Wellstar Gastroenterology, WCHE also presented the Nourish to Flourish series to further educate community members about screenings. Participants walked away with educational resources, fresh groceries and a slow cooker to promote healthy eating habits at home.
Live to the Beat. Powered by Wellstar. is an initiative of WCHE and Wellstar’s cardiovascular care team, in collaboration with the American Heart Association, the CDC Foundation and Million Hearts. Participants meet monthly with a Wellstar Community Health team member to have their blood pressure checked and discuss ways to keep their heart healthy, such as proper nutrition, exercise and caring for mental health.
Wellstar’s partners in the initiative are now looking at ways to bring the program to other communities nationwide to expand access to heart care and education.
“We want WCHE to be not only a beacon for health equity done right in the areas Wellstar serves in the state of Georgia,” Lockamy-Kassim said. “We want our work to be modeled across the U.S. as a way to ensure all people have access to the care they need to live their best life.”
If your organization or congregation is interested in partnering with Wellstar Community Health or WCHE, email [email protected] or [email protected].
To get connected with no-cost or low-cost resources, including food, housing and transit needs, visit wellstar.findhelp.com.

Wellstar Cobb First at Wellstar to Offer Latest Advancement in Robotic Surgery


The 5 Dos and Don’ts of Managing Joint Health

Hip & Knee Replacement Considerations
Dr. Eric Kiskaddon, Wellstar orthopedic surgeon
There are more than 1 million hip and knee replacement surgeries performed in the United States each year, primarily for patients experiencing debilitating arthritis pain in those joints. That number is expected to grow considerably as the population ages and looks to maintain an active lifestyle. However, despite being one of the most common elective orthopedic procedures performed today, many patients whose quality of life could benefit from such a surgery are often hesitant because they know friends or family members who have had a total joint replacement with a poor outcome. That is why helping patients understand what to expect during and after surgery, and how to optimize their health prior to the surgery, is crucial to any successful joint replacement procedure.
Before undergoing total joint replacement surgery, it is vital for a patient to be as medically optimized and strong as possible. This means working on range of motion exercises for the affected joint and doing light strengthening exercises on a consistent basis in order to increase joint and muscle movement, reduce stiffness and pain, and maintain flexibility. In addition, encouraging patients to practice good diabetic control, stop the use of nicotine products and optimize their weight by making healthy lifestyle choices also helps to reduce the risk of infection after surgery and improve patient satisfaction and recovery. These are incredibly important factors for patients to discuss with their surgeon when considering joint replacement surgery in order to increase the likelihood of having a complication-free surgery.
Prior to surgery, patients should be able to meet with their surgeon and care team to discuss the procedure in detail and have all their questions answered regarding post-operative complications, mobility, pain management and the impact on their lifestyle and daily activities. Finding a surgeon who prioritizes sitting with patients and taking the time to answer their questions ahead of surgery is imperative. Further, meeting with the anesthesia care team and participating in instructional classes related to hip and knee replacement helps patients feel at ease with undergoing the surgery and managing the recovery process.
Patients are often concerned about the hospital stay, including what will happen the day of surgery and after the surgery. Thanks to advancements in surgical techniques, many hip and knee replacement surgeries can now be performed as outpatient procedures. This allows patients to go home on the same day as their surgery, often with the support of home health and physical therapy services. For those who have more complex medical problems, an overnight stay is typically recommended.
Pain control techniques have vastly improved in recent years, and surgeons and anesthesiologists now work together to use a variety of methods to treat patients’ pain. These include nerve blocks, medications infiltrated around the actual hip or knee joint and medications administered after surgery that target multiple pain receptors and help keep pain manageable. At Wellstar Orthopedics & Sports Medicine, we ensure that patients are up and walking within a couple of hours of surgery with an assistive device. Most patients no longer require a blood transfusion due to better anesthesia techniques as well as medications that now slow blood loss during surgery, which also contributes to a faster recovery.
After surgery, patients can expect to need a walker for anywhere from a few days to several weeks. Most patients don’t need an assistive device by three to four weeks after surgery, but this does vary. Patients often return to driving around three to four weeks after surgery. In my practice, we typically close the incision with sutures underneath the skin, eliminating the need for patients to return to the office for suture or staple removal. In addition, the bandages we use are waterproof, making it easy for patients to shower after surgery. The total recovery time following joint replacement surgery is usually two to three months. Most patients benefit from attending weekly physical therapy sessions during this time to assist with regaining full joint range of motion, increasing strength throughout the lower extremity and regaining independence with functional activities such as ascending and descending stairs and getting up from a couch.
For those who are interested in doing their homework prior to surgery, there are excellent resources available to patients on both the American Academy of Orthopedic Surgery and American Association of Hip and Knee Surgeons websites. But the most important step for patients as they prepare for joint replacement surgery is to consider choosing a surgeon who has additional fellowship training in hip and knee replacement, is willing to answer their questions and proactively share what to expect, and who they ultimately trust to perform the surgery. Taking the time to find a surgical team that is committed to enhancing patients’ well-being and helping them achieve the best possible outcome will increase the odds of a successful joint replacement.

Empowering Communities: A Heart Health Collaboration with the American Heart Association and Wellstar Congregational Health Network
In today's fast-paced world, maintaining good heart health has never been more important. The collaboration between the American Heart Association and the Wellstar Congregational Health Network (CHN) is making meaningful progress in empowering four local churches to prioritize heart health. Wellstar CHN identified these partner churches in Metro Atlanta as facing significant gaps in the tools needed to support the well-being of their congregations. This initiative aims to increase awareness about high blood pressure, provide necessary tools for monitoring heart health, and save lives by ensuring these churches have CPR-trained staff and are equipped with devices like automated external defibrillators (AEDs).
Collaborating to achieve community well-being
The American Heart Association has long been at the forefront of cardiovascular health education, advocacy and research. By joining forces with Wellstar, which is dedicated to improving health and wellness in Georgia, the organization is expanding its reach into local communities.
The Wellstar CHN, which works closely with churches and faith-based organizations, has been committed to serving congregants’ physical, mental, and spiritual well-being for over 20 years. This collaboration represents an impactful move toward offering practical solutions to help address heart disease, the leading cause of death in the U.S.
Making early detection a priority
A key initiative under this collaboration is the establishment of blood pressure monitoring stations within the churches. These stations are designed to provide easy access for community members to check their blood pressure regularly. High blood pressure, often called the "silent killer," can lead to serious health complications such as heart attacks, strokes, and kidney failure if left undiagnosed and untreated.
By placing blood pressure monitoring stations in church spaces, people are encouraged to regularly monitor their health in a familiar, supportive environment. The program also provides educational materials on how to maintain healthy blood pressure levels, empowering individuals with the knowledge they need to act early.
These stations serve as a gateway to better health, helping people detect high blood pressure and seek medical advice sooner.
Providing access to lifesaving tools in churches
Another vital part of this collaboration is the provision of AEDs to participating churches. An AED is a portable device that can deliver an electric shock to someone experiencing sudden cardiac arrest (SCA), which can be fatal without prompt intervention.
Placing AEDs in churches means congregants and visitors have access to lifesaving tools in a cardiac emergency. These devices are easy to use, with step-by-step instructions, and they can dramatically increase the chances of survival if used quickly.
The goal is to equip churches with not just AEDs, but also the training to use them effectively. The American Heart Association provides training for church staff, volunteers and congregants so they can act confidently in the event of a cardiac emergency. For many people, churches serve as central gathering points within a community, making them ideal locations for AEDs to be readily available.
Building stronger communities through heart health
The American Heart Association and Wellstar CHN partnership is about more than providing tools—it is about building a healthier, more resilient community. By focusing on heart health, these initiatives aim to reduce the risks of heart disease and cardiac emergencies. They also foster a culture of wellness, where faith-based organizations can be hubs for health education and support.
Churches play a significant role in their communities, offering spiritual guidance and physical and emotional support. By embracing these heart health initiatives, they become even more integral in shaping healthy futures for everyone who walks through their doors.
Looking ahead to a healthier future
This joint effort between the American Heart Association and the Wellstar CHN is a shining example of how local groups can work together to make a tangible impact. By providing blood pressure monitoring stations, AEDs, and ongoing health education, the organizations are helping to save lives, prevent heart disease, and empower communities to take proactive steps toward better health.
As heart disease continues to affect millions of individuals each year, collaborations like these are crucial in shifting the narrative from reactive to proactive health care. Together, we can create a healthier future for ourselves, our families and our communities.
A big thank you to the churches below for empowering their members by hosting these heart health educational programs and providing the tools needed to improve their health and well-being. Your work in the community is inspiring.

Urology and You: A Doctor Answers Sensitive Questions


Wellstar Accelerates Training Next Generation of Caregivers

Limb Lengthening and Deformity Correction
Dr. Stephen Becher, Wellstar orthopedic surgeon
The history of orthopedic surgery is mankind’s attempt to make straight that which is crooked. The advent of anesthesia made it possible to use surgery to break bones and re-align them without undue pain. But the art of correcting deformities caused by abnormal growth or trauma has taken hundreds of years to advance to its current form. The most important observation—made incidentally by multiple surgeons, but most famously by Gavrill Ilizarov during the 1950s in the Soviet Union—was that a broken bone, if pulled apart with appropriate timing and stress, can form new bone.
This discovery came with years of painstaking research and trial and error in order to effect techniques that would allow for gradual correction of limbs that were bent, short or otherwise deformed. Initially, external fixator apparatus were used to manually manipulate the bone with daily turns of a crank, which involved mathematical calculations and equations that lacked precision when applied to the individual case. Gradually, these methods evolved to incorporate automation, modern computing and more biologically friendly surgical techniques. Newer devices allowed for the distraction pressure to be applied inside the body rather than outside in select cases, making the process of correcting limb alignment problems less cumbersome to patients.
Limb lengthening and deformity correction has always been a powerful yet technically difficult procedure, making it a smaller and less-utilized area of orthopedics. But the ability to correct errors of genetics or nutrition or deformities from trauma or infection is nothing short of magical—and magic requires study, practice and dedication to perform correctly. Distraction osteogenesis techniques are often applied to problems that are intractable by other, more commonplace means. Practitioners of the art enjoy the unique challenges presented and the potential to affect patients’ lives for the better. It is not always easy or simple, but the reward of helping others is the driving force behind the effort.
Subspecialty training in the area of limb lengthening and deformity correction is now available in the United States at several centers. A subspecialty society, the Limb Lengthening and Reconstructive Society (LLRS) provides educational opportunities with meetings and traveling fellowships. Orthopedic surgeons who have taken advantage of the society’s training and membership are often those most committed to learning the art and science of limb deformity correction. The Orthopedic Trauma team at Wellstar Kennestone Regional Medical Center includes physicians who have undergone this training and enjoy being a resource for patients and the orthopedic surgery community at large when it comes to limb deformities, difficult malunions or nonunions, infections requiring bone transport and other complicated cases. At Wellstar, modern techniques using both external fixation and computer-assisted guidance allow limb deformity correction to occur with minimal patient discomfort or manipulation of complex apparatus. Internal techniques are also used, including lengthening nails that allow the limb to be lengthened or straightened, replacing the need for a cumbersome external fixator.
Complications from orthopedic surgery often require unique solutions. Infected joint replacements, infected bone that requires removal (osteomyelitis) and bone loss resulting from severe trauma are all conditions that can be treated with modern limb lengthening and deformity correction techniques. The physicians specializing in these techniques are happy to consult over the phone with other physicians who need assistance in these complex situations, as well as share their expertise with patients during in-person consultations. The desire to provide world-class healthcare defines the individuals who make up the Orthopedic Trauma division at Wellstar. There are few orthopedic problems that they are not eager to try to solve, and they are always willing to learn the newest techniques in order to improve the lives of those who believed their cause was lost.

What’s Got You Sick?
Antibiotics save lives by effectively treating bacterial infections, but they aren’t effective against viral infections. At Wellstar Primary Care and Wellstar Urgent Care, our expert clinicians will evaluate your symptoms and tailor a care plan for your condition, including a prescription for the appropriate medication if needed.
Viral infections like colds, flu, respiratory syncytial virus (RSV) or COVID-19 may require antiviral medications. There is no antiviral medication to treat norovirus, but it’s recommended that you stay hydrated and use anti-diarrheal or anti-nausea medication if needed. Most people with norovirus will feel better in about one to three days.
If you’re diagnosed with an infection that has been caused by bacteria, such as strep throat or a urinary tract infection, an antibiotic can clear up the infection and help you feel better. Some bacterial infections can resolve without antibiotics, and your care team will work with you to determine your treatment plan.
While antibiotics are effective in treating bacterial infections, it’s important that you don’t take them if you don’t need them.
“Unnecessary antibiotic use can cause your body to build up resistance to them, which means they won’t be as effective when you do get an infection,” said Wellstar Urgent Care Physician Dr. William Broyles.
If you think you may have a bacterial or viral infection, contact your primary care clinician or visit an urgent care location near you so our team can help you start feeling better. Learn more about the types of care available at Wellstar and which may be right for your condition.


Wellstar Center for Health Equity Awards Grant Funding to Eight Local Organizations to Improve Patient Access and Care Through Technology
Everyone deserves high-quality healthcare and social services—no matter where they live. But people in many communities simply don’t have access. At Wellstar Center for Health Equity, we believe technology can be part of the solution. That’s why we created the Community Transformation Program (CTP) in 2020.
Each year, CTP invites local organizations to request support for a new or existing tech-based initiative that addresses health disparities in our communities. The winners receive a $10,000 grant to help fund their initiative. They also receive capacity-building support through:
This holistic approach ensures each organization’s tech initiative thrives. To date, CTP has touched over 18,000 lives in vulnerable populations across Metro Atlanta and beyond.
Meet our fifth cohort of partner organizations
This year, CTP chose eight organizations to be part of our growing network of difference-makers. These partners exemplify the diverse approaches needed to tackle our region’s complex challenges.
Each organization is in a unique position to make a profound impact. They include:
.jpg?la=en-us&h=300&w=600&rev=d03cbe6dd3c84cd280a26cf59efa223e)
A history of success
The organizations participating in CTP make a difference—sometimes in unexpected ways. Last year, Bethesda Community Clinic transitioned from being a brick-and-mortar practice to a fully mobile healthcare model. The clinic used CTP funds to equip their mobile health vehicle with telehealth kits. Patients sit inside the clinic’s vehicle, and doctors meet with them virtually. The doctors use the kits to conduct a full health assessment. This new model enables many more patients to receive care they otherwise may not have access to.
The Georgia Bureau of Investigation learned about the clinic’s care model and enlisted them to bring these telehealth kits into hotels. This model provides care to victims of human trafficking and serves as a lifeline for rescue. The FBI is now exploring this model as a standard nationwide.
A shared vision for a healthier Georgia
This year’s CTP partners represent another step toward a Georgia where every individual can achieve their full potential. Wellstar is transforming lives by empowering our partners to address inequities with innovative, community-focused solutions. Success stories like this demonstrate that when we work together, there’s no limit to what we can do.
Learn more about Wellstar Center for Health Equity and our initiatives

John Kerndl Joins Wellstar as Executive Vice President and Chief Financial Officer
John Kerndl has joined Wellstar Health System as executive vice president and chief financial officer. He will provide strong financial stewardship as the nonprofit health system continues to grow and expand access to care for Georgians across the state.
“John’s wealth of experience in healthcare financial leadership will allow us to invest in the technologies, resources, services and, most importantly, the people that enable us to deliver world-class care to the patients and communities we serve,” said Candice L. Saunders, President and CEO of Wellstar Health System.
Over his 30-year career, John has held senior executive positions in healthcare organizations across the nation. Most recently, he served as chief financial officer for Traditions Health, a $350M hospice and home health system consisting of 113 locations in 18 states. In this role, he oversaw all financial planning and analysis activity, treasury, central intake, revenue cycle, information technology and security, supply chain, risk and insurance, accounting, and managed care, among other responsibilities.
John previously worked as the EVP and chief financial officer for Beth Israel Lahey Health, a Boston-based health system consisting of 10 acute care campuses, 4,000 physicians and 35,000 team members. He also served as EVP and chief financial officer for Beaumont Health System, the largest care provider in Michigan.
John received his Bachelor of Business Administration from Georgia State University and his Master of Business Administration from the University of Chicago.

RalphCare
Douglasville resident Ralph Aiken experienced a motorcycle accident in April of 2022. The 82-year-old was thrown 10 feet in the air and another 20 feet down into a hole, suffering a broken left leg below the knee. As part of his healing, he worked closely with Dawnette Waters, Wellstar physical therapist, to rebuild muscle in the injured leg.
One fateful day while at therapy, the U.S. Army veteran experienced cardiac arrest. Due to the quick actions of Waters and members of the adjoining Wellstar Outpatient Cardiac Rehab center, EMTs were able to revive Aiken and rush him to Wellstar Douglas Medical Center, where Wellstar Interventional Cardiologist Dr. Cheryl Robertson found the cause of the cardiac event—95% blockage of an artery. Dr. Robertson immediately inserted an atrial stent. Ralph has felt healthy since the surgery and is grateful for the team at Wellstar who saved his life.
“Wellstar is very well-operated and efficient, and the doctors, the nurses and the therapists are top-notch. I wouldn't be here if it hadn't been for the therapy staff,” Ralph said.
Ralph enthusiastically reunited with his entire care team at Wellstar. Smiles and hugs were the mood of the day, as each recalled the events that led to him still being with us to enjoy life.
Today, Ralph continues to exercise and is proud of his active lifestyle, despite his age. “Look at me. How many 82-year-old men have a 34-inch waist and an arm muscle like that?” he said.

LatoyaCare
In Latoya Jordan’s world, “family comes first” is more than a mantra. It’s a way of life, as a wife and mother raising four fearless daughters.
While living in New York, Latoya learned how to be strong, determined and face challenges head-on—lessons she now instills in her own children. These traits proved useful when the Jordans resettled in the South at the start of the COVID-19 pandemic.
But between the big move and preparing the girls for virtual school, Latoya found it difficult to squeeze in any "me time." Caring for her little ones often led to putting her own health last.
However, with two different heart conditions—a murmur and high blood pressure—the mother needed tailored care to live her fullest life.
With the help of Wellstar, Latoya got expert care to stay heart healthy, right in her new neighborhood. But beyond that, she found a trusted healthcare family that had her covered when it came to her well-being.

Wellstar MCG Health to Exhibit Local Black Artists
Wellstar MCG Health Medical Center will celebrate Black History Month with an art exhibition showcasing Black artists from the Augusta area February 26 from 9 AM to 4 PM in the Professional Building Lobby.
The Beauty of Black Art, sponsored in partnership with the Lucy Craft Laney Museum of Black History and the Greater Augusta Arts Council, will be free and open to the public. Wellstar commemorates Black History Month as part of the health system’s dedication to diversity, equity, inclusion and belonging (DEIB).
“When we lead with respect and embed equity at every level of our organization, we improve health outcomes, job satisfaction and quality of life for our patients, team members and communities we serve,” said Le Joyce Naylor, Wellstar senior vice president and chief diversity, equity and inclusion officer. “It declares, ‘I see you,’ and everyone deserves to experience this profound sense of belonging.”
Wellstar provides diversity, equity, inclusion and belonging training for team members at every level of the organization to cultivate an environment where everyone is valued, welcomed and heard.
“Our DEIB program is threaded throughout the fabric of our organization and is evident through the work and efforts of our 30,000 plus team members from across the health system,” said Wellstar President & CEO Candice L. Saunders. “We remain steadfast in our commitment to six key areas of focus as we move forward—advancing workforce diversity, creating a culture of inclusion, building cultural competence, promoting health equity, improving community engagement and enhancing supplier diversity.”
At Wellstar, team members can join business resource groups to connect with colleagues from similar backgrounds or with shared experiences. The February 26 event is sponsored by the Women of Color in Leadership and Men of Color in Leadership business resource groups at Wellstar MCG Health. Through business resource groups, events, team member training and other initiatives, Wellstar creates spaces for conversations about diversity, equity, inclusion and belonging and supports team members, patients and community members.
“Wellstar focuses on listening to every voice, creating an inclusive workplace and engaging the community,” said Bernard Roberson, Wellstar MCG Health DEIB manager.
Artists highlighted at The Beauty of Black Art include:

Growing Partnership With Ser Familia Serves Latino Community
At Wellstar, our doors are open to everyone. Whether it’s an individual with a life-threatening health crisis or a family looking for a new primary care provider, we’re here to help.
Sometimes, it’s not enough to welcome people in. We also need to go out into the communities we serve to meet people where they live, work and play to ensure they receive high-quality care.
To meet more of our neighbors where they are, we partner with organizations like Ser Familia. Founded in 2001 in the Metro Atlanta area, Ser Familia equips Latino families with the tools, resources and skills they need to thrive. Ser Familia’s extensive wraparound services include support groups, family workshops, mental health counseling and educational programs. In recent years, Ser Familia has expanded its footprint with new locations across Georgia and Puerto Rico.
The power of working together
Wellstar Center for Health Equity has a long-standing relationship with Ser Familia. For example, Wellstar provides grant funding so Ser Familia can employ Spanish-speaking community health professionals. These professionals have a unique ability to provide health information where it is needed most. They can:
Also, Wellstar physicians participate in Ser Familia community health outreach programs serving Latino communities.
Excitement about a planned health clinic
In the near future, Ser Familia plans to open a health clinic with the support of Someone Cares, Inc. of Marietta, another Wellstar partner. The clinic will provide comprehensive primary care, including health, education and preventive services. Nurse practitioners will see patients at the clinic under the guidance of physicians at Someone Cares. And, if patients need care that Ser Familia does not offer, the nurse practitioners can refer them to a Someone Cares provider.
When organizations like Wellstar and Ser Familia work together, we accomplish far more in our communities than we could separately by making better use of our resources. Most importantly, we help people find the care they need where they need it.
Learn more about Wellstar Center for Health Equity.

Clubfoot & The Ponseti Method
When a health condition affects your child’s quality of life or keeps them from doing what they love, your family can rely on Wellstar Pediatric Orthopedics to provide compassionate, comprehensive care. As your child grows, so do their bones and joints, and they need specialized expertise—whether they have broken a bone on the playground or have an orthopedic condition present at birth.
Approximately one to four of every 1,000 babies are born with clubfoot, a condition in which one or both feet are turned inward and downward. The deformity affects a baby’s bones, muscles, tendons and blood vessels. Fifty percent of children born with clubfoot have bilateral clubfoot, which means both feet are affected. While the condition is readily visible at birth, many times the deformity is detected on prenatal ultrasounds, allowing weeks or months for the parents to prepare for the expected treatment. Most children born with clubfoot do not have a parent with the condition. Risk factors include male biological sex (boys are born with clubfoot twice as often as girls), genetic syndromes, neuromuscular disorders, birth defects and a breach birth.
Clubfoot is not a painful deformity, and most children who are treated early go on to live active and healthy lives. However, untreated clubfoot will not improve on its own. As the child gets older, they will have a challenging time walking on their own.
Our team of experts understands that babies born with clubfoot may also have associated conditions such as hip dysplasia or torticollis. Therefore, we thoroughly examine your child to ensure all their needs are addressed.
There are two types of clubfoot: idiopathic and syndromic. Idiopathic clubfoot is the most common, and although we suspect there is a genetic component, we still do not know what causes it. Idiopathic clubfoot is not related to any other medical issues. Alternatively, syndromic clubfoot is more severe, difficult to treat and occurs as part of a larger medical condition. If your child is diagnosed with syndromic clubfoot, our team will coordinate with multiple specialists to tailor care to your child’s specific needs.
Treatment for clubfoot usually begins when the child is a few weeks old. The goal is to correct the foot position before they learn to walk, thus minimizing the impact of the condition on the child’s long-term mobility. This is done through a series of casts designed to help the foot grow more normally.
“We use the Ponseti method, a nonsurgical approach that uses a series of casts and then bracing to gradually reposition the foot,” said Wellstar Pediatric Orthopedic Surgeon Dr. Michael Priola.
With this method, the doctor stretches out and repositions your child’s foot, then places it into a long leg cast to hold their foot in the appropriate position. Long leg casts are used to prevent the cast from slipping off the child’s leg. The cast is removed in about a week, the doctor again repositions the foot, and a new long leg cast is placed. This method continues until your child’s foot is moved into the correct position. Many of our providers utilize soft cast material, which has a higher parent satisfaction rating than the typical plaster material. Following casting, about 90% of patients require a minor procedure that releases the Achilles tendon, allowing further correction of the foot deformity. A final cast is then worn for an additional three weeks before being removed in the clinic.
Once corrected, a brace is used to maintain the alignment over several years. For the first three months after completion of the casting, the brace is worn for about 22 to 23 hours per day. After that, children typically progress to wearing the brace for naps and nighttime only (about 15 to 16 hours per day). This allows your child to learn to crawl, walk, run and play in the normal developmental time frame. Families should continue with this bracing schedule until the patient is 4 years old to prevent the condition from returning.
“This method boasts a high success rate and avoids the need for extensive surgery,” Dr. Priola said. “Sometimes in more severe cases (including a rigid clubfoot) or if the Ponseti method fails, more extensive surgical intervention may be considered.” These surgeries include a complete posteromedial release of soft tissues, tendon lengthening and realignment of joints.
With timely and appropriate treatment, children born with clubfoot can experience significant improvement, leading to a bright future that is not limited by the condition.
If your child is affected by clubfoot, our pediatric orthopedic specialists are here to provide expert care for this condition and support them at every step of treatment. We understand that medical procedures can be stressful for both children and their families. Your child’s care team will personalize treatment to their individual needs and answer any questions you have about clubfoot or managing the condition.
To book an appointment with a pediatric orthopedic surgeon, visit wellstar.org/pedsortho or call (404) 321-9900.

How one fulfillment team provides Wellstar patients with compassionate care
Caring for people is what Wellstar is all about. It’s easy to see the impact made by physicians, nurses and other clinical team members. But many others work beyond hospital walls to make compassionate care possible. One place where you can find them is Wellstar’s Consolidated Service Center—known to the team as the CSC. The 175,000-square-foot facility operates as a same-day delivery retailer, fulfilling orders for everything from medical supplies to printed materials for patients. The operation supplies Wellstar’s hospitals, health parks and other patient care locations.
The foundation for the important work done by one CSC team started more than two decades ago, when Wellstar partnered with Tommy Nobis Center.
“The Tommy Nobis Center’s mission is empowering people through employment,” said Darren Hazeur, Tommy Nobis Center employment site supervisor at Wellstar. “Tommy Nobis Center envisions supportive communities where people with disabilities are afforded the opportunity to work. Our focus is to educate, train and employ people with disabilities so they can truly blossom.

Save Lives, Don’t Drive—When to Call 911
When a stroke or heart attack strikes, every second matters. Saving time could mean saving a life, and it’s crucial that medical treatment starts right away. That’s why in the case of a heart attack or stroke, call 911 immediately—don’t drive yourself or another person to the hospital.
Emergency Medical Service crews are trained to start life-saving treatment on the way to the hospital, minimizing damage to your heart or brain. They can also conduct and interpret electrocardiograms to diagnose a heart attack in the ambulance.
You also don’t want to drive if you are experiencing a heart attack or stroke yourself because your condition could worsen on the way to the emergency department and impact your ability to stay safe on the road.
“If you're having an emergency, which could be severe abdominal pain, chest pain, shortness of breath, weakness that you can't really explain, you've got to call 911,” said Dr. Ed Malcom, an emergency medicine physician at Wellstar North Fulton Medical Center. “The ambulance and the EMS services will get you to the emergency department in a safe way, and we will get you taken care of.”
When a patient has a heart attack, ambulance crews communicate with our cardiac team on the way to the hospital, bypassing the emergency department and diverting directly to the cardiac catheterization lab, where our team is ready to restore blood flow to your heart. Calling 911 means reopening the heart artery sooner. And when someone has a stroke, it’s also crucial to take action right away—the sooner you seek treatment, the more brainpower can be saved.
To learn more about how Wellstar treats heart attacks and strokes, visit our heart care and neuro care pages.
Advanced Heart Care Close to Home
When it comes to getting high-quality care for your heart, you can count on Wellstar.
Because we know heart health is an essential part of overall wellness, we offer leading expertise, innovative treatments and compassionate care to protect your cardiovascular health.
From heart attacks and rehabilitation to cardiac surgery and psychological support, your heart is in expert hands at Wellstar.
With the largest network of certified Emergency Cardiac Care Centers (ECCC) in Georgia, Wellstar ensures world-class heart care is never far away.
Our cardiovascular experts are ready to treat patients at the first signs of a heart attack. We use high-tech equipment—including electrocardiograms (EKG), chest X-rays and cardiac catheterization—to diagnose heart attacks quickly.
Getting the right care can minimize or even prevent heart damage. That’s why Wellstar relies on the most advanced treatments, such as Shockwave technology, medicines and life-saving cardiac surgery, to effectively prevent and treat heart attacks as fast as possible.
Wellstar Kennestone Regional Medical Center has a cardiac hybrid operating room, bringing a catheterization lab and surgery suite together in one place. With catheter-based procedures, our interventional cardiologists can provide expert, minimally invasive heart attack care.
We also perform structural heart procedures, including valve repairs and replacements, along with cardiac surgery and electrophysiology procedures that can determine the cause of heart rhythm problems.
At Wellstar, we don’t just treat heart conditions when they happen. Our providers also offer world-class preventative care, helping people like Latoya Jordan catch chronic conditions—such as high blood pressure—at the very start.
The Wellstar Comprehensive Aortic Program provides treatment for people with emergency and non-emergency diseases of the aorta. We offer cutting-edge procedures and devices to diagnose, monitor and repair all types of aneurysms. From screening to treatment, our team uses a coordinated approach to care which includes comprehensive diagnostic testing. When urgent care is warranted, we can treat aortic emergencies quickly.
If an on-going heart condition, such as atrial fibrillation (AFib), is keeping you down, Wellstar has a team of experts who can help.
When Frank Ryan’s heart had trouble keeping pace and kept him from playing the tuba, he felt off-beat in everyday life. After getting specialized care at Wellstar, he’s back in the band again.
Wellstar Cardiac Electrophysiologist Dr. Narendra Kanuru shared state-of-the-art treatments available for heart rhythm disorders.
“Along with advanced medical therapies, we have numerous interventional or surgical therapies, including pacemakers, defibrillators and other advanced cardiac devices as well as cardiac catheter ablation,” Dr. Kanuru said.
Cardiac catheter ablation is a non-surgical procedure available at Wellstar that helps restore a regular heart rhythm by blocking abnormal electrical signals.
With the latest advances in electrophysiology at Wellstar, we’re keeping hearts going strong.
Wellstar also provides expert care for people with congestive heart failure like Bow Matthews. The husband and father-of-two found support from our Heart Failure Academy and learned how to take care of his well-being for the long haul.
To help prevent heart failure flare-ups, Wellstar offers a remote heart monitoring technology that provides real-time health information to our providers.
“With heart failure, as with all health issues, it’s best to take preventative action and stop problems from occurring,” said Dr. Hans Lee, medical director for the Wellstar congestive heart failure program. “Monitoring your heart health and staying in touch with your cardiologist can help keep you out of the hospital and keep your heart in shape.”
For those whose hearts need extra assistance like Mike Clements, a left ventricular assistance device (LVAD) can be a game-changer. An LVAD is a battery-powered pump that is surgically implanted to help the heart more effectively pump blood.
"An LVAD gives patients with severe heart failure the opportunity to get their lives back,” said Dr. Brian Howard, medical director of the advanced heart failure and LVAD program at Wellstar Kennestone. “These life-saving devices are powerful enough to take over for the failing heart. They allow patients to enjoy life with their loved ones as they await a heart transplant, and in some cases, they even serve as an alternate to a heart transplant entirely.”
At the Heart Failure Clinic at Wellstar Cobb Medical Center and the Advanced Heart Failure Program at Wellstar Kennestone, trained experts provide specialized care for those with heart failure and LVAD implants, helping to improve quality of life.
After Mike received his LVAD implant, he was able to walk his daughter down the aisle at her wedding. Thanks to advanced technology available at Wellstar, patients with heart failure can keep doing what matters most.
Wellstar has dedicated resources to help people with cardiac conditions find support.
Following a medical event like a heart attack or other serious cardiac problem, Wellstar offers cardiac rehabilitation to get people back on track.
Cardiac rehabilitation is a medically monitored program that provides education, support and lifestyle modifications. Our team helps you learn heart-healthy behaviors and lower your risk for future heart issues.
However, we understand health journeys aren’t just about physical healing. Dealing with heart issues can also cause many difficult mental health challenges, including anxiety and depression.
“At Wellstar, we wanted to build out a program just for our cardiovascular patients because behavioral health and cardiac health are really closely connected,” said Dr. Shawn Coyne, Wellstar director of health psychology and cardiac psychologist. “In fact, cardiac patients are three times more likely to be depressed than the general population.”
After living with three chronic heart conditions for years, John Petrick found solace in meeting with a Wellstar cardiac psychologist. Now, he’s learned new coping skills and how to prioritize his mental well-being.
With support services at the ready, patients with complex conditions can better understand themselves and their overall health.
No matter what your cardiovascular concerns may be, Wellstar is dedicated to helping people with heart conditions live life to the fullest.
Learn more about how Wellstar is protecting heart health in Georgia, and how you can take control of your cardiovascular health.

Wellstar MCG Health Medical Center Provides Hospital-Level Care in Patients’ Homes

Coale Peace Named 2025 National Champion for the Children’s Miracle Network

Together, We Can Slow the Spread of Illness in Our Community
Saving lives and fighting illness happens every day at our Wellstar healthcare facilities, but we can all do our part to keep ourselves and our loved ones healthy. When you focus on the wellness of your world—yourself, family and friends—you can help stop the spread of disease in our community.
Proper hand hygiene can reduce the spread of illnesses including COVID-19, flu, RSV and norovirus. Bacteria on your hands could increase your chances of getting sick or prolong recovery, so it’s important you wash your hands often.
If you do get sick, you can count on Wellstar for expert care. You have several options for treatment, including pharmacies, a virtual visit, your primary care professional, an urgent care center or an emergency department. Learn more about each type of care and where to go for your health needs at wellstar.org/knowwheretogo.

Wellstar Partners with Feeding the Valley to Improve Food Access and Nutrition
Wellstar Center for Health Equity and Wellstar West Georgia Medical Center have launched the Food as Medicine program. In partnership with Feeding the Valley Food Bank, this initiative supports Wellstar’s strategy to improve food access in high-need communities.
Patients will be screened during primary care visits at offices in the LaGrange area for food insecurity. Clinicians will then connect patients who screen positive for food insecurity to a medically tailored meal program offered by Feeding the Valley.
Participants will receive 10 healthy, prepared meals each week for 90 days. They will also gain access to Cooking Matters classes held at Wellstar West Georgia’s Enoch Callaway Cancer Center, where they will learn to shop for and cook healthy meals on a budget. By equipping patients with practical nutrition knowledge, budget-friendly cooking skills and a three-month supply of healthy meals, Wellstar aims to support people in making lasting, health-boosting changes to their diets and overall well-being. While food insecurity is a concern identified by our Community Health Needs Assessment, diabetes and other diet-related illnesses are also a major threat to our community’s well-being.
Wellstar is increasingly working toward healthy food solutions that address both food access and health. Our efforts with Wellstar Mobile Markets, in partnership with Goodr, and our food rescue initiatives, in collaboration with Goodr and Second Helpings Atlanta, show our commitment to increasing food access.

Make Heart Health Your Habit
It’s impossible to count all the ways your heart supports you in a single day. Whether it’s checking out a new trail, gardening or simply playing with your kids, every beat of your heart helps you do all the activities you enjoy most.
That’s why it’s so vital to take care of your cardiovascular health—and doing so is easier than you might think. According to Wellstar medical experts, consistency is the key.
“To keep your heart in top shape, make gradual changes sustained over a lifetime,” said Dr. Vivek Nautiyal, Wellstar medical director of preventative cardiology. “Investing in your heart health can be as simple as going for a walk after work, trying a healthy recipe or scheduling that wellness exam you may have been delaying.”
Remember to start small—by just taking a few simple steps, you can keep your heart going strong.
Getting a heart screening is a great way to care for your cardiac health. The Know Your Heart screening program helps catch potential heart problems early, so you can live life to the fullest. Through this testing, you can learn your risk of heart disease and other serious conditions, such as high blood pressure or high cholesterol.
After the screening, you will receive an individualized health report with all the latest stats about your heart. Our team will go over the results with you one-on-one and recommend lifestyle modifications to help you be the healthiest you.
Call (770) 956-STAR (7827) or visit the Know Your Heart page for more information.
Along with monitoring your overall well-being, your primary care clinician can help catch potential heart problems early.
“At your annual wellness exam, your provider can assess your risk of certain heart conditions, such as heart disease or high blood pressure,” Dr. Nautiyal explained.
Your provider will check the Foundational 4 numbers that are the cornerstone of general wellness and heart health, including:
“Your provider can help create a personalized plan to keep your heart healthy, which may include diet, exercise or other lifestyle modifications,” Dr. Nautiyal shared. “If you need expert cardiovascular care, they can also refer you to a heart specialist right away.”
When it comes to staying ahead of potential health issues, Dr. Nautiyal also shared the importance of being aware of your family history and cardiovascular stats.
“Be sure to know your cholesterol numbers and seek a preventative cardiology consultation if you have a family history of premature heart attacks, coronary disease or stroke—especially at an age below 55 years old,” Dr. Nautiyal said.
Learn more about the advanced heart care services offered at Wellstar.

Loran Wills, 93, Retires from Paulding County Hospital Authority
Keep reading
Make Health Your Habit as a Family

Partner with Your Care Team to Help Prevent Gynecological Cancer
The more you know about your health, the more empowered you are to take control of it. There’s no greater example of the power you have to protect your future when it comes to preventative health visits and cervical cancer. While cervical cancer is one of the most common gynecological cancers, it doesn’t have to be.
With the guidance of their physician, physician assistant or nurse practitioner, women and teens can learn important information and take action that could potentially save their lives. That’s because most types of cervical cancer are now completely preventable.
Cervical cancer typically affects women between 30 and 50 years of age. Younger women are also at risk.
Of course, prevention works best when it starts early. The human papillomavirus (HPV) vaccine prevents cervical cancer. It is recommended to give the vaccine to children around 11 or 12 but can be given as early as 9 years of age.
If not previously vaccinated, the HPV vaccine is recommended for everyone through the age of 26 and can be administered by a primary care clinician or gynecologist. Even some adults in their 30s and 40s who were previously unvaccinated benefit from getting an HPV vaccination.
A pediatrician, primary care clinician, gynecologist or many pharmacists and healthcare workers in public health departments can administer the vaccine.
The HPV vaccine has been found to provide close to 100 percent protection against infections and pre-cancers caused by HPV.
According to the Centers for Disease Control and Prevention, HPV infections and cervical precancers (abnormal cells on the cervix that can lead to cancer) have dropped significantly since the vaccine has been in use in the United States. Among teen girls, infections with HPV types that cause most HPV cancers and genital warts have dropped 86 percent. There has been a 71 percent decrease for young adult women.
Women can also be screened for cervical cancer at regular intervals. There are two tests that can help:
Most health plans cover preventative care services—like vaccines and screening tests—at no additional cost. For people without insurance, Wellstar practices have low-cost annual exams that include evaluation for cervical cancer and a Pap test if it is medically appropriate.
To find a primary care clinician, gynecologist or pediatrician, call (770) 956-STAR (7827) or schedule online by clicking the “Book Now” button at the top of any page.
Take control of your health and read how to lower your risk and recognize the signs of gynecological cancer.

Wellstar Expands Obstetrics and Gynecology Services in Spalding, Upson Counties

Wellstar and Integral Advance Redevelopment Project

Empowering Youth Through Literacy: Wellstar Center for Health Equity & Small TALK Partner to Support Cobb Collaborative’s Family Literacy Kits
Learn more about the Wellstar Center for Health Equity.

Wellstar Presents: A Conversation With Martin Luther King III
In a heartwarming display of camaraderie, Wellstar team members gathered across the system to honor Dr. Martin Luther King Jr.'s life and legacy as part of the health system’s annual program to recognize his profound impact on civil rights in the United States. This year, the program featured a compelling conversation with his eldest son, Martin Luther King III.
A humanitarian and civil rights activist in his own right, King sat down with nationally renowned journalist Monica Kauffman Pearson to discuss his parents' legacy of nonviolent and peaceful activism, and how their influence continues to shape his own life and efforts. The conversation centered on one of his father’s most famous quotes: "The time is always right to do what is right."
King discussed the importance of using constructive dialogue in times of conflict, sharing insights into how his late mother, Coretta Scott King, successfully convinced President Ronald Reagan in 1983 to sign into law a bill that created Martin Luther King Jr. Day as a federal holiday.In the conversation, Kauffman Pearson asked King how his father's legacy extends to health equity.
“I think we're making small steps. We need to accelerate it to gigantic steps,” King said, encouraging people to consider an important question: “What are you going to do to make your community, your nation, our world better?”
“Like Martin Luther King III, I believe we have a responsibility to make the world a better place,” said Candice L. Saunders, president and CEO of Wellstar Health System. “In healthcare, we seize that opportunity one patient at a time, serving with compassion and honoring every voice as we work together to enhance the health and well-being of every person we serve.” View excerpts of the conversation here.
Wellstar CEO Candice L. Saunders to Retire
MARIETTA, Ga. (Jan. 15, 2025) – Wellstar Health System announced today that President and CEO Candice L. Saunders has shared her intention to retire at the end of the nonprofit’s fiscal year on June 30, 2025, after an exceptional career of service and accomplishment.
Saunders joined Wellstar in March 2007 as president of Wellstar Kennestone Regional Medical Center. She was promoted to executive vice president and chief operating officer of Wellstar Health System in May 2013 and was appointed president and CEO in July 2015.
Saunders has guided Wellstar’s growth from its roots as a small group of community hospitals into a leading nonprofit health system with 11 hospitals, more than 400 medical offices, and 33,000 team members serving more than 3 million patients each year in 148 of Georgia’s 159 counties. Today, Wellstar is a national leader in charity and uncompensated care, providing more than $1 billion annually in healthcare to patients who are uninsured or under-insured.
“Candice is a compassionate caregiver and a visionary leader,” said Frank Ros, chairman of the Wellstar Board of Trustees. “Under her leadership, Wellstar has forged new community partnerships, implemented new care models and clinical innovations, and advanced cutting-edge technologies that are improving health outcomes and enhancing the patient experience. As a result, Wellstar has become an essential provider of quality healthcare for Georgia.”
“I will leave with a full heart. I feel fortunate to have had the opportunity to lead Wellstar and work with so many talented leaders and caregivers, all committed to our vision of providing world-class healthcare to every person, every time,” said Saunders. “I’m so proud of our team and all we’ve accomplished together.”
The announcement begins a planned six-month succession process. The Wellstar Board of Trustees will retain an executive search firm and create a CEO search committee that will be led by Ros. The national search will include internal and external candidates. Saunders will remain engaged after June through an appropriate period to ensure a smooth leadership transition.
Saunders started her career as a critical care nurse and still regularly puts on scrubs to make rounds at Wellstar facilities and listen to doctors, nurses, patients, and families. She is known for her emphasis on building a positive workplace culture and developing strong leaders. During her tenure, Wellstar has received numerous awards as a great place to work, including Fortune’s list of 100 Best Companies to Work For in America.
With the belief that the patient should be at the center of every activity, Saunders led Wellstar’s launch of the PeopleCare brand, created a rigorous strategic planning process, and established new mission, vision, and values statements that prioritize the consumer experience.
Saunders was the architect of the successful partnership between Wellstar and Augusta University’s Medical College of Georgia to create Wellstar MCG Health, strengthening healthcare in the Central Savannah River Area and enhancing medical education in Georgia. She led an expanded partnership with Kennesaw State University and its Wellstar College of Health and Human Services, helping to increase the number of much-needed nurses in Georgia.
One of Wellstar’s significant innovations during Saunders’ tenure was the launch of Catalyst by Wellstar, which supports the development of early-stage technologies with the potential to improve health outcomes and the patient experience.
After Wellstar’s difficult decision to close Atlanta Medical Center following an unsuccessful two-year effort to find partners, Saunders forged a partnership with The Integral Group, a nationally recognized Atlanta-based firm, to develop a community-based plan for the future of the site. The work is being guided by a land-use plan unanimously approved by the Atlanta City Council with support from Atlanta Mayor Andre Dickens and the leadership of the local neighborhood association.
Saunders served on the Boards of Trustees of the American Hospital Association and the Georgia Hospital Association, where she also served as chairperson. She serves on the Boards of Directors of the Coalition to Strengthen America’s Healthcare, the Metro Atlanta Chamber of Commerce, the Cobb Chamber of Commerce, and the Board of Trustees for the Kennesaw State University Foundation. She also belongs to the Downtown Rotary Club among many other civic organizations. Modern Healthcare named her to its lists of Top 25 Women Leaders and Top 50 Most Influential Clinical Executives. In 2022, she was recognized by the Atlanta Business Chronicle as Atlanta’s Most People-Focused CEO. In 2025, she was named to Georgia Trend’s list of 100 Most Influential Georgians for the 9th consecutive year.
# # #
ABOUT WELLSTAR HEALTH SYSTEM
Wellstar personalizes the patient experience. We call it PeopleCare and it's only possible thanks to our 33,000 team members who provide compassionate care for every stage of life. PeopleCare also means we serve our communities as a non-profit health system, providing more than $1 billion annually in charity care and community programs, and operating the largest integrated trauma network in the State of Georgia. We embrace innovation and technology, nurture early-stage companies through our venture firm Catalyst by Wellstar, and train future generations of caregivers with academic institutions including the Medical College of Georgia. Wellstar honors every voice, earning Newsweek's recognition as one of America’s Greatest Workplaces for Diversity, and one of Fortune's 100 Best Companies to Work For. To learn more, visit Wellstar.org.

Feeling Sick? Know Where to Go to Get Care
Whether you experience an injury, minor illness or simply need a wellness exam, the most important step you can take is getting the care you need. That way, you can find trained experts for your specific medical needs, stay ahead of potential health issues or even help prevent your condition from worsening.
With primary, virtual, urgent and emergency care services available, as well as retail pharmacies, how do you decide which type of care is best for your medical situation? Learn the differences between each type of medical service so you don’t delay and get care right away.

If you are ill and have minor symptoms, over-the-counter medications can help you feel better. At your local retail pharmacy, you can find over-the-counter treatments for minor conditions like colds. If your symptoms worsen or do not go away with over-the-counter treatments, contact your primary care team or visit an urgent care location.
Local pharmacies also carry at-home COVID-19 tests, offering a convenient testing option for people who have been exposed or are experiencing mild symptoms of COVID-19.
Whether you have a busy schedule or are just looking for a more convenient option, virtual appointments are an easy way to keep up with your health from anywhere.
At Wellstar, we offer virtual visits with both primary care clinicians and specialists—no matter if you are an established patient or not. Connect with your Wellstar care team over the phone or with video on a computer, smartphone or tablet.
If you’re an established patient, simply request a virtual visit through MyChart. If you don’t have an account, it’s easy to sign up for MyChart and keep all of your important health information in one secure space. You can also call your physician’s office directly and request a virtual appointment over the phone.
These days, many types of appointments can be done virtually, including consultations, care for chronic conditions and prescription management. In addition to virtual primary and specialty care appointments, we also provide virtual urgent care through WellstarON for minor medical concerns.
While virtual care is a convenient way to stay well, it should never be used in place of emergency care. If you are experiencing a life-threatening medical emergency, call 911 right away.
Primary care is ongoing, comprehensive care and preventative medicine that helps you live a full, healthy life.
Your primary care clinician—either an internal or family medicine physician, pediatrician or OB/GYN, depending on your age and medical needs—gets to know you and your health history on a deeper level. That means they have a more accurate view of your overall wellness.
Services include:
Find a Wellstar primary care location in your neighborhood.
If you’re dealing with a minor injury or illness or need care after your physician’s regular office hours, going to urgent care is often the right choice. Wellstar Urgent Care Centers provide quick, convenient care for non-emergency medical conditions.
We also offer urgent care through WellstarON, which provides virtual health visits for minor medical concerns from the comfort and convenience of home.
Wellstar Urgent Care provides:
Find a Wellstar urgent care location near you or make a virtual urgent care appointment.
In a life-threatening medical emergency, every second counts. Never put off getting the proper care when lives are on the line. Remember, driving yourself to the emergency department (ED) may delay care, so call 911 for the fastest access to emergency care.
When the unexpected happens, Wellstar is always ready in a medical emergency. Our trained team provides expert emergency care 24 hours a day for people of all ages. We even have several pediatric emergency room locations, specifically designed to treat children.
Recognize the signs of a medical emergency:
Find a Wellstar emergency department close to you. Remember, call 911 right away in a medical emergency. That way, care can begin sooner during the crucial time it takes to be transported to the hospital.

MartinCare
There’s a reason the “widowmaker” heart attack got its nickname. According to the American Heart Association, the survival rate following this type of heart attack, which is caused by a blockage in the heart’s main artery, is only 12% when it occurs outside a hospital or advanced cardiac care center. But thanks to the swift response of his cardiac-nurse wife and the excellent care of his cardiovascular surgery team, Martin Hornberger is here to tell his story and offer hope to others.
It was a Saturday morning in May. Martin started his day with breakfast and a cup of coffee—as he always did. He had no pain or unusual symptoms—merely some indigestion, which he managed by taking a few antacids, and fatigue that was a common symptom of his diabetes.
Aside from having diabetes, the Cartersville resident had always considered himself relatively healthy. When he wasn’t hard at work as an engineer, he spent much of his time outdoors and enjoyed staying active.
Everything changed later that day when he and his wife, Donna, left the house to see their granddaughter play tee ball. Halfway there, Martin collapsed while driving.
“I tried to tell my wife to take the steering wheel but never got the words out,” he said.
Donna, a cardiac nurse at Wellstar Kennestone Regional Medical Center, jumped into action. Unable to move Martin’s foot off the gas pedal, she eventually got the truck under control by turning off the ignition. Then, using her nearly 50 years of emergency room and cardiac training, she began administering hands-only CPR. Another driver who stopped to help called 911.
While the EMTs were en route, Donna was able to revive Martin by delivering multiple rounds of chest compressions to mimic the heart’s pumping action.
“Knowing her, she didn’t even have to think about it. Her training kicked in and she just went to work,” Martin said of his wife. “She’s the hero of this whole thing.”
The EMTs rushed Martin to a nearby hospital in Rome, where the cardiac team performed an emergency stent to restore blood flow in his main heart artery and get him stabilized. However, further tests revealed even more blockage that could not be treated with additional stents. Martin would need heart bypass surgery.
Donna immediately began advocating for him to be transferred to her unit at Wellstar Kennestone for surgery. She wanted the best possible care for her husband and knew the Marietta hospital was a Certified Comprehensive Cardiac Care Center—the first in Georgia and the fourth in the nation to receive this highest certification in cardiovascular care by The Joint Commission and American Heart Association.
“I knew the process; I knew the people,” she explained. “If anyone could save my husband, it was them.”
On Wednesday evening Martin was moved to Wellstar Kennestone, where he was introduced to Dr. Richard Myung, the cardiothoracic surgeon who would be performing his coronary artery bypass grafting (CABG) surgery. Dr. Myung took the time to explain to Martin everything that would happen during the procedure. The surgeon’s personable demeanor and genuine empathy immediately put Martin at ease.
“He has a tremendous bedside manner—his presence in the room was comforting,” Martin said. “The smile on his face and the relaxed confidence [gave me] reassurance that things are going to work out.”
Dr. Myung works as part of a larger multidisciplinary team to provide the highest quality care to every patient, from diagnosis to surgery and through recovery. His commitment to excellence has helped Wellstar Kennestone’s cardiovascular program earn a distinguished three-star rating from the Society of Thoracic Surgeons for its patient care and outcomes in isolated CABG. The award places the hospital among the most elite programs for heart bypass surgery in the U.S. and Canada.
Martin’s case, unfortunately, was not unique for Dr. Myung. “Probably a third of our cases are bypass cases,” the surgeon explained.
CABG is regularly performed to treat people with multiple blocked coronary arteries. It involves a surgeon taking a healthy vein or artery from another part of the body (in Martin’s case, Dr. Myung used a vein from his leg and an artery from his chest wall) and attaching it to the aorta and the coronary artery above or below a blockage. This creates a new route for blood to flow around the blockage.
Although the most common approach is traditional open-heart CABG, where the heart is stopped and a heart-lung bypass machine is used, other less-invasive methods—including “off-pump” procedures, in which the heart does not have to be stopped—are sometimes an option. Dr. Myung determined that Martin could undergo an off-pump CABG, which reduces the risk of complications and often leads to a shorter hospital stay.
When the big day arrived, Martin’s procedure went smoothly, Dr. Myung reported. Thanks to his expert team and their advanced techniques, Martin was going to be okay.
Martin is grateful to the nursing team at Wellstar Kennestone for supporting him before, during and after his procedure.
“From beginning to end, they were attentive, encouraging [and] they coached me through each step,” he shared.
One nurse in particular made a lasting impact on Martin through his clear, comforting instructions that let him know exactly what to expect.
“Prior to the surgery, he was telling me, ‘Now, when you wake up, you’re going to have a tube in your throat. Don’t fight it. Just remember that this is part of the recovery.’ And you know, that stuck in my mind,” Martin recalled. “They had prepared me for everything I was going to face. There were no surprises, and I really appreciated that.”
Within 24 hours of his bypass surgery, Martin was out of bed and walking laps around the hospital floor with a walker. “I even heard a patient telling the nurses, ‘Tell that guy to slow down!’” he said with a laugh.
With the specialized care of his nursing team, he continued to improve daily and was discharged only four days after surgery.
“That whole place is full of heroes. They do it day in and day out,” Martin said. “They love what they do and they’re good at it. They take pride in that—and they should.”
Thanks to Dr. Myung and his less-invasive techniques, Martin experienced a relatively painless recovery. Six weeks after his surgery, Martin felt well enough to return to his full-time job.
Determined to get back to life as normal as quickly as possible, Martin kept himself moving at home and also visited Wellstar Cardiac Rehabilitation in Woodstock to continue building his strength. Wellstar has one of the largest cardiac rehabilitation programs in Georgia, which helps patients improve their long-term outcomes.
Martin will continue to monitor his cardiac wellness through regular check-ups with expert Wellstar cardiologists. The Wellstar Center for Cardiovascular Care ensures patients who recently had heart surgery can easily receive the follow-up care they need by offering more than 20 convenient locations across Georgia.
Martin recognizes that adjusting to life after a heart attack—and all the emotional challenges and physical limitations that come with it—will take time. For now, he is focused on making small strides every day.
“I do get tired but not as often, so I’m seeing progress in the length of time that I’m doing activities, that I’m able to sustain it longer,” Martin shared. “That’s encouraging.”
Without the first-rate care he received at Wellstar, Martin wouldn’t be where he is today—back to work, living an active lifestyle and surrounded by his children and grandchildren, who lovingly call him “Gramps.”
He also wouldn’t have had the chance to make a memory he would cherish forever. On a Sunday afternoon in August, Martin was selected by Wellstar to throw the opening pitch at the Atlanta Braves vs. Miami Marlins baseball game. He was joined by Donna and their family on the field at Truist Park and later enjoyed cheering on the home team alongside Dr. Myung.
“That was a huge experience in my life,” Martin said. “Never in my wildest dreams did I imagine I would ever do that in my lifetime.”
Today, Martin is sharing his story to encourage others who may be recovering from a heart condition. “It does get better,” he offered. “It doesn’t happen as quickly as you want it to, but I can see it progressing.”
By recounting her husband’s experience, Donna has inspired several of her patients to consider cardiovascular procedures that could detect potential blockages. She also hopes it will influence more people to learn CPR.
“If our story can even save one life, that would mean the world to us,” she said, humbly adding, “I’m not a hero; I’m a wife that loves her husband that just so happens to be a cardiac nurse.”
Martin is all too aware that his wife’s combination of critical thinking skills, composure under pressure and cardiac training is why he is still here today. “I was lucky to have a cardiac nurse as my passenger that day,” he shared. “I am very blessed to be alive.”
Learn more about Cardiovascular Surgery at Wellstar.

Expert Burn Care at Wellstar Cobb Medical Center
By Dr. Travis Perry, burn surgeon and medical director of the burn center at Wellstar Cobb Medical Center
By Dr. Travis Perry, burn surgeon and medical director of the burn center at Wellstar Cobb Medical Center
The burn and wound treatment center at Wellstar Cobb Medical Center, operated in partnership with Joseph M. Still Burn and Reconstructive Centers of America, has provided expert treatment for burns in both adults and children for over a decade. During the winter months, burns are common as people gather near indoor or outdoor fires, set off fireworks or spend time outside in cold weather.
Burns are tissue damage to the skin from exposure to sun, heat, chemicals, electricity, flames, steam or extreme cold weather.
Frostbite, a cold injury also treated at Wellstar Cobb, is when the skin freezes after exposure to cold temperatures and is most common on the fingers, toes, nose and ears.
Burns are categorized by their severity:
All burns should be evaluated by a burn care expert.
You can help keep your family safe by taking precautions around potential causes of burns:
If you do experience a burn, take these steps right away to limit damage to the skin:
The expert burn care team at Wellstar Cobb provides critical care for severe burns, as well as reconstructive surgery. In our 16-bed inpatient unit and 10-bed burn medical/surgical unit, we treat adults with all sizes and types of burns and children one year and older with burns on less than 20% of their bodies.
The inpatient burn unit offers long-term care for critically ill burn patients, including innovative limb salvage, skin and tissue saving surgeries. Our outpatient clinic serves walk-in patients and scheduled return visits. We offer state-of-the-art hyperbaric oxygen therapy as both an inpatient and outpatient service, as well as hydrotherapy.
Learn more about burn care at Wellstar Cobb at wellstar.org/burncenter.
5 Habits to Become the Healthiest You
Small changes add up to big results. By incorporating simple habits into your life, you can kickstart your wellness journey and stay on track for the long run.
Use the SMART goal-setting system to help define your goal and develop attainable resolutions.
Keep in mind, you may encounter some bumps in the road along the way. Recognizing all the small accomplishments can help you stay motivated and win in the long run.
“Focus on what small steps you’ve accomplished rather than how far you have to go,” Dr. Gomez shared. “Also, have a resiliency plan to help you bounce back after a more challenging day.”
Build new habits into your regular routine by beginning small and adding on over time. With this “habit stacking” technique, you pair your new habit with something you’re already doing. For example, if your goal is to drink more water, drink a glass of water while making your morning coffee or tea.
Seeing your primary care clinician at least once a year is the single most important thing you can do for your health.
At your annual exam, your care team will help keep you healthy and reach your wellness goals. They screen for diseases to stay ahead of medical issues and check in on your overall well-being.
Set a reminder on your phone or calendar to prompt you to book an appointment. You can also use an important date, such as your birthday, anniversary or a holiday, as a marker to remind you to schedule a visit.
If you’re focused on improving your fitness routine, put a plan in place to be more active.
“Begin to incorporate a little more exercise into your daily routine,” said Wellstar Primary Care Physician Dr. Jeremy Boyd. “The Centers for Disease Control and Prevention offers a suggestion of 150 minutes of aerobic activity a week. I like to break that down to a good 40 minutes four times a week.”
Having a bedtime routine is essential to catch more Zs throughout the year. When you wake up feeling rested, you often feel more productive and energized throughout the day.
Get started by setting a specific time to go to sleep—and stick to it. Make sure you reserve at least seven to nine hours per night for sleep.
Limit your screen time before getting in bed. Bright screens from a phone, computer or TV can keep your brain awake and make it harder to fall asleep.
If you’re having trouble getting to sleep, have a decaffeinated cup of tea or take a warm bath to help you relax.
When it comes to losing weight, many people look for a quick fix, which can often create unhealthy ways of eating. Creating a healthy eating plan from the start can help avoid any fad diet pitfalls.
Nutrition plans that restrict or eliminate food groups and those with extreme calorie deficits are difficult to maintain and can often produce more weight gain or undesired results, according to Wellstar Registered Dietitian Kelly Prian.
Diet trends can also create a negative relationship with food, which can make it harder to achieve your goals. Prian shared that those with long-term success focus on maintaining a plan that enables steady weight loss over time.
A healthy nutrition plan is balanced and emphasizes whole foods, such as fruits and vegetables, lean proteins, low fat dairy, nuts and seeds, and whole grains.
Try not to overcomplicate healthy eating. You can start by filling half your plate with vegetables or having fun trying new recipes.
Self-care is an important aspect of your mental well-being and should be made a consistent part of each day.
“Make self-care a priority and a non-negotiable,” Dr. Gomez said.
“Think of self-care as a form of personal healing and a way to strengthen resilience,” Dr. Gomez explained. “Much like the way exercise enhances physical health, self-care enhances mental health.”
According to Dr. Gomez, it can be helpful to turn tasks we do on “autopilot” into more meaningful experiences.
“When washing your hands, give yourself a hand massage,” Dr. Gomez shared. “When driving, use red lights to practice deep breathing. Listen to a book on tape or language lessons rather than the radio or call someone to reconnect.”
If you feel overwhelmed by stress or anxiety, Wellstar behavioral health specialists are here for you.
“Working with a mental health provider is different than speaking with a friend or even a life coach,” Dr. Gomez said. “Mental health professionals are trained and licensed to address psychological or emotional wellness.”
Need support? Connect with a Wellstar behavioral health specialist.

Wellstar Announces Kevin Smith as President of Wellstar Spalding Medical Center and Wellstar Sylvan Grove Medical Center
Wellstar Health System has selected Kevin Smith to join Wellstar as Senior Vice President and President of Wellstar Spalding Medical Center and Wellstar Sylvan Grove Medical Center. Smith brings a wealth of experience spanning over 20 years in healthcare operations, organizational leadership, and community engagement. He will work alongside the current local leadership team to set strategy and implement Wellstar’s commitment for continuous improvement.
Wellstar continues to increase access to care in Spalding and Butts counties, opening new primary care and neurology clinics in 2024 and previously opening or expanding clinics for cardiology, oncology, orthopedics and gastroenterology. Last year, Wellstar’s Spalding and Sylvan Grove hospitals provided $16.7 million in uncompensated care, and nearly 3,000 people in Spalding and Butts counties benefited from a Wellstar Community Health program. Wellstar also recently expanded its graduate medical education program at the hospitals, knowing that new physicians are more likely to stay in the communities where they begin their careers.
“Kevin’s experience includes both small rural and larger urban markets, making him ideal to lead our continued commitments to PeopleCare in Spalding and Butts counties,” said Mary Chatman, PhD, RN, executive vice president of acute care operations for Wellstar. “In addition to leading our local teams, Kevin will collaborate with executives across the Wellstar system, partner with our physician enterprise, and engage with community partners to advance healthcare in the region.”
Most recently, Smith served as Vice President and Chief Operating Officer at Atrium Health Wake Forest Baptist-High Point Medical Center, where he oversaw operations for a more than $440 million revenue organization with key service lines including Oncology, Heart/Lung/Vascular and Behavioral Health.
Smith holds a Doctor of Philosophy in Industrial/Organizational Psychology, a Master of Health Administration, and a Bachelor of Science in Radiological Sciences. He is a Fellow of both the American College of Healthcare Executives and the Association for Medical Imaging Management, reflecting his commitment to healthcare excellence and innovation.

Make Health Your Habit
The start of a new year is a great time to focus on your health. For many of us, that means setting resolutions to live a healthy, full life. While many people like to reset their health goals in January, Wellstar partners with patients year-round to help them feel their best.
By following tips from Wellstar health experts, you can create realistic resolutions and better your health—making healthy choices a lifelong habit rather than a short-term goal.
When it comes to your wellness goals, staying healthy starts with a visit to your Wellstar primary care team.
“Your primary care provider will collaborate with you to create a customized care plan and recommend screenings based on factors such as your age, gender and family history,” said Wellstar Primary Care Physician Dr. Cristina Dasoveanu. “Regular screenings can help you stay ahead of issues and catch any health concerns early.”
To check your health status and screen for potential medical issues, your clinician will take your Foundational 4 numbers, a few screenings that identify risk factors for some health conditions such as heart disease.
A blood pressure test helps diagnose hypertension (high blood pressure), hypotension (low blood pressure), heart disease and other conditions.
The amount of glucose (sugar) in your blood can indicate the onset of diabetes or risk of heart disease, heart attack or stroke.
Low-density lipoprotein (LDL), often called “bad” cholesterol, can indicate clogged arteries, which may lead to heart disease, heart attack or stroke.
A higher level of body fat may indicate an increased risk for heart disease, hypertension (high blood pressure) and diabetes.
“Gynecologists partner with women in their healthcare across the lifespan,” said Dr. LeThenia “Joy” Baker, a Wellstar obstetrician and gynecologist. “The first gynecologic visit is recommended between 13 and 15, and the first exam between 18 and 21.”
Gynecologists are uniquely positioned to care for women from adolescence through menopause and beyond.
“We’ll make sure you are up to date on screenings like mammograms and Pap smears, help you make informed decisions about family planning and fertility, and provide medical and surgical treatment for a variety of conditions affecting the female reproductive system,” Dr. Baker said.
In addition to in-person primary care visits, Wellstar also offers virtual care options. Connect with your Wellstar clinician over the phone or with video on a computer, smartphone or tablet.
“While primary care physicians help patients meet long-term wellness goals, we’re also here for you when you’re sick,” said Wellstar Primary Care Physician Dr. Georgia Forrest. “Your primary care provider is already familiar with your background and health needs, so we can seamlessly continue that care and help you get back on track when you’re ill.”
If you need to see a specialist such as a cardiologist, pulmonologist or neurologist, your primary care team will refer you for that specialized care while continuing to help you manage your overall wellness.
“Through our patient portal MyChart, specialists and primary care physicians can see test results and visit summaries and stay updated on how each of us is working with the patient,” Dr. Forrest said.
If you’re a MyChart user, E-visits are a convenient way for you to receive care from a Wellstar clinician without needing to schedule an appointment or come to the clinic. Through MyChart, tell us about your health concern by answering a few questions about yourself and your symptoms, then a primary care expert will respond in MyChart with your care plan.
Conditions that can be treated with an E-visit include:
Log on to MyChart and click “Symptom Checker” from the menu in the top left of the screen to start an E-visit.
For more immediate healthcare needs that are not life-threatening, you can talk to a clinician with WellstarON, our virtual urgent care.
In an emergency, such as if you are having trouble breathing or experiencing chest pain, call 911.
Learn more about the different types of care Wellstar offers and where to go if you’re not feeling well.

Wellstar MCG Health is a Partnership Built on Progress
Candice L. Saunders and Russell Keen
We have a responsibility.
The nurse who sits at the bedside, holding a patient’s hand; the professor committed to training the next generation of caregivers; the hospital system executive seeking innovative technology to advance healthcare. They’re united by a shared sense of responsibility — to care for others.
That powerful commonality and our cultural alignment has been the underpinning of the successful partnership between Wellstar Health System and Augusta University’s Medical College of Georgia. In the year since Governor Brian Kemp, our state legislators and the University System of Georgia’s Board of Regents put their trust in us to create Wellstar MCG Health, we’ve improved healthcare in the Central Savannah River Area and enhanced medical education for future generations of Georgia caregivers.
From the beginning, we knew our people would be the key to our success. They’ve committed their lives to caring for others, and we’re committed to caring for them. It’s why we prioritized pay raises, enhanced mental health support, and now offer additional resources to help them take care of themselves and their families. Thanks to their feedback, we’re also investing in their career growth, with programs like CareerCare, which provides funding to help further their healthcare careers.
Supporting caregivers extends beyond those on our team. We’re also expanding the pipeline of clinicians to address our state’s chronic physician and nursing shortages. The Medical College of Georgia is the fourth largest medical college in the country, and the second-largest sponsoring institution for graduate medical training. By bringing academic excellence and advanced research together with deep healthcare experience and extensive resources, we’re able to offer innovative academic teaching models that ensure more physicians are trained in a modern clinical environment. Together, we’re building the healthcare workforce of the future.
As we address the need for more caregivers, we can’t overlook the need to expand access to care. To do that, we’ve increased digital health services and launched mobile care vans to serve rural communities. We’re looking ahead too, building the first hospital in Columbia County, the largest county in the state without its own hospital. Opening this 100-bed, Level II trauma center means people will have better access to the expert, compassionate care they need, right in their own backyard.
For the facilities already serving the area, there are now 129 new doctors, four new urgent care centers, and we’ve introduced innovative technology to improve patient care. We’re the first hospital in Georgia to use Galleri cancer testing, for example, which allows us to use just one blood test to detect more than 50 types of cancer earlier than ever before. We also have two new magnetic resonance imaging (MRI) suites featuring state-of-the-art machines for faster scanning.
Another piece of technology new to WMCG ensures our caregivers have the tools they need to give people the best care possible. It’s called Epic, an electronic medical records system, and it lives up to its name. With Epic, our caregivers now have improved data access for more accurate diagnoses, better treatment plans, and improved patient outcomes. Epic allows students to learn on modern technology, it facilitates research and makes it easier for patients to access their medical records. We invested approximately $175 million in this technology, along with other upgrades, and completed the implementation almost two full years ahead of schedule. It's a game changer and we couldn't be prouder of how the team came together to get this technology up and running.
Georgia’s leaders have put their faith in this partnership, an honor we take seriously. As we continue our work to create a healthier future for all Georgians, we’re committed to collaboration and financial sustainability, because we know our communities depend on us today and for generations to come. Improving the health and well-being of every person we serve isn’t just our responsibility, it’s our privilege, and none of it is possible without our dedicated team members. It’s heartwarming to see the way they embrace each other as one team. In the wake of hurricane Helene, their compassion hasn’t wavered as they care for patients and each other, a testament to their strong bonds. This is a team that cares deeply about each other and the communities we serve; a team that empathizes and uplifts; a team with determination and heart. With that kind of spirit, we can accomplish anything.
Candice L. Saunders is president and CEO of Wellstar Health System and Russell Keen is president of Augusta University.
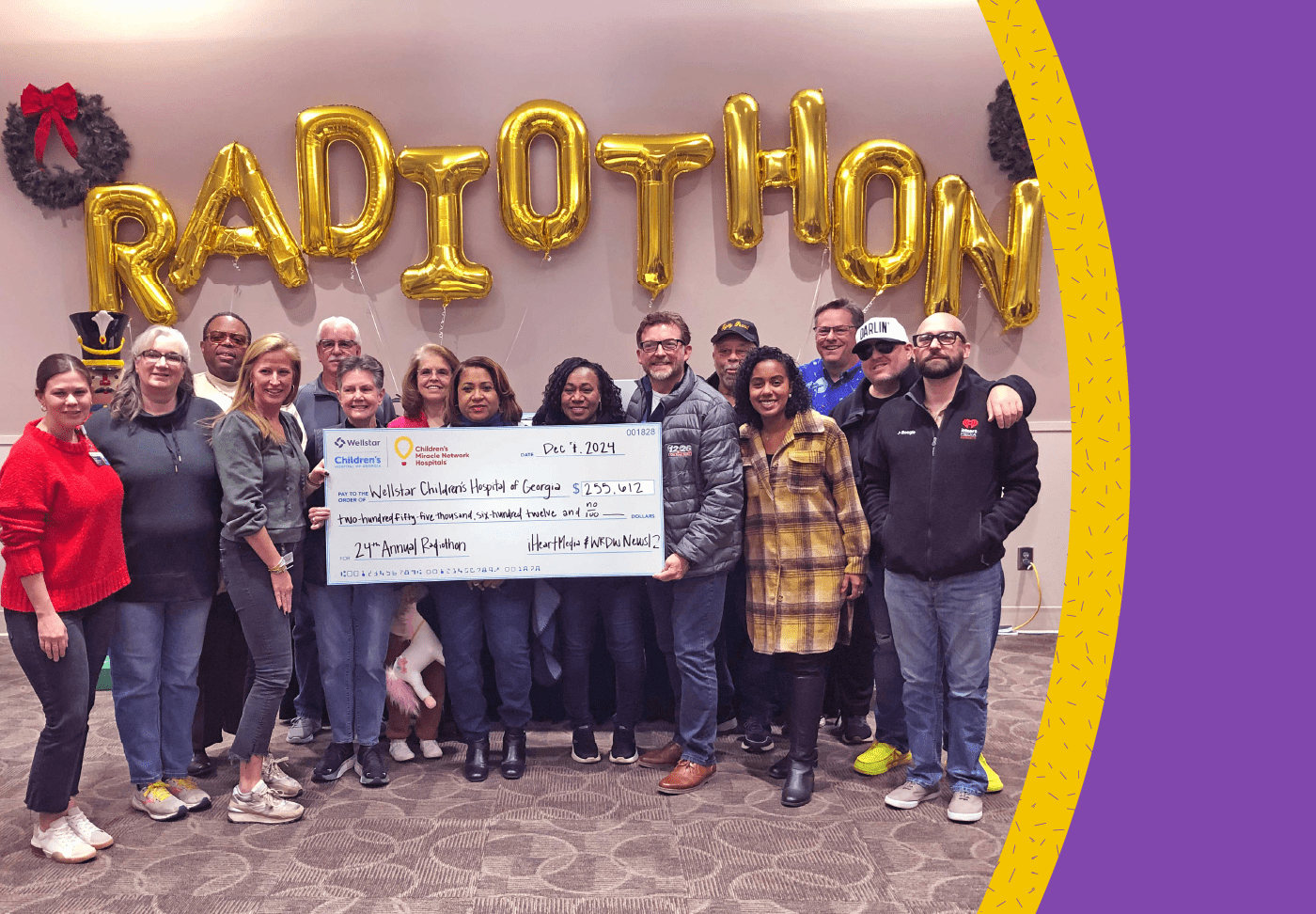
24th Annual iHeartMedia Cares for Kids Radiothon Raises $255,612 for Wellstar Children’s Hospital of Georgia
Christmas music and cheers filled the halls of Wellstar Children’s Hospital of Georgia Dec. 5 through 7 as listeners and viewers of local iHeartMedia radio stations and WRDW-TV generously supported patients and families for the 24th consecutive year.
In the end, the community pledged $255,612 to support Wellstar Children’s.
iHeartMedia generously donated the 72 hours of airtime to the cause while three of its popular radio stations—104.3 WBBQ, 96.3 Kiss FM and 105.7 The Bull—and WRDW News 12/NBC 26 broadcast live from the hospital.
“The children’s hospital could not survive without the support of the community. I’m just so grateful for everyone’s support,” said Dr. Valera Hudson, pediatrician-in-chief of Wellstar Children’s. “No children’s hospital thrives without philanthropy; 100% of the money that’s raised is used directly to help the children we take care of here. All of the funds stay right here at the Wellstar Children’s Hospital of Georgia.”
Wellstar Children’s is a not-for-profit hospital with specialists who care for pediatric patients with a range of conditions, including the most complex conditions.
Some of the patients who have been treated at Wellstar Children’s shared their stories with DJs and reporters throughout Radiothon. For example, 9-year-old Kensley Woodberry began developing spots on her hands and feet that became so painful, she could no longer walk. She stopped eating and refused to play. A team of specialists at Wellstar Children’s diagnosed her with juvenile dermatomyositis, a rare autoimmune disease that causes the body to attack its own muscles and leads to inflammation throughout the body.
This past summer, Kensley attended Camp Joint Venture, a summer camp for children with rheumatic conditions. It gives kids like Kensley the opportunity to enjoy the summer camp experience while a team of medical personnel is nearby in case they are needed. The camp is one of several summer camps funded through Radiothon.
Radiothon also allows for purchases of comfort items like Zaky Hugs, which mimic the warmth and security of a parent’s touch for babies in the NICU; red wagons for transporting young patients around the hospital; and sensory toys for children with autism. These are only a few of the items that bring joy, comfort or care to young patients that the hospital could not purchase without community support.
Though Radiothon has concluded, donations can be made throughout the year by calling (706) 721-4004, by emailing Wellstar Children’s Director of Philanthropy Catherine Stewart or through the Cares for Kids Radiothon website.

Former Falcons Player Surprises Wellstar Patient After Football Injury
A Wellstar patient recovering from a brain injury got a surprise visit Thursday from a former Atlanta Falcons player in celebration of the teenager’s graduation from the intensive care unit of Wellstar Kennestone Regional Medical Center in Marietta.
Oheneba “O.J.” Appiah, 17, who plays linebacker for the football team at Archer High School near Lawrenceville, sustained the brain injury during a football game last month.
“After the game, he said he was dizzy, and that’s when he passed out,” said his mom, Elizabeth Appiah.
“I met O.J. on the worst day of his life,” said Dr. Phillip Parry, a Wellstar neurosurgeon. “He had a life-threatening bleed inside his head, and we took him to surgery immediately.”
O.J. has come a long way during his 20-day stay in intensive care.
“His miraculous recovery is a testament to the care he received and an inspiration to us all to continue doing what we do every day,” Dr. Parry said.
“We are so grateful to God,” O.J.’s mother said. “The team here is great, and the nurses are amazing.”
Wellstar Kennestone’s neuro-ICU team, called “5 Blue East,” bonded with O.J. and his family over their love of football. The team members said it’s been great witnessing O.J.’s recovery and seeing his personality come back.
Former Atlanta Falcons and Pro Bowl player Ovie Mughelli visited O.J. during a special surprise party Thursday. Mughelli gave O.J. a signed jersey and photo from his professional football days and shared advice.
“You had a hard situation happen to you, but you can do hard things,” said Mughelli, encouraging O.J. to “ask for help up front.”
The young football player had just one question for the former NFL player: “How do you get an offer?”
By working hard and building relationships, Mughelli responded. He also stressed the importance of focusing on school. After learning O.J. had never been to a Falcons game, Mughelli invited him to attend one next season.
Wellstar Kennestone President Lorrie Liang, who also stopped by to congratulate O.J., noticed Mughelli’s gift.
“Now you have a jersey to wear during rehab,” she said to O.J.
But O.J. didn’t feel like waiting. He put on the jersey almost immediately.

On Giving Tuesday, Local Mom Urges Donors to Consider Wellstar’s Small TALK Program
Carter Fawcett has been reading to her four children since before they were born. As a fifth grade teacher, she knows the importance of immersing children in words, stories and songs, starting when they’re still in the womb.
“While I was pregnant with my firstborn, reading and singing to him was my whole attachment to motherhood,” she said. “The other three were just along for the ride, even in my belly, listening to me read aloud to my toddlers.”
Fawcett’s children are patients of Dr. Melissa Boekhaus, a pediatrician at Wellstar Pediatric Adolescent Center in Smyrna. Fawcett was thrilled to learn that the practice had implemented a literacy program called Small TALK, made possible thanks to generous donations from the Wellstar Foundation.
“I love knowing that Wellstar encourages families to read together,” she said.
Wellstar is the only health system in Georgia that provides a high level of literacy support throughout the entire spectrum of pediatric care, from pre-birth through third grade and beyond.
During various touchpoints, from prenatal care to pediatric well-child visits, Small TALK teaches parents and caregivers to tune into their child’s interests and activities. By regularly asking open-ended questions, even to newborns, children learn how to become conversational partners.
“We encourage parents to use their home language and speak in complete sentences using complex vocabulary to lift their child’s language and grow their understanding of the world,” said Lisa Liedke, manager of Small TALK for Wellstar. “Talking, reading, playing and singing together helps even the youngest children establish these skills.”
“Parents are their children’s first and best teachers,” Liedke said. “Empowering the family to have this intentional engagement carries this role from Wellstar to home.”
Small TALK allows healthcare professionals to work closely with families, explaining and coaching how to produce early healthy brain development and language acquisition. These conversations help monitor early development, address concerns and encourage early interventions through referrals if necessary.
“Just as children need food nutrition to grow their bodies, they require language nutrition to grow their brains,” Liedke said.
“If you’re looking for a charitable cause to support on Giving Tuesday, please consider the Wellstar Foundation,” said Fawcett. “Small TALK reaches children across all socioeconomic levels, setting them up with the foundational language tools they’ll need for educational success before they even start kindergarten.”
To learn more about the Wellstar Foundation or to make a tax-deductible donation, visit wellstar.org/give.
Language Development
Small TALK Timeline
.jpg?rev=e623251622ee4116956d7bf55a43cffe)
We’re Offering No-Cost Telehealth to Underserved Communities
Many people in low-income neighborhoods go without essential healthcare services, with reasons including lack of insurance, unreliable transportation or inflexible work schedules. At Wellstar Center for Health Equity, we’re excited to offer a simple solution for people living in northwest Atlanta: no-cost digital health services. Digital health services, also called telehealth or telemedicine, allow people to schedule virtual visits with a healthcare professional to access the care they need—when they need it.
This solution is possible thanks to a partnership between Wellstar, Family Life Restoration Center in Mableton and Giving Health, a Georgia-based telemedicine provider. To participate, people can sign up at Family Life Restoration Center. Then, they can schedule online telehealth appointments using a phone, smart device or computer. The program provides 24/7 access to:
Participants can use the digital health service for up to a year. Staff and volunteers at Family Life Restoration Center can help participants apply for Medicaid and find a primary care practice when they are ready.
Health and wellness success with telehealth
While the telehealth program is new, Giving Health has provided telehealth for low-income and uninsured people since 2019. They also offer after-hours digital health services for many clinics in the Wellstar Community Clinic Network.
Family Life Restoration Center is also part of the Wellstar Community Clinic Network, which was launched nearly 10 years ago to better serve the most vulnerable and under-resourced people in our communities.
Many people in Mableton and other areas in South Cobb County are living below the poverty line. Many do not have a primary care provider or health insurance. Round-the-clock access to telehealth can make a significant impact on people’s lives, helping them experience better health and avoid unnecessary trips to the emergency department.
The Family Life Restoration Center provides community members with food, clothing, spiritual encouragement and referrals to nearby social services. Wellstar has worked with the center for over a decade to meet the community’s needs, including vaccination clinics, health screenings and patient education programs.
Check out the Wellstar Find Help Tool
Another way we’re meeting health needs in our community is with the Wellstar Find Help Tool. It allows people to search for free or reduced-cost resources, including:
The tool, available in several languages, is one of several Wellstar initiatives to improve the health well-being of every person we serve by connecting them with resources such as nutritious foods, housing and education.
Learn more about the Wellstar Center for Health Equity.

Wellstar Health System Releases 1-Year Progress Report on Affiliation with Augusta University’s Medical College of Georgia
AUGUSTA, Ga. (Dec. 2, 2024) – Wellstar MCG Health is transforming healthcare in the state and advancing medical education for the next generation of caregivers. A new 1-year progress report details the significant strides that have been made since Wellstar Health System and Augusta University’s Medical College of Georgia (MCG) joined forces last year.
This strategic affiliation combines Augusta University’s academic excellence and research capabilities with Wellstar’s extensive healthcare expertise and resources. Since beginning the partnership on Aug. 30, 2023, Wellstar MCG Health has improved access to care, made substantial investments in facilities, and expanded innovative programs aimed at serving Georgia’s unique healthcare needs.
Highlights from the Year-One Progress Report:
“We’re proud of the progress we’ve made in this first year,” said Candice L. Saunders, president and CEO of Wellstar Health System. “From expanding access to care and enhancing our facilities to investing in our people, we’re dedicated to a brighter, healthier future for Georgia. This partnership is a testament to what we can achieve when we bring together academic and healthcare excellence.”
Dr. Russell Keen, president of Augusta University, added, “A great example of how Wellstar and Augusta University are collectively improving the lives of Georgians is the ongoing collaboration between MCG researchers and clinicians in the Georgia Cancer Center, the Children’s Hospital of Georgia and the MCG Center for Telehealth. I couldn’t be more pleased with the collaborative spirit, shared passion and culture of innovation that permeate Augusta University and Wellstar Health System.”
The Wellstar and Augusta University/Medical College of Georgia partnership will continue to evolve and expand its impact, with projects such as the new Wellstar Columbia County Medical Center, affiliated with the Medical College of Georgia, slated to open in 2026, which will bring acute care services to Georgia’s largest county without an existing hospital.

Aortic Experts & AI Identify Thousands with Hidden Aneurysms
Wellstar’s Comprehensive Aortic Program has identified thousands of hidden aneurysms in the past two years. The goal of the program is to help people before their conditions become life-threatening.
Aortic aneurysms are bulges in the body’s largest blood vessel. They can burst and cause severe damage or death if they become too big. Unfortunately, most people never know they have one because they are typically asymptomatic until they rupture.
However, the aortic experts at Wellstar found a way to help people before they have an emergency.
“When patients have CT scans at Wellstar for other reasons, we use artificial intelligence (AI) to sift through them and find images of someone who may have aneurysm,” said Wellstar Cardiothoracic Surgeon Dr. James Ryan Burke. “That allows us to proactively contact them and bring them in if appropriate for evaluation to discuss that diagnosis.”
Since the program launch in July 2022, more than 4,700 people with aneurysms have been placed under surveillance—a protocol to monitor people who have a risk. Surveillance allows people to avoid undergoing unnecessary surgery but to know when the aneurysm grows larger and becomes a greater concern.
For people who had large, potentially life-threatening aneurysms, cardiovascular surgeons and vascular surgeons performed more than 700 advanced procedures at Wellstar Kennestone Regional Medical Center since the program began.
“These are major cardiac operations only performed in centers that offer complex aortic surgery,” Dr. Burke said. “The outcomes are best when done in experienced centers that do a high volume of procedures, like Wellstar Kennestone.”
“This program is very patient-oriented. We have an excellent team of dedicated physicians at Wellstar to accomplish our mission and I think it’s very beneficial for both patients and physicians,” said Dr. Michael Corey of Vascular Surgical Associates.
The aortic program at Wellstar provides a higher level of aortic care than a patient would typically find in a local hospital. What makes the program unique is:
“The aorta is the largest blood vessel in the body. It runs from the heart, through the chest and abdomen and down to the legs,” said Dr. Burke. “When you have a disease process involving the aorta, it requires multiple specialties.”
Wellstar’s specialized aortic team includes cardiovascular surgeons, vascular surgeons, cardiologists, anesthesiologists, radiologists, nurse practitioners and physician assistants.
There is also a cardiac hybrid OR that brings a catheterization lab and surgery suite together in one space, making aortic aneurysm treatment more efficient and encouraging collaboration between our expert providers.
“The hybrid OR is a state-of-the-art, innovative, open operating room where patients can receive complex aortic reconstructions—procedures that have open surgery components to them—as well as endovascular (or minimally invasive) aortic reconstructions. This all can take place in one nice operating room,” Dr. Corey said.
The aortic program is part of a larger heart care program at Wellstar, based at Wellstar Kennestone, the first in Georgia and the fourth in the nation to receive Comprehensive Cardiac Care Center Certification by The Joint Commission and American Heart Association. This is the highest certification in cardiovascular care.

Wellstar Ready to Launch Georgia’s First Hospital Care at Home Program
In a first-of-its-kind program for Georgia, Wellstar MCG Health Medical Center is now offering admitted hospital patients the option to receive care from the comfort of their own homes. The new Hospital Care at Home program provides acute, hospital-level care at home for patients admitted to the medical center who meet certain criteria—such as having a qualifying non-life-threatening condition, needing relatively straightforward care and having access to a reliable caregiver, if bedbound.
Emergency department clinicians now assess if their patients need to stay in the hospital or if they can safely receive treatment at home. This treatment involves the use of hospital equipment, two or more daily in-person visits from nurses or paramedics, daily virtual visits from a dedicated provider and 24/7 virtual access to clinicians. Patients admitted to the Hospital Care at Home program receive all necessary medical supplies—including blood pressure cuffs, video communication devices and patches that monitor vital signs—along with healthy pre-packaged meals and training on how to take medications and use equipment.
“This latest innovation shows, once again, how Wellstar and the Medical College of Georgia lead the way in digital health,” Ralph Turner, senior vice president and hospital president at Wellstar MCG Health Medical Center, said. “By maximizing virtual services at our academic medical center, we have the chance to reduce readmissions and open up beds for those who need it most while improving patient and family satisfaction.”
According to the Centers for Medicare & Medicaid Services (CMS), the conditions most often treated by Hospital Care at Home programs include conditions affecting the lungs, kidneys and cardiovascular system, along with infectious diseases.
Patients admitted with severe illnesses requiring urgent attention or continuous IV treatment will stay on-site at the medical center. Because Wellstar Hospital Care at Home patients might occasionally need to return to the hospital for additional support, the care team must be able to respond to a patient’s home within 30 minutes for emergent needs. As a result, geographic boundaries are considered for admission.
Wellstar MCG Health plans to start accepting patients the week of December 2 for admission into its new Hospital Care at Home program. The medical center remains the only hospital in Georgia to have received an approved waiver from CMS to offer acute hospital care at home.
Our ability to offer this care long-term depends on Congressional renewal of the Acute Hospital Care at Home initiative beyond 2024. If passed, H.R. 7623, the “Telehealth Modernization Act of 2024,” would extend the flexibilities that make possible hospital-at-home services for our patients. To date, CMS has approved the waiver for 139 health systems in 39 states.

Wellstar Ready to Launch Georgia’s First Hospital Care at Home Program
In a first-of-its-kind program for Georgia, Wellstar MCG Health Medical Center is now offering admitted hospital patients the option to receive care from the comfort of their own homes. The new Hospital Care at Home program provides acute, hospital-level care at home for patients admitted to the medical center who meet certain criteria—such as having a qualifying non-life-threatening condition, needing relatively straightforward care and having access to a reliable caregiver, if bedbound.
Emergency department clinicians now assess if their patients need to stay in the hospital or if they can safely receive treatment at home. This treatment involves the use of hospital equipment, two or more daily in-person visits from nurses or paramedics, daily virtual visits from a dedicated provider and 24/7 virtual access to clinicians. Patients admitted to the Hospital Care at Home program receive all necessary medical supplies—including blood pressure cuffs, video communication devices and patches that monitor vital signs—along with healthy pre-packaged meals and training on how to take medications and use equipment.
“This latest innovation shows, once again, how Wellstar and the Medical College of Georgia lead the way in digital health,” Ralph Turner, senior vice president and hospital president at Wellstar MCG Health Medical Center, said. “By maximizing virtual services at our academic medical center, we have the chance to reduce readmissions and open up beds for those who need it most while improving patient and family satisfaction.”
According to the Centers for Medicare & Medicaid Services (CMS), the conditions most often treated by Hospital Care at Home programs include conditions affecting the lungs, kidneys and cardiovascular system, along with infectious diseases.
Patients admitted with severe illnesses requiring urgent attention or continuous IV treatment will stay on-site at the medical center. Because Wellstar Hospital Care at Home patients might occasionally need to return to the hospital for additional support, the care team must be able to respond to a patient’s home within 30 minutes for emergent needs. As a result, geographic boundaries are considered for admission.
Wellstar MCG Health plans to start accepting patients the week of December 2 for admission into its new Hospital Care at Home program. The medical center remains the only hospital in Georgia to have received an approved waiver from CMS to offer acute hospital care at home.
Our ability to offer this care long-term depends on Congressional renewal of the Acute Hospital Care at Home initiative beyond 2024. If passed, H.R. 7623, the “Telehealth Modernization Act of 2024,” would extend the flexibilities that make possible hospital-at-home services for our patients. To date, CMS has approved the waiver for 139 health systems in 39 states.

Wellstar Launches Program to Expand Access to Colorectal Cancer Education and Screenings
Colorectal cancer continues to be a critical community health challenge across Georgia, particularly in areas served by Wellstar. High cancer incidence rates are driven by barriers such as limited access to education on screening guidelines, risk reduction strategies and screening resources. This lack of access impacts not only the affected communities but also the organizations working to support them.
To address these challenges, the Wellstar Center for Health Equity and Wellstar Community Health have launched the ColoCare Connect Program, funded by the 2024-2025 Community Health Improvement Plan Partnership Grant from Cobb & Douglas Public Health (CDPH) with support from the Wellstar Foundation. This program aims to improve access to colorectal cancer education and screenings by providing fecal immunochemical tests (FITs) to community clinics serving high-risk populations.
Building on insights gained through previous collaborations, including the #GoodDownThere campaign with BLKHLTH and Cottonelle, this program is designed to overcome obstacles such as low awareness, insufficient health insurance coverage, fear of test results and limited access to resources.
The ColoCare Connect Program focuses on empowering community clinics to seamlessly integrate colorectal cancer screening into their care workflows. This approach supports education, screening and follow-up care, ensuring a more comprehensive and sustainable impact while directly addressing barriers to improve screening rates and outcomes among high-risk and underserved populations.
We are excited to collaborate with the following community clinic organizations on this initiative:
These partnerships will help bring critical screening resources to vulnerable populations while supporting clinics in their mission to provide equitable healthcare.
We are grateful for the commitment of these clinics and look forward to seeing the positive impact of the ColoCare Connect Program in the communities we serve. Together, we are making strides toward reducing the burden of colorectal cancer and advancing health equity across Georgia.

JohnCare
It seems "defeat" just isn't in John Cashen's vocabulary. A survivor in more ways than one, John has overcome not only a catastrophic natural disaster, but also fought cancer with unyielding resilience.
In 2005, as flood waters from Hurricane Katrina rose and threatened his New Orleans home, John took an axe to his attic's ceiling, climbed atop his roof and tied himself to his chimney so he wouldn't be swept away. Days later, no help had arrived, so John untied himself and swam to an overpass where he was rescued by a helicopter. He joined the rest of his family in Georgia.
Since then, John has become a proud citizen of LaGrange. A master of everything Mardi Gras, John runs a local krewe and is a natural at building parade floats from the foundation up. But when he was diagnosed with lung cancer in 2019, he summoned his fighting spirit, squared his shoulders, and faced his cancer journey head on.

First Responders Warn About Dangers of Improper Turkey Frying
In a fiery demonstration on Wednesday, nurses from the Joseph M. Still Burn Centers at Wellstar Cobb Medical Center joined Cobb County firefighters to showcase why it’s essential to be vigilant during the holidays to prevent burn wounds and fires.
News cameras began recording as firefighters in full gear used a long rod to lower a frozen turkey into a fryer full of overheated vegetable oil. Immediately, a violent splash of hot oil spilled from the fryer and burst into a flash flame that extended 5 feet outward and roughly 20 feet high. It would have been a disaster if that scenario had played out during a family’s Thanksgiving feast.
At the demonstration, team members from the Burn Center at Wellstar Cobb told reporters that cooking mishaps are among the most frequent causes of the burn injuries they treat and shared safety tips that can help keep the holidays merry and bright.
“Please be extremely careful while deep frying your turkeys this holiday season,” said nurse Imani Hence of Wellstar Cobb’s inpatient burn unit. “Everyone loves fried turkey, but we have seen a lot of instances where turkey fryers have tipped over, causing significant burn injuries from the grease.”
Burn Program Manager Nadine Lynch said it’s crucial to maintain a “kid-free zone” around cooking areas, whether indoors or outdoors.
“It’s wonderful when the whole family pitches in, but make sure to keep hot liquids away from table edges,” she said. “Use potholders when cooking. Unplug cooking sources when no longer needed and use long-handled tools for grilling and frying.”
Emily Black, clinical coordinator at Wellstar Cobb’s burn, wound and hyperbaric outpatient clinic, said that when kids are out of school during the holidays, more accidents happen.
“We see a great many hand burns from children touching hot stoves, oven doors and glass screens on fireplaces,” Black said. “With kids home and cooking for themselves, we see an even greater number of hot water, tea and ramen noodle burns as well.”
What to do if someone suffers a burn:
What not to do if someone suffers a burn:
The sooner you’re seen at a burn center, Lynch said, the better your outcome.
Turkey fryer fire safety:
What to do if a grease fire occurs:

Support Children’s Health During iHeartMedia Cares for Kids Radiothon
This holiday season, you can support Wellstar Children’s Hospital of Georgia, a Children’s Miracle Network hospital, by tuning in to the 24th Annual iHeartMedia Cares for Kids Radiothon.
Tune into 104.3 WBBQ, 96.3 KISS FM and 105.7 The Bull or watch News12 NBC26 to hear stories of hope, healing and inspiration as patients and families share how Wellstar Children’s has had a positive impact in their lives.
December 5 & 6
6 AM to 7 PM
December 7
8 AM to 1 PM
Wellstar Children’s offers dedicated, world-class care to the youngest patients in our state and beyond. The hospital is home to a 24/7 Pediatric Emergency Room, a dedicated Level II Trauma Center, a Level IV NICU and the only Level I PICU outside of Atlanta.
Giving is easy! Here’s how:
Learn more at caresforkidsradiothon.com.

A Heart for Collaboration: Wellstar Cardiovascular Quality Forum 2024

Wellstar & Someone Cares Team Up to Serve Vulnerable Communities
It’s simple for many of us to find a primary care physician or advanced practice provider that we trust and feel comfortable with. By booking online or making a quick phone call, we can make an appointment and feel confident about the level of care we will receive. We know how and where to get the help we need when we need it.
Many people lack access to care, making their path to high-quality care more challenging. It could be because they don’t have insurance, are unable to pay for medical services or don’t have a way to get to their appointments. This isn’t how it should be.
At Wellstar, we believe every person deserves to live their healthiest life, regardless of their circumstances. The Wellstar Center for Health Equity has partnered with local clinics like Someone Cares to make healthcare accessible to everyone in our communities.
A safe and welcoming space
People who rely on Someone Cares include those who are underinsured or have difficulty accessing healthcare due to transportation or financial issues. The clinic is a one-stop shop that offers care at a brick-and-mortar location in Marietta. Services include:
In addition to their Marietta clinic, Someone Cares has two mobile units. They travel to communities throughout metro Atlanta to provide HIV and STD testing, health screenings, health education and vaccinations. It’s a convenient option that allows people to get the care they need, where and when they need it.
Someone Cares also offers specialized services for individuals in the transgender community, including gender-affirming hormone therapy.
How Wellstar supports Someone Cares
Wellstar and Someone Cares began their partnership in 2023 when the organization was applying to become a Federally Qualified Health Center (FQHC).
FQHCs are community-based centers that receive funds from the federal government to provide primary healthcare services in underserved areas. FQHCs typically work with a hospital or health system to ensure patients have easier access to services that are unavailable in the primary care setting, such as inpatient behavioral health services.
Someone Cares will officially become a FQHC in February 2025. The designation allows them to expand their services, further supporting vulnerable communities.
Each partnership is unique
Someone Cares is one of about a half-dozen clinics in the Wellstar Community Clinic Network. The Wellstar Center for Health Equity launched the network eight years ago to serve the most under-resourced populations in our communities better.
Each partnership is unique and customized to the community-based clinic’s needs. A few examples of the services we provide include:
We’re grateful for our Community Clinic Network partners, who help Wellstar create a healthier Georgia for all. Together, we’re making a difference in people’s lives across the state.
Learn more about the Wellstar Center for Health Equity.

Take the Mystery Out of Menopause with Wellstar
From sleepless nights to hot flashes and brain fog to vaginal symptoms, many women feel isolated or embarrassed about discussing what they go through during menopause. At Wellstar, our compassionate women’s health team provides individualized care to help women navigate this stage of life, demystify menopause and give women back their confidence during this stage of life.
Menopause is defined as the permanent absence of a period for 12 consecutive months. The average age of menopause in the U.S is 52, but generally, women will experience menopause between ages 45 to 55.
Perimenopause is the four- to seven-year period prior to menopause when women are having menopausal symptoms.
“During perimenopause, cycle lengths will vary. Many women experience their periods coming closer together. Hot flashes and night sweats are also common during this transition,” said Wellstar Women’s Health Nurse Practitioner Karin Hulon.
Women may also experience brain fog, mood swings, fatigue, trouble sleeping, skin and hair changes, vaginal dryness, decreased libido, painful sex, joint pain or inability to lose weight. Every woman is unique and may not experience the same severity of symptoms. The menopause experience may be influenced by genetics, race or environmental factors.
The ovaries are the main producers of estrogen. As women age, ovarian follicular function decreases, leading to decreasing levels of estrogen. These levels can also radically decrease due to surgery, infection, medications or radiation.
“Estrogen receptors are found all over our bodies. A decrease in estrogen can affect the part of the brain involved in thermoregulation, resulting in hot flashes and night sweats,” said Wellstar Chief of Women’s Health Dr. Paula Greaves. “Research suggests that women who have hot flashes may be at higher risk for developing heart disease. Additionally, research shows that African American women experience more intense and more frequent hot flashes for a longer duration.”
Estrogen receptors are located in the vagina, vulva, bladder and urethra, helping to maintain blood flow, tissue turgor and microbial balance. Therefore, a decrease in estrogen can lead to vaginal dryness and atrophy, making intercourse painful. The pH of the vagina also changes with decreased estrogen, increasing the risk of infections or urinary leakage.
These are only some examples of how menopause can impact women’s health and quality of life, and it’s important to treat menopausal symptoms as soon as possible.
Your care team will discuss your concerns and health history to tailor a safe, personalized plan that fits your needs. The choice should be guided by symptoms, medical history, contraindications and shared decision making. There are FDA-approved hormonal as well as non-hormonal options for treatment of hot flashes, vaginal dryness, painful intercourse and even decreased libido.
“We must promote lifestyle changes such as smoking cessation, weight loss and cognitive behavioral therapy, which can help decrease symptoms,” said Dr. Greaves.
“Women: You need your mammograms and your health and cancer screenings, including Pap smears until age 65. Women who have had abnormal Pap smears in the past may need to continue Pap smears beyond age 65,” Hulon said. “Even if you’ve had a hysterectomy and you no longer have a uterus, you still need to ensure pelvic floor health.”
If you experience vaginal bleeding after menopause, schedule an appointment with your women’s health care team.
“The cause of bleeding could be something as simple as vaginal tearing due to dryness or as serious as endometrial cancer,” Hulon said.
Whatever your health concerns may be, Wellstar will partner with you to help you stay healthy. Other diseases can masquerade as menopause, so if something is worrying you or stopping you from feeling your best, mention it to your clinician.
“For example, if you start having joint pain, that may not be menopause. That may be arthritis. Fatigue, weight gain or night sweats may be a sign of thyroid disease, not menopause,” Dr. Greaves said. “Trust and open communication have been instrumental in aiding gynecologists to uncover other diseases affecting our patients who assumed they were menopausal.”
Wellstar OB/GYN clinicians specialize in addressing the health needs of women and are experienced in caring for people going through menopause.
“It is important when you’re looking for a clinician to find someone who specializes in women’s health and who has a passion for treating women entering the menopause transition,” Hulon said. “Find someone who will listen to you, not dismiss you, will make you feel comfortable and treat you as an individual.”
While troubling symptoms of menopause may be common, you don’t have to go through it alone.
“With increasing life expectancy, women will spend more than 40% of their life in this life stage. Therefore, we need to focus our efforts in providing a smooth transition for every woman into menopause so she can enjoy her best years yet,” Dr. Greaves stated.
Wellstar Women’s Health offers compassionate care through menopause, answering your questions and helping to manage your symptoms. Many of our clinicians are certified menopause practitioners. Find a Wellstar OB/GYN location near you.

Wellstar Team Members Tackle Hunger and Housing Challenges
More than 450 Wellstar team members fanned out across metro Atlanta, West Georgia, Augusta and beyond on November 14, volunteering their time to improve access to healthy food and housing by supporting 20 local, community-based organizations.
They packed and distributed food, assisted in community gardens, and sorted food and clothing donations.
“It warms my heart to see so many team members participating in our annual Day of Service,” said Candice L. Saunders, president and CEO of Wellstar Health System. “As a nonprofit, community-based health system, our mission is to enhance the health and well-being of every person we serve, and it’s always exciting to expand that mission outside the walls of our facilities.”
Wellstar volunteers participated in service projects for the following nonprofit organizations: Atlanta Community Food Bank (Atlanta and Marietta), Covenant House (Atlanta), Douglasville Community Garden (Douglasville), The Drake House (Roswell), Feeding the Valley Midland Warehouse (Muscogee County), Five Loaves & Two Fish Food Pantry (Griffin), Food Well Alliance – Roswell UMC Giving Garden (Roswell), Golden Harvest Food Bank (Augusta and Aiken, S.C.), Helping Hands of Paulding County (Dallas), LaGrange Personal Aid (LaGrange), MUST Ministries (Marietta Donation Center and Mobile Pantry at the VA Clinic), North Fulton Community Charities (Roswell), Our Giving Garden (Mableton), The Salvation Army (Atlanta, Griffin and Marietta), Sweetwater Mission (Austell) and the Warehouse of Hope (Douglasville).

Kennesaw State and Wellstar Double Nursing Student Enrollment
KENNESAW, Ga. (Nov. 12, 2024) — Kennesaw State University (KSU) and Wellstar Health System have doubled the number of students at KSU’s Wellstar School of Nursing in the last four years, helping to fill the need for more nurses in Georgia.
The nationwide shortage of nurses is hitting Georgia particularly hard. Georgia currently has 21 percent fewer registered nurses than it needs and is expected to see the second-highest estimated shortage in the U.S. by 2035, according to the federal Health Resources Service Administration (HRSA).
“Our partnership with Wellstar not only enhances the educational opportunities for our students, but also makes a significant impact on the future of healthcare in Georgia,” said Kennesaw State President Kathy S. Schwaig. “Together, we are ensuring that more nurses are entering the workforce, highly trained and dedicated to providing essential care and support.”
To grow KSU’s Bachelor of Science in Nursing enrollment, Wellstar in 2020 committed nearly $9 million over five years to fund nursing scholarships and the hiring of new nursing faculty and staff. As a result:
“At Wellstar, we have a responsibility to create pathways for our communities’ future healthcare workers,” said Candice L. Saunders, president and CEO of Wellstar Health System. “By working closely with Kennesaw State, we’re helping more students pursue medical careers through scholarships and the additional faculty to teach them. This collaboration is critical to help meet Georgia’s need for more healthcare workers.”
The Wellstar scholarships at KSU can be combined with the state-provided HOPE and Zell Miller Scholarships, which are helping thousands of Georgia students attend an in-state four-year college or university, as well as other tuition assistance. Wellstar also offers its nurses and other clinical team members tuition reimbursement for ongoing education at KSU throughout the career.
“Wellstar Health System’s generous support directly addresses the critical nursing workforce need,” said Monica Swahn, dean of KSU’s Wellstar College of Health and Human Services. “Our commitment to excellence has remained steadfast, and as we look to the future, we will continue to lead and innovate in shaping the next generation of nurses.”
According to the U.S. Bureau of Labor Statistics, nurses in metro Atlanta earn on average about $45 per hour, or $95,000 per year plus benefits, depending on their area of specialty.
The longstanding KSU-Wellstar partnership’s success supporting community health and well-being is outlined in the 2024 Wellstar School of Nursing annual report.
Kennesaw State has been collaborating with Wellstar for decades. Wellstar currently manages the University’s on-campus student health clinics and is the named donor of the College of Health and Human Services and its School of Nursing.
Wellstar, on top of its previous $18 million in contributions to KSU, recently committed $25 million to expand the relationship. Wellstar provided the lead funding commitment for a new state-of-the-art training and conditioning complex for KSU student-athletes, pending approval by the Board of Regents of the University System of Georgia, along with a new Center for Research on Human Sport Performance and Wellbeing. Beginning July 1, 2026, Wellstar will be the exclusive orthopedics and sports medicine provider, partner, and sponsor of the KSU Athletics Association, providing key services for Kennesaw State student-athletes.

Wellstar Georgia Cancer Center’s Pharmacogenomics Program may Help Reduce Side Effects From Chemotherapy for Some Patients
The Wellstar Georgia Cancer Center Pharmacogenomics Program (CaPP) has launched pharmacogenomics testing services for the center’s patients and oncologists. Pharmacogenomics employs genetic sequence alterations in drug metabolism genes to predict toxicity.
The tests measure changes in genes that make proteins that metabolize common chemotherapy drugs. If a patient has a mutation in these genes, their metabolism will not handle the drug properly. This may cause the patient to become sick.
“These tests can help people avoid severe toxicity from chemotherapy. We want to optimize treatment for patients who need a lower dose when they have any gene mutation,” said Dr. John W. Henson, director of neuro-oncology at the Medical College of Georgia and the Wellstar Georgia Cancer Center. The Pharmacogenomics Program is co-led by Henson in the Hereditary Cancer Clinic and Dr. Katherine Saunders-Wohlfrom in Oncology Pharmacy.
The program’s initial focus will be on patients with gastrointestinal cancers in conjunction with Dr. Asha Nayak. Henson said this is where the biggest impact will come right away. Other service lines, including breast cancer, will benefit as more testing is done.
“This is a valuable message to the community,” said Henson. “CaPP services will include testing support, report interpretation, document management, clinician consultation, and patient and family consultation.”
Henson also thanked Dr. Brandy D. Gunsolus in Clinical Laboratory Science for her help with the program, saying she was instrumental in developing the order process.

Wellstar Experts Collaborate to Help People Fight Lung Cancer
From catching cancer to following through with expert care, Wellstar ensures patients never have to fight lung cancer alone.
Wellstar is dedicated to early intervention in lung cancer, which improves outcomes for patients. After detection of an abnormality on a CT scan, patients are immediately surrounded with an interdisciplinary support team devoted to their well-being.
If you are at increased risk for developing lung cancer, talk to your care team about screenings. With a low-dose CT scan of the chest, it only takes a few seconds to check in on your lung health. These screenings are offered at several Wellstar imaging centers.
The United States Preventive Services Task Force has revised lung screening guidelines. Patients may qualify for screening if they are 50 to 80 years old and smoked for 20 years. If they are a former smoker, they may qualify if they quit less than 15 years ago.
“Lung screening improves a person’s chances of detecting a lung cancer at an early stage and being cured of that cancer,” said Wellstar Thoracic Surgeon Dr. William Mayfield.
Because finding cancer and starting treatment sooner can be life-saving, Wellstar has invested in the incidental nodule program. When people come into a hospital seeking care for something else—whether that be a health condition like appendicitis or a traumatic event like a motorcycle accident—they might get a scan of the abdomen or chest that also shows portions of the lungs.
Using artificial intelligence, reports of those scans are fed to report coordinators, categorized based on their risk level, and if the patient is higher-risk, forwarded to nurse navigators for review. Nurse navigators consult with physicians about the findings, and Wellstar can then initiate care if cancer is found.
“People that come to the hospital for other problems may also be walking around with a lung cancer they didn’t know about,” Dr. Mayfield said.
The program, which started in fall 2020, has identified a total of 148 lung cancers and 14 other types of cancer, as of October 2024.
“Now those people are getting care, and it’s quite likely those cancers would have been missed,” Dr. Mayfield said.
Wellstar is developing another incidental nodule program for the abdominal area, which could lead to the discovery of several cancers including ovarian, kidney, bladder and liver cancers.
The program aligns with the Wellstar mission of enhancing the health and well-being of every person we serve.
“It was the right thing to do for the community. If we miss these cancers, it is a broken promise to the patient,” Dr. Mayfield said.
Then, if cancer is found, Wellstar “closes the loop” by initiating treatment and connecting the patient with resources, Dr. Mayfield said.
From the very beginning, lung cancer patients at Wellstar are surrounded by a team of experts. Rather than go through the time-consuming process of driving to multiple appointments with different specialists, patients meet with all these physicians in one place.
The Wellstar Lung Cancer STAT Clinic, at Wellstar Cobb, Douglas, Kennestone Regional, North Fulton and Paulding medical centers, as well as the Thoracic NOW Clinic at Wellstar MCG Health Medical Center, give patients immediate access to specialists in medical oncology, radiation oncology, pulmonary medicine and thoracic surgery.
“No other health system does multidisciplinary care the way Wellstar does,” Dr. Mayfield said.
Getting multiple expert opinions from the start not only gives patients peace of mind, it speeds up treatment, too. In the United States, the average time between an abnormal scan and the beginning of treatment is 95 days, Dr. Mayfield said. The STAT Clinic reduces that time to as little as 14 days. Time-to-treatment affects long-term survival in lung cancer patients, Dr. Mayfield said—a six-week delay can reduce five-year survival by up to 13%, according to research from the Cleveland Clinic.
“Time really does matter in the treatment and diagnosis of lung cancer,” Dr. Mayfield said.
For many patients, surgery is a crucial part of lung cancer treatment. Wellstar offers several minimally invasive options, reducing recovery time for patients.
Dr. Mayfield said more than 90% of lung cancer surgeries at Wellstar are performed using either the da Vinci Surgical System or Video Assisted Thoracic Surgery techniques (VATS).
Minimally invasive surgeries reduce pain, scarring, blood loss and infection, as well as time to recover—getting patients back to work and other routines quicker.
The da Vinci system is equipped with 3D cameras and instruments that can make very intricate, precise movements, allowing for shorter incisions and more accurate surgery. Some patients can leave the hospital as early as the next day.
For biopsies, Wellstar has completed 500 procedures using the Ion system, a robotic-assisted platform.
To prevent lung cancer and keep your lungs healthy, talk to your primary care team and follow a few tips, such as avoiding smoking and getting your exercise. Learn more about treatments on our cancer care page.

Grant Provides No-Cost Support for Pregnant Women and New Parents in Three Georgia Counties
Lead Khristen Flennoy is on a mission. As the new director of the Wellstar Healthy Start program, she wants to enroll hundreds of women in Butts, Spalding and Troup counties in a program that cares for mothers and babies before, during and after childbirth.
“There is a great need to expand women’s health services in Butts, Spalding and Troup counties, and we’re grateful for the resources the Healthy Start grant provides,” said Flennoy. “After an extremely competitive application process, Wellstar is now part of Healthy Start’s 33-year legacy of improving the health of women and families. I am ecstatic to lead the charge alongside a dynamic team to create a lasting impact for the people in these communities.”
For the first time in her new role, Flennoy led a community consortium meeting on Friday, October 25. The group was formed to serve as a voice for the community after Wellstar received the $5.5 million Healthy Start federal grant from the U.S. Department of Health and Human Services’ Health Resources and Services Administration. The highly competitive grant invests in communities to improve health outcomes before, during and after pregnancies.
According to the Georgia Department of Health, maternal deaths during pregnancy are increasing. Black women are twice as likely as white women to die from pregnancy-related causes. Wellstar is the first grant recipient in the state to embed the Healthy Start program in its OB/GYN offices.
Participants include pregnant women, new moms of babies up to 18 months old, and fathers and other caregivers. So far, more than 50 participants in Butts, Spalding and Troup counties have signed up. Many are already receiving the services at no cost, which include case managers, nurse navigators and doula services, as well as classes on pregnancy and infant care, parenting and nutrition. The grant also covers transportation needs.
“This grant allows us to better connect clinical expertise with community support to improve the health of women and families in Georgia counties that have the greatest need," said Preston Hendrickson, assistant vice president of Women’s Health at Wellstar. “We’re thrilled about the opportunities that the Healthy Start grant will make available to families that live, work and play in Butts, Spalding and Troup counties.”
A family’s income or insurance status does not factor into who qualifies. Any expectant or new parent can receive care through the program. To apply, fill out the confidential questionnaire at wellstar.org/healthystart.
This article is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $5.5 million with 0% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS or the U.S. government.

Make Lung Health Your Habit
Whether you’re running a marathon or simply running errands, having healthy lungs helps you to live comfortably and do the activities you enjoy.
Lung health is an important part of overall wellness. It’s best to prevent health issues before they start, and Wellstar experts will partner with you to personalize a plan to keep your lungs healthy.
Book an appointment online to check in with a provider about your lung health and follow these tips to breathe a little easier.
If you are a smoker, keep in mind that there are both short-term and long-term benefits to quitting. One to nine months after the last cigarette, your shortness of breath should decrease. Within 10 years of quitting, a former smoker's risk of developing lung cancer is 30% to 50% below that of a person who continues to smoke.
Also, if you don’t smoke, do not pick up the habit. Nicotine is highly addictive, even more so than many other drugs including narcotic opiates, according to Wellstar Pulmonologist Dr. Hitendra Patel.
Dr. Patel said that vaping is gaining popularity, especially among younger people. However, vaping irritates a person’s airways and increases their risk of asthma.
“Nothing but air should go in and out of the lungs,” Dr. Patel said. “Any other chemical or substance, or inhalation of smoke of any kind, is going to be detrimental and harmful.”
Wellstar Primary Care Physician Dr. Jignesh Dholaria said misinformation about vaping is common.
“People have the notion that vaping is somehow safer and that it doesn’t have the same chemicals that cigarettes do,” Dr. Dholaria said. “We’re seeing a lot more harmful effects from vaping just because we don’t always know all the chemicals that are in these vapes. That has caused a lot more lung-related injuries.”
While staying active is a critical component of overall wellness, it’s especially important to keep your lungs in top shape.
“As you’re breathing in and out, getting rid of carbon dioxide and inhaling more oxygen, that helps your tissues, which helps you feel better overall,” Dr. Dholaria said.
Even if it is raining—or if pollutants are especially high that day and you’re worried about lung irritation—there are ways to get your steps in. Dr. Patel recommends going to an air-conditioned shopping mall or store to get some exercise if being outside is not an option.
“Continuing to exercise to the fullest of your body’s ability is an important step of maintaining whatever lung health you have,” Dr. Patel said. “If you start with healthy lungs, staying on an exercise program and regimen is vital.”
Balance that exercise with some rest, too. Dr. Patel, who is also the medical director of the Wellstar sleep program, said being well-rested can ward off sickness, including some respiratory illnesses.
“If you don’t sleep well, that means your immune system is not going to function as well as it should,” he said.
In addition to getting your sleep, some relaxation and breathing techniques can have benefits for both mental wellness and lung health.
Dr. Patel recommends “4-7-8 breathing,” which involves inhaling for four seconds, holding your breath for seven seconds and then exhaling for eight seconds.
Benefits of breathing exercises may include lower stress and anxiety levels, lower blood pressure and better sleep.
If you have asthma, know your lungs and avoid the environmental triggers that cause the condition to flare up, Dr. Patel said. Common triggers include pet dander, seasonal changes, allergens like perfume and smoke inhalation.
Asthma can also run in families, although there is often no specific reason why a person develops asthma, Dr. Patel said.
“Sometimes people underestimate how bad asthma can be,” Dr. Patel said.
If you have asthma, see your primary care physician to monitor your lung health. Pulmonologists specialize in caring for people’s lungs, and they often collaborate with primary care clinicians to create personalized plans to manage their patients’ asthma.
Early detection is key in cancer treatment, but many lung cancers present in later stages, Dr. Patel said.
“In that area in the middle of the lungs and the middle of the chest, there are no pain fibers or pain sensors in there,” Dr. Patel said. “If a tumor occurs there, patients don’t know it. They don’t feel it, and it doesn’t hurt them.”
Lung cancer is sometimes found when it spreads and causes complications, Dr. Patel said.
If you are at increased risk for developing lung cancer, ask your care team about screenings. You should consider screenings if you are a current or past smoker. Visit our lung cancer screening page to learn more about if screening, which involves low-dose CT scans, could benefit you. To keep up with your lung health, find a Wellstar physician near you.

Wellstar Offers Saturday Hours for Lung Cancer Screening Day November 9
Lung cancer screening can detect cancer earlier, before symptoms show up. Earlier-stage cancers are more easily treatable and more frequently cured, so if you are at increased risk of developing lung cancer, you could benefit from regular low-dose CT scans to monitor your lung health. To expand access to these vital screenings, Wellstar will offer screenings at several imaging locations on Saturday, November 9.
“Lung screening improves a person’s chances of detecting a lung cancer at an early stage and being cured of that cancer,” said Wellstar Thoracic Surgeon Dr. William Mayfield.
Wellstar is partnering with the American Cancer Society National Lung Cancer Roundtable, the American College of Radiology, the Radiology Health Equity Coalition, and GO2 for Lung Cancer to celebrate National Lung Cancer Screening Day Saturday, November 9. While lung scans are always available at Wellstar’s conveniently located imaging centers during regular business hours, offering these Saturday hours will help patients fit screenings into their schedules.
Ask your care team about whether you meet the criteria for screening, or call to learn more about qualifying and to schedule a scan.
Call us to learn more and make an appointment for a scan:
The following Wellstar imaging locations will be open Saturday, November 9:
In addition to these special hours November 9, low-dose CT lung scans are available at several Wellstar imaging locations.

Lung Biopsy Technology at Wellstar Reduces Complications, Speeds Up Treatment
Innovative technology at Wellstar is offering patients a minimally invasive option for lung biopsies, reducing complications and helping expedite lung cancer treatment.
The Ion system is a robotic-assisted platform for performing lung biopsies. If a lung cancer screening or any other CT scan shows a suspicious nodule, providers will need to perform a biopsy to determine if the patient has lung cancer and how to proceed with care.
“Those nodules may not be cancer, but in certain situations we still need to know what it is,” said Wellstar Pulmonologist Dr. Timothy Udoji. “The Ion technology helps us biopsy those nodules to get an answer so that additional workup can be done immediately. If it is cancer, we want to catch it at an early stage.”
The system uses a three-dimensional spatial recognition technology that helps guide a catheter down the airway, deep into the lung, all the way to small nodules where biopsies can be performed. The robotic catheter maintains its shape and stability throughout the biopsy process significantly improving diagnostic yield compared to other modalities.
“The better the image and the more certainty we have of the spatial location of the catheter, the better we can avoid complications by making sure we are not too close to a blood vessel or the edge of the lung,” said Wellstar Thoracic Surgeon Dr. Daniel Fortes.
During the biopsy, providers can also use the Ion system to mark an area in the lung, making it easier to find later during surgery.
“If something is very small and hard to find in surgery, Ion can be used to mark that area with dye, or contrast, that allows us to find it in surgery,” Dr. Fortes said. “With this technology added to the surgical robotic system in the operating room, we can better identify those lesions and remove smaller portions of lung, also called segments.”
The Ion system also has further reach than previous technologies and is able to more easily biopsy nodules in the peripheral areas of the lung. For many cancer patients, this will allow them to initiate care earlier and improve their outcomes, as well as give them peace of mind during the treatment process.
“Mental health impacts physical health. We are able to confidently biopsy and identify these nodules and that means a lot for our patients,” Dr. Udoji said. “Now, with this new technology we are able to get a biopsy done much earlier which has huge outcome implications for malignant nodules.”
At Wellstar, cancer care is tailored for each patient. In the Wellstar STAT Clinic for Lung Cancer, patients meet with multiple specialists at once to discuss their care options and create a personalized treatment plan. Specialists in the STAT Clinics, which are located at Wellstar Cobb, Douglas, Kennestone Regional, North Fulton and Paulding medical centers, work with patients to determine the optimal course of treatment and will talk with patients and families about biopsy options, including the Ion system. The STAT Clinics give patients the opportunity to have their diagnoses managed right away, and literature shows that the clinics’ diagnostic and treatment model improves outcomes for patients.
The Ion system is currently in use at Wellstar Kennestone Regional Medical Center, where the team has completed 500 procedures. Learn more about lung cancer care at wellstar.org/lungcancer.

Partner with Wellstar Center for Genetics to Reduce Your Risk of Cancer
While the cancer care experts at Wellstar are dedicated to providing world-class cancer treatment, our care teams are also committed to preventing disease and helping you evaluate your risk so you can be proactive with your health.
Some patients may have an increased risk of developing cancer if they have a family history or a genetic mutation. For example, a family history of prostate cancer could be indicative of a genetic mutation that increases the family’s risk for breast cancer, and vice versa. The Wellstar Center for Genetics determines if you may develop or carry certain genetic disorders. Using a compassionate approach, Wellstar genetic counselors ensure patients have the information they need to make an educated decision about genetic testing. Our team supports you every step of the way, answering questions and often working through complicated emotions.
At Wellstar, our focus is PeopleCare—personalized healthcare tailored uniquely for you. Your care team will ask you about your family’s history of cancer, including if you have had any relatives with cancer. If you do have a family history, they will ask how old your family members were when they got diagnosed.
If you have a family history of cancer, your doctor might recommend you start screenings such as mammograms or prostate-specific antigen tests earlier or get screened more frequently. Your care team may also suggest preventative measures like medications or lifestyle changes, and they’ll partner with you to take action against potential cancers.
Some possible signs of hereditary cancer include:
Your care team may evaluate your risk of hereditary cancer by looking at your BRCA genes. Mutations in the BRCA1 or BRCA2 genes are most commonly associated with breast cancer, but they are also tied to an increased risk of several other cancers, including ovarian, pancreatic and prostate cancers. A BRCA gene mutation can also make a man more likely to develop breast cancer.
“Since these genetic mutations can affect someone’s risk for several different types of cancer, it’s important that you discuss any family history of cancer with both your relatives and your Wellstar care team,” Wellstar Urologist Dr. Justin Watson said.
These conversations can be beneficial to both you and your family members.
“Men diagnosed with prostate cancer at an early age may pass along a higher genetic risk for both prostate and breast cancer to their children,” Dr. Scott Miller, Wellstar Urology specialty lead and director of robotic surgical services, explained. “Understanding these risks empowers families to take preventive steps earlier and opens the door to targeted screening programs.”
If you are wondering if you may have a genetic predisposition to certain cancers, the Wellstar Center for Genetics has nine convenient locations, and our genetic counselors can help you learn more about your risk. Your physician can refer you for genetic testing, or you can contact the genetics team directly to make an appointment. In an initial 45-minute appointment, your genetic counselor will meet with you to review your family history and discuss testing options. Most testing can be done with a saliva sample.
Genetic testing is one way that families can work to protect and inform each other so everyone can reduce their cancer risk. “The whole family is in this together,” Kimberly King-Spohn, director of the Wellstar Center for Genetics, said. “Testing helps us manage their risk and know what they're at risk for, and it's an opportunity for prevention.”
To learn more about the Wellstar Center for Genetics or make an appointment, call (470) 793-7472.
.jpg?rev=e49b00e4e51e434aaf29b244ed69b74b)
Wellstar Announces Redevelopment Vision for Former Atlanta Medical Center Site
ATLANTA, Ga., Oct. 17, 2024 – Wellstar Health System announced today that redevelopment of the former Atlanta Medical Center campus is set to begin in the coming weeks, led by The Integral Group and guided by the land-use plan unanimously approved by the Atlanta City Council last month with support from Atlanta Mayor Andre Dickens.
“We will work closely with the city to build on its revitalization plan and bring to life our shared vision of a thriving, healthy addition to the Old Fourth Ward,” said Candice L. Saunders, president and CEO of Wellstar Health System.
To lead the redevelopment process, Wellstar has engaged The Integral Group, a nationally recognized, Atlanta-based firm that specializes in creating spaces that reflect the needs, character and history of their community.
The City of Atlanta placed a zoning moratorium on the property in 2022 and renewed it three times, most recently in June 2024. The moratorium expired October 15, 2024.
“For nearly two years, our administration has worked with purpose and intent on a thoughtful plan for the next chapter for this property,” said Mayor Dickens. “Through direct engagement with the Old Fourth Ward and surrounding stakeholders, we now have an opportunity to create an inclusive, forward-looking and thriving new development that meets the community’s needs for affordable housing, green space and safe streets—while maintaining some medical use and retaining the neighborhood’s unique character. I appreciate Wellstar moving forward with this community-driven project while our administration continues to explore options to meet the healthcare needs of residents on the Southside.”
The vision for the 22-acre campus includes a vibrant, diverse mixed-use neighborhood with affordable housing, residential properties, community and public green space, neighborhood-level retail, new street access, commercial uses, and health and well-being resources.
“At Integral, we believe that transforming a community requires more than just development—it requires a commitment to understanding and addressing the core needs of the people who live there,” said Egbert Perry, chairman of The Integral Group. “This project is a tremendous opportunity to create a lasting impact. It will honor the history of the area while shaping a vibrant, sustainable future.”
The nature of the health and well-being component will be determined in collaboration with community stakeholders as part of Integral’s comprehensive planning process and will include an in-depth analysis of the area’s healthcare needs.
Over the next few weeks, Integral will develop an implementation plan and engage with neighbors and community stakeholders to gather further feedback. The revitalization effort will take place in phases over several years, with community input at every stage. In response to the neighborhood’s desire to see progress quickly, Integral expects to apply for permits soon with the goal of beginning demolition of certain aging structures in the first quarter of 2025.
“This is a long-awaited new beginning for the Old Fourth Ward community," said Atlanta City Councilor Amir Farokhi. “These properties have enormous potential to meet our city’s and the neighborhood’s need for more dense, mixed-use development, including, hopefully, new housing.”
“The Old Fourth Ward sits at a crossroads of our city. This is a vital investment in the growth and advancement of this historic neighborhood for the betterment of all who live here,” said Tom Boyle, president of Old Fourth Ward Neighborhood Association. “We are ready to move ahead quickly with the next steps for this site and we are eager to work together throughout all phases of this project.”

Wellstar Partners with Social Cascade to Tackle Health Inequity Through Technology
The Wellstar Center for Health Equity has teamed up with Social Cascade, a health literacy platform designed to modernize patient education, to address health inequities across Georgia. This partnership is part of Wellstar’s Community Transformation Program and represents a shared commitment to improving health outcomes by using technology to bridge the gap between healthcare providers and patients. However, the partnership is about much more than what can be accomplished through technology; it is about empowering patients and making meaningful progress toward health equity.
At Wellstar, we have long believed that every person deserves the opportunity to live their healthiest life, regardless of their circumstances. The Center for Health Equity is committed to making healthcare accessible, equitable and dignified for everyone in Georgia. By implementing systemwide programs that address health disparities, Wellstar is creating lasting change across the state. Now, Social Cascade joins us in championing this important work that ensures everyone can access quality care, regardless of their background or circumstances.
A collaborative approach to health equity
Improving health inequities requires teamwork. No organization, policy or program can solve these complex issues alone. Wellstar’s new partnership with Social Cascade uses a collaborative approach to make a meaningful difference in the community.
Here’s how it works: Wellstar has identified five Georgia-based clinics and advocacy organizations focused on reducing health inequities. Social Cascade will give those clinics full access to its innovative AI-powered solutions to help them more easily reach the patients they serve and strengthen patient engagement. The five participating organizations are:
These clinics and advocacy organizations serve some of the most vulnerable populations, offering crucial services to individuals and families who may face barriers to healthcare access. Together, Wellstar and Social Cascade aim to amplify their reach, ensuring their patients receive timely, accurate health information through the social media platforms they already use.
Leveraging technology to improve health outcomes and access
Many individuals struggle to find, understand and apply health-related information, leading to poor health outcomes and difficulties navigating an already complex healthcare system. Social Cascade’s role is to help improve this situation by making health information more accessible and actionable for patients through the organizations and providers patients already know and trust.
With Wellstar’s support, Social Cascade will help participating groups:
Both Wellstar and Social Cascade envision a future where organizations across Georgia can more easily connect with their patients, improve access to care and positively impact the social determinants of health in their communities over time. Our organizations look forward to sharing the positive outcomes of this partnership and continuing to drive change in healthcare through innovation and collaboration.

Dr. Earl Stewart Jr. Takes on New Role as Medical Director of Health Equity, Committed to Improving Healthcare Access and Inclusivity
We are pleased to announce that Dr. Earl Stewart Jr. has accepted the role of medical director of health equity at Wellstar.
Dr. Stewart, a native of Augusta, graduated with honors from Mercer University and Meharry Medical College. He completed his internal medicine residency at Brown University. His clinical interests include heart disease prevention, the effects of the environment and climate on health, health equity and the connection between spirituality and medicine.
He is a fellow of the American College of Physicians and a member of the National Medical Association, the American Association for Physician Leadership and the Arnold P. Gold Foundation for Humanism in Medicine. He actively serves in various capacities at both the state and national levels with these organizations.
"Growing up in Augusta, I saw family members in rural areas near Augusta struggle to access healthcare,” Dr. Stewart said. “That experience shaped my desire to improve access to care, which remains a key driver for me today."
His passion for making a difference is rooted in the belief that everyone should have access to the care they need, no matter where they live or their background. This personal connection continues to fuel his dedication to creating more inclusive healthcare.
"Many of us from underrepresented groups pursue medicine to advocate for equitable healthcare for those with similar experiences,” said Dr. Stewart on the importance of community care. “Despite advancements in care, these issues still persist."
In his new role, Dr. Stewart will partner with executive leadership and nursing teams to develop strategies for fostering diversity, equity and inclusion at Wellstar, leading initiatives to improve patient experiences, enhance cultural competency, boost employee engagement and strengthen community partnerships.
Dr. Stewart emphasized collaboration and innovation saying, "We are working to implement the PREVENT (Predicting Risk of cardiovascular disease EVENTs) tool to more accurately assess cardiovascular risk for patients,” he said. “We are also gearing up for the 2025 Community Health Needs Assessment to improve care, clinician data resources, and partnerships focusing on addressing the health care needs for all we serve, especially underserved groups."
Additionally, Dr. Stewart will help guide the Wellstar Center for Health Equity in addressing social determinants of health and reducing disparities.
"Improving diversity, equity and inclusivity in healthcare is no longer optional for health care systems—it's a requirement,” said Dr. Stewart. “Accreditation, certification and reimbursement all depend on it and we must embrace this new reality."
Reflecting on his roots, Dr. Stewart is ready to give back to the community he grew up in. "I'm thrilled that these initiatives will extend to Wellstar MCG Health Medical Center, Wellstar Children's Hospital of Georgia and Wellstar Georgia Cancer Center in Augusta, where I first learned the ropes and prepared for a career of practicing medicine."

Wellstar MCG Health to Offer Blood Test That Can Detect More Than 50 Types of Cancer
In 2023, an estimated 610,000 people will die of cancer in the U.S. It’s the second leading cause of death in the nation, just behind heart disease.
That’s partly because detecting cancer early is essential to treating it. Yet recommended screenings like mammograms, Pap tests and colonoscopies only screen for a handful of individual cancers.
That’s why the new Galleri Multi-Cancer Early Detection (MCED) blood test being offered at Wellstar MCG Health Medical Center is revolutionary. It can detect more than 50 kinds of cancer using about 1.5 tablespoons of blood.
Dr. Brandy Gunsolus, who oversees pathology utilization for Wellstar MCG Health, said the vast majority of the cancers Galleri can detect don’t currently have any other type of screening method. This is particularly important for more lethal cancers that aren’t typically caught until later stages, she said.
“To be able to catch a Stage II or even a Stage I ovarian cancer or pancreatic cancer, which you typically don’t catch until Stage IV, is completely life-changing,” she said. “It gives patients an increased chance of survival.”
In addition to looking for cancerous cells to determine if cancer is present, the test can also indicate in which organ system the cancer likely started. This lets the doctor know which additional tests to perform to verify the presence of cancer, such as a CT scan of a patient’s lungs.
The Galleri test development was supported by what is believed to be one of the largest study programs in genomic medicine, with more than 20,000 participants at more than 140 clinical study sites, including the Mayo Clinic, Cleveland Clinic and Dana-Farber Cancer Institute. Its false-positive rate—the rate in which the test detects a cancer signal when there is no cancer present—is 0.5%.
Gunsolus said she started vetting the Galleri process this past spring. Wellstar MCG Health is the first hospital in Georgia to offer the test.
“It’s a process where pathology looks at the lab and the test itself to ensure it’s a legitimate test and not a scam,” she said.
While the test is a breakthrough, Gunsolus said she isn’t expecting high demand at the start because the test is not currently covered by insurance, although that’s expected to change in the next 12 to 18 months. The test is offered at a discounted rate of $799 for patients at Wellstar MCG Health. The regular price is $950 for patients outside of the health system. However, patients can use funds from their FSA or HSA to pay for the test, and a payment plan is available.
“Even though insurance doesn’t cover it yet, we wanted to go ahead and offer it for individuals like me who are very high risk,” she said. “This is a life-changing screen.”
Gunsolus said she plans to take the test because her four grandparents died from cancer, and her father has cancer.
“I’m willing to put out additional money until the test is covered because it’s not a matter of if I get cancer, but when,” she said.
The Galleri test is recommended for those 50 or older at elevated cancer risk. Those interested in taking the test can call (706) 721-9335.

Wellstar Offers Life-Changing Adult Scoliosis Surgery
Scoliosis is a sideways curve of the spine. It can develop in adults, often due to changes in the spine, such as disc degeneration, arthritis or osteoporosis. While many adults with scoliosis may not need treatment, surgery may be necessary in severe cases where the curve causes significant pain, limits movement or leads to deformity.
This type of surgery, called spinal deformity correction, is a complex procedure performed by a neurosurgeon. The goal is to realign the spine from the neck to the hips, both front-to-back and side-to-side. Dr. Ben Zussman, a Wellstar neurosurgeon at Wellstar North Fulton Medical Center, is one of the few specialists in Georgia who performs this life-changing surgery.
“Adult degenerative scoliosis often develops slowly, causing someone with a previously straight spine to become increasingly crooked,” Dr. Zussman explained.
Common signs that might lead to considering surgery include:
These symptoms occur because the spine's unnatural curve forces the body to adjust, which can change posture and make it hard to stay upright. “Without a good center of gravity, your body begins to lean, which is exhausting,” says Dr. Zussman. When pain and limited mobility significantly affect daily life, scoliosis surgery can help improve movement and quality of life.
By age 50, Cynthia Clark’s spine had become so crooked that she could no longer stand upright. A CT scan taken just eight years earlier showed a straight spine, but degenerative scoliosis had progressed quickly, causing intense pain and difficulty walking.

Dr. Zussman offered Cynthia surgery to relieve her severe symptoms, explaining the complexity and long recovery process. Although she was nervous, Cynthia reached a point where she felt she couldn’t continue living in such pain.
Before surgery, Dr. Zussman referred her to an endocrinologist to strengthen her bones, ensuring she was physically and mentally prepared. When she was ready, Cynthia underwent the procedure.
Cynthia’s surgery was extensive, lasting eight hours and involving a long incision down her back. Dr. Zussman used advanced imaging techniques to guide the placement of 17 levels of screws with precision. He removed damaged discs and relieved pressure from pinched nerves. The screws were then connected by long, strong rods to realign her spine, restoring its shape and function.

Post-operative X-rays show Cynthia standing up straight. The screws, rods and spacers help to brace her skeleton internally and maintain her posture.
Cynthia’s recovery was remarkable. She began walking within two days after surgery—far surpassing expectations. Her quick progress allowed her to be discharged without needing inpatient rehab, and she completed a shorter-than-usual course of outpatient therapy.
“Cynthia now walks completely straight without a cane,” said Dr. Zussman. “Even people at her grocery store notice the drastic difference and give her hugs.”
Cynthia credits Dr. Zussman and his team with giving her life back. “I’m so happy I can move and do stairs—it’s like a miracle,” she shared.
Wellstar’s neurosurgery team addresses complex brain and spine conditions, including adult spinal deformity. In severe cases, scoliosis correction surgery requires a dedicated team of 10 to 15 medical professionals working together to realign the spine.
“This type of surgery can be totally life-changing,” Dr. Zussman shared.
Only a few neurosurgeons in Georgia perform this extensive surgery. Wellstar offers this advanced level of scoliosis care at Wellstar Cobb Medical Center, Wellstar Kennestone Regional Medical Center, Wellstar MCG Health Medical Center and Wellstar North Fulton Medical Center. Reach out to a location near you to schedule an appointment:
Learn more about spine surgery at Wellstar.

Make Breast Health Your Habit
When it comes to diagnosing breast cancer, time is of the essence.
That’s why Wellstar uses state-of-the-art imaging technology to help identify cancer sooner, so we can treat it faster. Getting a screening mammogram can save your life, so don’t delay.
“The earlier we detect a breast cancer, the better we are able to treat it,” said Wellstar Chief of Women’s Health Dr. Paula Greaves.
With several imaging centers offering mammography, it's easy to find one that's convenient to you.
If you do not have any risk factors that increase your chance of developing breast cancer, you should start annual screening mammograms at age 40.
If you’re at higher risk for breast cancer, your provider may recommend you start screenings earlier and can help you create a personalized plan.
“Being female at birth gives you a 1 in 8 chance of developing breast cancer, but there are other components that can increase that risk,” Dr. Greaves said.
You may be at higher risk of developing breast cancer if:
Call (678) 581-5900 to schedule your mammogram. You can also ask your Wellstar care team to put your mammogram order in MyChart and you'll be able to schedule the test online. Find a mammography location near you.
A mammogram uses low dose X-rays to examine the breast for abnormalities and signs of cancer. Wellstar offers 3D mammograms, which provide a series of detailed images of the breast, allowing healthcare teams to better evaluate breast tissue layer by layer. In these images, fine details are more visible as compared to 2D mammograms and are no longer hidden by overlapping tissue.
The mammography unit is a rectangular box that houses the X-ray tubes and special accessories so that only the breasts are exposed to radiation. Attached to the unit is a device that holds and compresses the breast and positions it so images can be taken from several angles.
The technologist is with you throughout the procedure and will ensure that the necessary images have been taken before completing the exam.
Once you have completed a mammogram, you may resume your normal, everyday activities.
If your screening mammogram results are normal, your next mammogram will be the following year, unless your care team recommends more frequent screenings due to family history or other risk factors. If you notice any changes such as a lump, sore spot or a difference in the appearance of the skin, contact your clinician.
When a mammogram result is flagged for follow-up care, it can be scary and intimidating for patients and their loved ones—but at Wellstar, you won’t have to navigate your health journey alone.
As you search for answers about your breast health, the Wellstar Comprehensive Breast Health Program and its complimentary concierge services will make your experience more seamless with a tailored care plan, advocacy for your physical and emotional well-being, dedicated team members for scheduling appointments and education about your care options. Our team of experts will stay by your side through the entire diagnostic process, offering personalized counsel at every step.
For more information on our Comprehensive Breast Health Program, call (470) 610-1910 or email [email protected]. Learn more about our personalized breast care at wellstar.org/breasthealth.
In addition to yearly mammograms, your doctor may recommend you conduct monthly breast self-exams to look for any changes. Signs of breast cancer can include:
If you notice any of these symptoms, reach out to your doctor and schedule an appointment to evaluate your breast health.
Your Wellstar care team will support you at every step of your breast health journey, from screening mammograms to follow-up care.

LGBTQ Care: Inclusive Healthcare for Everyone
With dedicated health resources and caring, compassionate providers, Wellstar is making primary care more accessible to people who are lesbian, gay, bisexual, transgender and queer/questioning (LGBTQ+).
Historically, many healthcare systems have not focused on the specific needs of the LGBTQ community.
“The LGBTQ community has been marginalized by the healthcare system,” Wellstar Primary Care Physician Dr. Gabriella Maris said. “There is a lack of providers who have adequate training to understand and treat their unique health risks.”
Wellstar believes every person should have access to safe, high-quality healthcare. At each of our primary care locations, we maintain a welcoming, non-judgmental environment to treat patients. Across Wellstar, we’re committed to providing inclusive medical services in a safe, comfortable space to make LGBTQ care more available.
Members of the LGBTQ community may be at a higher risk for certain medical issues.
For example, lesbian and bisexual women may be at increased risk for breast, cervical and ovarian cancer, according to the American Cancer Society. The American Psychiatric Association also shared that LGBTQ people are more likely to experience mental health concerns and use mental health services.
Treating these health concerns starts with trained providers who take a caring, compassionate approach to help patients stay healthy.
Wellstar provides primary care for the LGBTQ community, including wellness exams, chronic disease management, virtual appointments and other health screenings. We also offer special services for people who identify as LGBTQ including:
Gender-affirming care is medical treatment that supports a patient’s gender identity when their identity differs from their sex assigned at birth.
“Gender-affirming care has the ability to save lives,” said Wellstar Primary Care Physician Dr. Danielle Ortega. “We know that a large percentage of transgender individuals, even starting in adolescence, have either suicidal intent or attempts in the past, and we know that gender-affirming care, when appropriate, improves mental health and prevents suicide.”
Wellstar physicians provide great care to patients and our health experts are dedicated to being a true partner in your wellness journey.
“I want for patients to know that Wellstar is their medical home—for them to feel comfortable when they walk in our door and for them to know that this is going to be a clinic that is not judgmental, is truly empathic and is here to help them in whatever way we can,” Dr. Maris said.
Our primary care team puts patients at the center of their care, presenting them with all their options and working with them to decide how to accomplish their goals.
“I get to know patients and understand what their goals are, what their hopes are, who their supports are, what their job entails, what their community is like and, specifically, what their goals are in relation to their health,” Dr. Ortega said.
Find a Wellstar primary care location near you. Learn more about diversity, equity, inclusion and belonging at Wellstar.

Surgery Center of Columbia County and AU Health Imaging Transitioning to Wellstar Facilities
Effective November 2, 2024, Surgery Center of Columbia County and AU Health Imaging will be transitioning to Wellstar Outpatient Surgery Center Columbia County and Wellstar MCG Health Imaging Wheeler Road, respectively.
This change is part of Wellstar’s ongoing commitment to enhance the quality of care we provide and to ensure that our patients receive the most comprehensive and integrated care. As a result, patients will have greater access to a broader range of medical services, specialists, and advanced technologies within our hospital network.
While transitioning to a hospital-based entity will result in changes to the billing and payment process, it is our goal to make this transition as simple and convenient for patients as possible. Moving forward, patients will receive billing statements from two entities: Wellstar MCG (Hospital) for services rendered during treatment, and Wellstar Medical Group (WMG) for physician services. Our surgery and imaging services will stay at their current locations and our team members remain committed to providing world-class patient care and services to our community.
We encourage patients to contact their insurance carrier and/or Wellstar Customer Service at 956-STAR (770-956-7827) with any questions.
Thank you for entrusting Wellstar with your care. It is our privilege to serve you.

ChrisCare
It’s not every day that a young man survives a nearly fatal car accident and takes a victory walk through the hospital hallways to thank his care team. After suffering a rare cricotracheal separation that left Chris LoCurto unable to effectively breathe on his own, that’s exactly what happened.

At 22, Chris was in a car accident that caused serious injuries he wasn’t sure he’d be able to survive. He fractured his jaw, clavicle and spine and his lung collapsed. His most life-threatening injury was a tracheal separation—his airway was cut in half.
EMS professionals arrived on the scene. Although Chris was talking and walking, they could hear something abnormal in his breathing. The paramedics coordinated care with Wellstar Kennestone Regional Medical Center so the trauma team would be assembled and ready for Chris upon arrival.
“I was trying to breathe but I wasn’t getting air,” Chris said. “Going to the hospital, I was honestly thinking I wasn’t going to make it.”
Led by Dr. Daniella Kington, the trauma team was waiting when Chris arrived. Immediately, they intubated him so he could breathe. They used a bronchoscope, a special camera, to see inside the airway to diagnose the injury and learn important details to plan treatment.
Chris was then put on extracorporeal membrane oxygenation (ECMO). This highly-advanced machine helps the heart, lungs or both heal after extreme trauma or organ failure.
“For Chris, ECMO supported his breathing and oxygenation during the intricate surgical repair of his trachea,” said Jamie Van Ness, MBA, BSN, TCRN, director of Trauma Services at Wellstar Kennestone.
Now a Level I Trauma Center, the hospital is one of a few in Georgia that offers ECMO.
Dr. Nelson May, a head and neck trauma surgeon, was assisted by Dr. Nicholas Mildenhall to perform Chris’ tracheal repair. The surgery required the surgeons to reattach Chris’ larynx to his trachea. Then they placed a tracheostomy tube so Chris would be able to breathe, swallow and talk again.

To allow his airway to heal, Chris was sedated for a few weeks. When he woke, his injuries had been treated but he was fighting pneumonia. He was transferred to intensive care and his condition improved within a week.
Throughout his time in the hospital, Chris received the right treatment at the right time thanks to Wellstar’s multidisciplinary approach to care.
“Coming to Wellstar Kennestone made a difference in Chris' outcome,” said trauma surgeon Dr. Ginger Justice, a physician who got to know Chris on her daily rounds. “He came to a trauma center that had all the resources to care for him—pretty much from the moment he hit the Emergency Department to discharge.”&
When Chris was a patient, all the specially trained doctors and advanced technology were available to help him recover from his life-threatening injuries. Shortly after, Wellstar Kennestone was verified by the American College of Surgeons as a Level I Trauma Center, the highest level of trauma care offered.
“The first and most crucial piece [to Level I Trauma Center verification] is that we have all the different subspecialists available in one place to provide full care for our patients,” Dr. Kington said. “If a patient comes in, no matter where they’re injured, we have a subspecialist who can help with all those different injuries.”
That was exactly what Chris needed. In addition to helping people get trauma care fast, Wellstar Kennestone is home to a residency program, training the next generation of trauma doctors.
For about a month and a half, Chris recovered in the trauma unit, ICU and intensive inpatient rehabilitation. In Wellstar Kennestone’s inpatient rehab, specially trained speech, occupational and physical therapists create a specialized care plan to help each patient achieve their goals and get back to living life.
While the trauma team saved his life, Chris credits his nurses with keeping him motivated.
“Every nurse I met who came in, we ended up forming some sort of relationship,” Chris said. “They took care of me like their own. That’s not in their job title, nobody asked them to do that, which is why I’m so grateful. They went above and beyond what they get paid to do to make me better physically and mentally.”
For example, one nurse found out about Chris’ love of aviation and brought him to see an air ambulance helicopter. Another nurse shared his love for hunting and planned a reunion for Chris and his hunting companion, his dog Maddux.

“While the future was kind of unforeseen, the nurses connected with me,” Chris said. “I got to spend some time with my dog too. It was huge for my mental well-being.”
Chris defied the odds by walking, talking and being able to eat. Today, he’s taking steps toward a full recovery. While learning to live with a tracheostomy tube, he’s working out and increasing his cardio exercise. He spends a lot of time walking Maddux.
“I’m slowly introducing myself to normalcy again,” he said.
A crucial part of recovery was visiting the hospital and saying “thank you” to his care team.

“He and his family walked in,” Dr. Justice remembered. “I saw Chris in normal street clothes, walking with his sunglasses on. He said, ‘Hey, I’m doing great!’ To see this young man with so much potential have a good outcome was very inspiring.”
Chris made sure to thank as many care team members as possible. “Their motivation and drive to get me going is without a doubt one of the reasons I’m moving around as good as I am today,” he said.
Dr. May added, “It was gratifying to see the real-life implication of Chris’ care and to be able to participate in getting him to where he is today.”
Overall, without the first-rate trauma response of Chris’ medical team at Wellstar Kennestone, he would not be where he is today—back in the wilderness with Maddux.
“The coordination of many different teams and doctors with different areas of expertise in different phases of his care allowed him to be where he is today,” Dr. May said.
Wellstar Kennestone provided the advanced care Chris needed with excellent trauma services. Now with a Level I Trauma accreditation, the trauma team can keep offering advanced care—and preparing the physicians of the future to do the same.

Wellstar Uses Innovation and Technology to Improve Healthcare: Highlights from Health Connect South Conference
At the recent Health Connect South conference, Dr. Charles Craton, Quality Medical Director of Primary Care at Wellstar Health System, participated in an impactful panel discussion titled “Driving Innovation in Your Backyard: Helping Local Startups Get Off the Ground.” The discussion brought together Dr. Craton and other medical experts to explore how innovation and technology are shaping healthcare access and outcomes across the state.
“Part of my role as the Quality Medical Director is to provide great evidence-based care, but I also want to make it easier on our primary care doctors and help reduce burnout,” Dr. Craton explained.
He highlighted Catalyst by Wellstar's pilot program, developed in collaboration with MapHabit, a company dedicated to helping individuals with cognitive disorders. The technology allows patients living with Alzheimer’s disease, intellectual and developmental disabilities, autism, and traumatic brain injuries to live more independently. After learning about MapHabit, Dr. Craton reached out for more information.
“We don’t have great tools for these conditions,” he said. “While we have medication to slow disease progression, this is a tool that can help a lot of people live a better life.” Matt Golden, CEO of MapHabit, was also a panelist. He discussed the growing prevalence of Alzheimer’s, asking audience members to raise their hands if they knew someone affected by the disease. Nearly 80 percent of attendants raised a hand.
“Ten years ago, you might have only had half that response, but unfortunately, Alzheimer’s disease is exploding as people live longer,” Golden shared.
The collaboration between Wellstar and MapHabit is a testament to Wellstar’s ongoing commitment to innovative care. The pilot program, currently taking place in Douglasville and through Population Health Managers, involves ten primary care physicians and 75 families from these practices. The study includes a diverse population, with 65% of study patients being African American, ensuring that the findings and benefits of the program are relevant and beneficial to a wide range of communities.
MapHabit is the first company to use the spared memory system through visual cues and applied behavioral analysis—proven habit-building techniques that benefit people with cognitive decline. The system allows caregivers to set up step-by-step guides for specific tasks they want their loved ones to learn. Patients can follow these visual steps and, over time, perform daily activities without thinking through each step, using a preserved area of the brain. This unique approach helps drive independence for neurodiverse individuals.
Dr. Craton shared that they are halfway through enrolling participants in the pilot, which serves as a proof of concept, and early results have shown improved outcomes. His vision is to see the tool implemented across the entire Wellstar system.
“My ultimate goal is to conduct a full study and publish comprehensive data,” Craton said.
Wellstar Leads the Way in Using Technology to Improve Patient Experience
Wellstar’s commitment to safely streamlining the flow of information was among the highlights at a gathering that brought together more than 1,200 health leaders from across the South.
Bob Speakman, Wellstar’s VP and Chief Technology Officer, participated in a panel discussion titled, “The Rise of the Digitally Native Health Care Consumer” at Health Connect South’s annual event Wednesday at the Georgia Aquarium. Speakman gave insights into Wellstar’s partnership with CLEAR, the technology company that provides biometric travel document verification systems at airports and stadiums across the U.S.
In May, Wellstar became the first healthcare system to pilot a program that allows patients to efficiently check in for appointments using CLEAR’s technology integrated into Epic’s kiosks and tablets. The technology uses facial recognition to verify a patient’s identity and streamline the check-in process safely and reliably. Wellstar pioneered the development of this solution in partnership with CLEAR and Epic.
“Everything we’re doing is based around the patient experience,” Speakman said. “We’re trying to make things better, easier, less stressful. Our objective is to replace the clipboard.”
As patients of all ages become more comfortable with having technology at their fingertips, Wellstar continues to lead the way in exploring the application of smart-phone and other technology innovations in the healthcare setting.
During the gathering, Speakman also said he’s excited about healthcare innovations surrounding artificial intelligence.
“I’m excited about the AI stuff. It’s going to be a game changer,” he said.
Other participants in the Health Connect South panel discussion were David Bardan, General Manager and Head of Healthcare for CLEAR, and Dr. Priyanka Agarwal, Founder and CEO of HealthEx. Ryan Howels, Principal of Leavitt Partners, served as the moderator.

Improving Health Through Collaboration: Health Connect South 2024
Each year, leaders and innovators from across the Southeast come together at Health Connect South to discuss the health needs of our communities and how local systems and organizations can collaborate to address these needs. This year's event, held on September 18 at the Georgia Aquarium, convened healthcare, finance and community leaders to discuss shared solutions for challenges like healthcare accessibility, workforce shortages and health outcomes.
During a panel discussion with other healthcare leaders, Wellstar Health System President and CEO Candice L. Saunders explained how healthcare collaborations can improve access to care and workforce development, and the importance of leveraging technology and innovation to improve the lives of our communities.
"As we look at the future of healthcare, where we're going, what's happening in the healthcare industry from an overall cultural transformation and all the other opportunities and challenges that we face, we see a different future for healthcare— one that is much more holistic, more proactive," said Saunders.
Wellstar knows the importance of collaboration and has long worked with community partners and local systems to enhance the health and well-being of every person it serves across the region.
Last August, Wellstar announced a partnership with the University System of Georgia and the Medical College of Georgia (MCG) in Augusta to create Wellstar MCG Health. The organizations' shared vision for effectively addressing the unique needs of people and communities across Georgia has inspired several programs and initiatives to expand access to care and develop the healthcare workforce of the future.
"As we focus on our biggest problems and opportunities, we must use technology, including AI, to augment care and help our caregivers. But we also want to make sure we can make it more human. We can't forget the important human connection in health care, which we all need to protect," she continued.
Saunders also shared how leveraging innovative technology to advance telehealth has presented significant opportunities for Wellstar and Wellstar MCG Health to reach patients and clinicians in every corner of the state. Through the Rural Hospital Virtual Care Network, pioneered by Augusta University Health, rural hospitals can receive support from local systems like Wellstar for particularly challenging procedures. The network also helps address significant health disparities across rural Georgia, such as maternal and cardiovascular health.
The panelists also discussed the issue of recruiting and retaining clinicians to address the shortages health systems and hospitals have faced in recent years. According to the federal Health Resources Service Administration, Georgia currently has 21% fewer registered nurses than the state needs. The state is expected to see the second-highest shortage in the country by 2035. That's why, as Saunders shared, the Wellstar College of Nursing at Kennesaw State University, in partnership with Wellstar, is working to double the number of students in the next four years, ensuring a strong pipeline of new nurses to address the shortages we continue to see.
"You must have partners; the health systems cannot do this alone. And how do we help people continue to learn and grow? We know that it is not only really good for patient care but also good for business," Saunders continued.
Through Wellstar's partnership with MCG and other state medical colleges and universities, work is underway to expand residency programs to educate hundreds of future clinicians statewide. Students at MCG will also be trained to use Epic, ensuring they are prepared to use the latest digital tools as technology continues to evolve and drive innovation in care delivery.
Wellstar team members also have significant opportunities for professional development and advancement, such as the CareerCare program, which provides funding for tuition in select healthcare career pathways and expands professional development, education and growth opportunities.
Wellstar is proud to partner with organizations across the state to meet Georgians' healthcare needs now and for years to come. Together, these organizations can create the healthcare workforce of the future, leverage technology to increase affordability and accessibility of care, and improve the health of the patients and communities they serve.

Make Prostate Health Your Habit
Quick history lesson: In the 1990s, U.S. doctors adopted the prostate-specific antigen test—or PSA—to identify prostate cancer early, when it’s more treatable. While the PSA helped more men get diagnosed, concern was raised over the risks versus benefits of biopsies, procedures and treatment. In response, the U.S. Preventive Services Task Force gave a controversial recommendation against routine screening with PSA in 2012.
But with new evidence from a variety of credible studies, they changed their recommendation in 2017. The current Task Force recommendation focuses on men having a conversation with their doctors about their risk for prostate cancer and the risks and benefits of screening.
Prostate cancer is the most common cancer diagnosed in males after skin cancer. The American Cancer Society projects that there will be more than twice as many prostate cancer cases diagnosed in men as lung cancer this year.
“The prevalence of the disease cannot be ignored,” said Dr. Jeffrey Tharp, a primary care physician and chief medicine division officer for Wellstar Medical Group. “Early-stage prostate cancer has higher survivability than prostate cancer diagnosed in later stages.”
Dr. Tharp pointed out that while guidelines have changed, so have the way doctors diagnose and treat prostate cancer. An elevated PSA does not automatically mean a cancer diagnosis. And when cancer is diagnosed, some care options have no side effects.
Read on to learn:

Wellstar Children’s Hospital of Georgia Renovating to Better Serve the Region
Due to renovations at Wellstar Children’s, the main lobby and parking circle are closed. The renovations are ongoing until Spring 2025. Here’s how to plan your visit while construction is underway.
Wellstar Children’s continues to expand to meet the growing needs of the CSRA. To help improve your access to care, the Wellstar Children’s lobby is closed for renovations beginning August 29, 2024. During renovations the main entrance on Harper Street and the first floor elevators will not be accessible. The Wellstar Children’s parking circle will also be closed to all traffic.
Patient Access
For ease of access, please park in Medical Center Parking Deck 2 at 1461 Harper St.
Pharmacy Curbside Pick-up
Reserved parking for pharmacy pick-up will remain available.
Chick-fil-A Access
Chick-fil-A will remain open and accessible during renovations.
Blue Coat Ambassadors are always available to assist. Find a team member wearing a blue blazer to answer any questions you have.

Wellstar Cherokee Health Park Expands Cancer Care
The cancer care experts at Northwest Georgia Oncology Centers at Wellstar Cherokee Health Park are dedicated to patient-centered care that’s tailored to every patient, every time. We have expanded our services and space to invest in the health of our community in Cherokee and the surrounding areas.
Our facility now has tripled patient exam rooms and quadrupled infusion recliners to facilitate complex treatment that is requested by our cancer patients. We’ve also added support services, including an onsite compounding pharmacy and a clinical pharmacist available to help answer any questions.
Our leaders, researchers and innovators collaborate with specialists and care team members to create treatment plans for optimal clinical outcomes.
Our services include:
“At Wellstar, our patients have the support they need at every step of their cancer care journey,” said Wellstar Hematologist and Oncologist Dr. Madhurima Uppalapati. “Our team provides expert care for every aspect of the patient’s well-being and personalizes care to each patient’s needs.”
Support services include nurse navigators, who are registered nurses specially trained in cancer care who bring a highly personalized level of guidance and support to each patient and their family. Other members of our cancer care team include dietitians, social workers and genetic counselors.
To schedule a cancer care appointment at Wellstar Cherokee Health Park, call (470) 267-0230.

Wellstar MCG Health, Doctors Hospital, Piedmont Augusta, and VA Unite in New Healthcare Leadership Council
Leading healthcare institutions in the Central Savannah River Area (CSRA) have joined forces to enhance collaboration and address critical healthcare needs in the region. The inaugural meeting of the CSRA Healthcare Leadership Council convened Dec. 12, 2023.
Comprising the top executives from the area’s foremost hospitals, the council includes Ralph Turner, president of Wellstar MCG Health Medical Center; Joanna Conley, chief executive officer of Doctors Hospital; Lily Henson, chief executive officer of Piedmont Augusta; and Robin Jackson, medical center director of the VA Augusta Health Care System.
Wellstar MCG Health’s Ralph Turner emphasized the significance of collaboration among healthcare leaders. “Sometimes there’s a focus on competition among hospitals, but we have a common goal of wanting to take care of the people in our community.”
Joanna Conley added: “At Doctors Hospital, our mission is that, above all else, we are committed to the care and improvement of human life. By convening regularly, we can strengthen our partnership and elevate the level of care across the CSRA.”
Robin Jackson of VA Augusta Health Care System said the council is about sharing resources, knowledge and best practices. “Quality healthcare doesn’t happen in isolation. It starts with partnership. The communication and collaboration coming out of the CSRA Healthcare Leadership Council will only strengthen the quality of care we deliver to local veterans and the wider community.”
The group’s monthly meetings will focus on recurring topics such as community health and emergency preparedness for the area.
“Piedmont Augsuta is creating real change across Georgia, in part through partnerships that empower our communities with education and access to seamless, hassle-free, high-quality care,” said Lily Henson. “By embracing the future and exemplifying teamwork and connections, we can make a positive difference in every life we touch.”
The council’s monthly meetings will rotate among participating facilities, fostering inclusivity and equitable engagement. These gatherings will serve as forums for discussing pressing healthcare issues and identifying collaborative opportunities to enhance patient care and community well-being.

Hyundai Hope on Wheels Awards $400,000 Grant for Pediatric Cancer Research at Wellstar Georgia Cancer Center & Children's Hospital
AUGUSTA, Ga. (Aug. 8, 2024) – With courage that belies her 15 years, Harper Mathis stepped to the podium at Wellstar Children’s Hospital of Georgia and spoke to visitors from Hyundai, Wellstar Health System, Wellstar Children’s, Wellstar Georgia Cancer Center and Augusta University. When she finished, there wasn’t a dry eye in the house.
“This is my second chance at life,” she told them. “Without this trial, I don’t know if I would be here today. I just got the best MRI I’ve gotten in a while.”
On Thursday, Harper and other patients at Wellstar Children’s made their mark for kids battling cancer across the country by pressing their paint-covered hands onto white stickers, which were then placed on a new white Hyundai Santa Fe. The effect is a custom handprinted paint job to commemorate Hyundai Hope on Wheels’ $400,000 grant for pediatric cancer research.
Each year, Hyundai Hope on Wheels visits children’s hospitals across the U.S. to donate a two-year Scholar Hope grant to researchers working to improve outcomes and treatments for children diagnosed with cancer. The annual event also raises awareness for pediatric cancer research.
The $400,000 Scholar Hope grant will fund Dr. Ted Johnson’s research project titled, “Novel measurement of molecular immune activation to predict response to pediatric immunotherapy.” Dr. Johnson is a pediatric hematologist-oncologist at Wellstar Children’s and co-director of the Pediatric Immunotherapy Program at Wellstar Children’s and Wellstar Georgia Cancer Center.
Dr. Johnson and his research team are working to define the mechanisms that suppress the body’s immune response and allow tumor survival, so they can identify ways to counteract those processes and fortify the immune system to fight the tumor instead.
“This grant represents another critical pledge in our fight against pediatric brain tumors,” Dr. Johnson said. “This investigation is important because the more we understand about how these tumors quietly advance, the closer we will get to developing better treatments and therapies. This could positively impact care for children with brain tumors by improving their quality of life.”
This is the fourth Hyundai grant awarded to Dr. Johnson, who has received a total of $925,000 in Hope on Wheels funding since 2011 for his pediatric immunotherapy studies. The current Scholar Hope grant will fund research to measure the immune system’s activation and response to pediatric immunotherapy.
Harper and her family, who are from Michigan, have spent nearly six months at Wellstar Children’s to participate in the study.
“It means the world to me that Dr. Johnson has made his life all about this trial because I needed it so badly and so do other kids,” Harper said. “So many people don’t understand how meaningful this all is and how grateful and thankful we are."
Hyundai Hope on Wheels is a nonprofit organization committed to finding a cure for childhood cancer. The organization provides grants to eligible institutions nationwide that are pursuing critical research aimed at improving treatments and saving lives.

Wellstar Commits $25M to Expand Partnership with Kennesaw State
KENNESAW, Ga. (Aug. 13, 2024) — Kennesaw State University (KSU) and Wellstar Health System (Wellstar) today announced a new collaboration to support the health, wellbeing, and performance of KSU student-athletes. The partnership has three main components:
Today’s agreement builds on a longstanding partnership between the two institutions. Wellstar manages the University’s on-campus student health clinics and is the named donor of KSU’s Wellstar College of Health and Human Services and its Wellstar School of Nursing. In 2020, Wellstar made a $9 million funding commitment to help KSU double enrollment in its Bachelor of Science in Nursing program, which is helping meet Georgia’s urgent need for nurses.
“We are grateful to Wellstar for their continued generosity and support of Kennesaw State’s mission,” said KSU president Kathy S. Schwaig. “Their latest contribution comes at an exciting and pivotal time for the University, and it will further strengthen our ability to train the next generation of healthcare providers, as well as to support athletic programs that will benefit our students for years to come.”
“We congratulate Kennesaw State for growing its healthcare programs and expanding its medical research,” said Candice L. Saunders, president and CEO of Wellstar Health System. “We appreciate the opportunity to take an active role caring for our community’s athletes and providing the next generation of athletes with opportunities to improve their physical and mental wellness, on and off the field.”
Subject to approval by the Board of Regents of the University System of Georgia, the Sports Performance Complex and the Sports Medicine and Training Center will provide comprehensive services to more than 450 student-athletes, including injury prevention and treatment, physical therapy, and hydrotherapy, and will contain a strength and conditioning suite, training table, locker rooms, and new weight room. In addition, the complex will provide a new home for KSU’s football program with team and position meeting rooms, coaches’ offices, and a team locker room.
Wellstar’s funding will also support the creation of the Center for Research on Human Sport Performance and Wellbeing in the Wellstar College of Health and Human Services. The center will engage in research and teaching that explores technological methods to improve sport performance and athletes’ overall well-being.
Officials from KSU and Wellstar celebrated the agreement at a signing ceremony held on the Kennesaw campus, which comes 10 months after the University launched its most comprehensive fundraising campaign, The Campaign for Kennesaw State.
KSU competes in NCAA Division I in eight men’s sports and 10 women’s sports. Since joining Division I in 2005, KSU has won 61 conference championships across a range of women’s and men’s sports.
Earlier this month, KSU assistant coach Daniel Haugh competed in the Summer Olympics in Paris in the hammer throw, becoming the first former student-athlete in Kennesaw State’s Division I history to compete in the Olympics twice. Current student Emma Hunt competed in the Paris Olympics in sport climbing. Other recent success has included the KSU men’s basketball team making a memorable March Madness run to the NCAA Tournament in 2023, and track and field standout Isaiah Rogers winning the national championship in the weight throw.

Wellstar Pediatric Orthopedics Provides Advanced Scoliosis Care for Children
Scoliosis, or curving of the spine, has been around for centuries. Over time, treatments have improved to offer patients more options to maintain motion and recover smoothly. The compassionate experts at Wellstar Pediatric Orthopedics use cutting-edge technology to provide scoliosis care tailored to your child.
Fusion, which involves bone grafting and limiting motion through segments to control spinal deformity, used to be a popular treatment method. However, these treatments could lead to stiffness and postoperative pain concerns.
“As care has evolved, clinicians have begun to focus on alternative methods that help patients maintain motion and flexibility,” said Wellstar Pediatric Orthopedic Surgeon Dr. Timothy Oswald.
Over the last two decades, an immense amount of research and innovation has led to the development of new procedures to preserve motion, called fusionless scoliosis treatments. Currently the two most popular and well-studied treatments are anterior vertebral tethering and posterior distraction technologies.
Vertebral body tethering is an improvement upon previous treatment and allows for the potential of improved correction. However, the procedure has also now been associated with a high incidence of tether breakage and progression.
In this procedure, the surgeon attaches metal anchors to the side of the spine that is curved. A flexible cord is connected to these anchors, and as the child grows, the tether slows the growth on the curved side, helping the spine grow straighter.
Currently there are very limited indications and a very specific time frame when tethers have been found to be successful for improving curves in the growing child. But as with any new technology, the next generation of innovation is encouraging: The tethers have become stronger and indications clearer. Wellstar currently offers this treatment but with very strict inclusion criteria so that we can have the best outcomes for our patients.
Another new option is posterior distraction based fusionless technologies. The surgeon implants a rod with flexible joints that help the patient maintain normal spine motion.This procedure has shown an 85% success rate within two years with controlling the curve of the spine, but there are still concerns of instrumentation failure and progression. Wellstar also offers this surgery and has had good success in the appropriate patient population.
If your child has advanced scoliosis, Wellstar offers multiple care options, and our team is experienced in treating this condition in children. Our specialty surgeons each have over 20 years of experience treating pediatric spinal deformities. To find a surgeon near you, visit wellstar.org/pedsortho.

Get Connected: VIP Portal is Moving to Wellstar MyChart
Wellstar, affiliated with Medical College of Georgia, is transitioning from the VIP Portal to Wellstar MyChart in November 2024. With MyChart you’ll be able to request prescription refills, manage your appointments, access your test results and message your care team.
We’ll help you throughout the transition process, but there are few ways you can prepare and stay proactive with your care. In this article, we’ll provide key dates to keep top-of-mind, instructions on how to create a Wellstar MyChart account, new features to explore in MyChart and answers to your questions. Check back often, as this page will be updated regularly with the latest information. Here’s what you need to know.
October 29, 2024, is the last day you can message your care team and request prescription refills in the VIP Portal. All VIP Portal functions will move to Wellstar MyChart November 2, 2024.
It is important to note that your health records in VIP Portal, such as after-visit summaries and lab tests results, will not transfer to MyChart. Instructions are provided in this article on how to download a copy of your records from the VIP Portal. You will no longer be able to download your records after April 1, 2025.
Access your new patient portal today! Sign up for a Wellstar MyChart account.
Sign up for your MyChart account today! You can create your MyChart account at any time and patient portal functions will be activated beginning November 2, 2024.
Yes, the transition date for Wellstar MyChart has moved to November 2, 2024. If you have already created your MyChart account, great! Now you’re fully prepared for when Wellstar MyChart is available for use in November. Until then, you can continue to use your existing VIP Portal as you do today.
Visit mychart.wellstar.org. You can also learn more about MyChart at Wellstar at wellstar.org/mychart.
If all your information does not match what is in our system, someone will reach out to you by email within 48 hours or you can call the MyChart Help Desk at (470) 644-0419 for assistance.
Yes, there are several options.
Yes, you can download the app in the Apple App Store or Google Play.
To view MyChart in Spanish, go to the MyChart login page and click Ver en Español in the top right corner. At this time messages from your provider are not translated into Spanish.
There are two changes to be aware of:
To message your providers, you must re-establish your relationship as their patient within MyChart. This is an automated process that occurs after you have had an in-person or virtual visit with your physician or advanced practice provider.
There are three ways to schedule an appointment:
You can request prescription refills through your pharmacy.
Yes, you can request refills through MyChart for medications ordered after November 2, 2024. Here’s how:
Your healthcare records will not transfer from VIP Portal to MyChart. Here’s how to download your records.
Wellstar reminds you to store your personal records and information in a safe, secure place.
You will have access to all your healthcare records prior to November 2, 2024, in the VIP Portal until April 1, 2025. In accordance with HIPAA laws (Code of Federal Regulation 164) and Georgia Statuses, your official medical records are stored within the Wellstar, affiliated with Medical College of Georgia, system. You have the right to access and obtain copies of your protected health information. To request your official medical records at any time, contact our Health Information Management Services Department at (706) 721-2948 or visit wellstar.org/request-medical-records for more information.
VIP Portal records will be available upon request after April 1, 2025. Click here to request your records.
Once you have created your account, you will begin to see your after-visit summaries, lab tests results and more in MyChart for Wellstar provider visits November 2, 2024, and later. These will include hospital and medical office visits.
You will be able to see your lab test results, mammogram results and chronic disease information in your MyChart account.
HIV and genetic testing will not be in Wellstar MyChart. You can request those records here.
Yes, you will gain new functionality in MyChart. Some of the many features include:
o You can request adult proxy access for a family member or caregiver via your MyChart by searching the Sharing Hub, selecting Manage Friend and Family
Access and following the prompts.
o If you have power of attorney rights for an adult patient, you must provide a copy of your legal documents along with a completed Adult Proxy Form to gain
MyChart proxy access. (Adulto Delegado Formulario en Español)
o For children 17 years old or younger, parents/legal guardians can be granted full access to their child’s MyChart account by completing a Child Proxy Form.
(Formulario Para Representante de Menor en Español)
o When a patient turns 18 the parent/legal guardian’s proxy access will automatically be revoked because the patient is now a legal adult.
o Teen Access allows teens age 12 to 17 to have full access to their own MyChart account. Teens can invite family or legal guardians to have full proxy access to
their account by using the adult proxy feature mentioned above.
o You can view and pay your bill through Wellstar MyChart beginning November 2, 2024.
o You will now see cost estimates for your medical care via MyChart for dates of service November 2, 2024, and forward.
o You will have the ability to set up a payment plan in MyChart.
If you have questions about your bill, payment plan or want to make a payment, contact (888) 531-0397 or visit the Patient Bill Portal. If you have questions about extended payment plans or Access One, contact (888) 458-6272.
Please call (866) 700-2989.
Contact (844) 703-5532.
Call (706) 721-1301.
Will I still call the VIP Portal Help Desk for my VIP Portal questions after October 29, 2024?
No, you will call the MyChart Help Desk at (470) 644-0419. There will be a patient portal specialist available at this number to assist with any of your patient portal questions.
We’re here to help. You can email us at [email protected], call us at (470) 644-0419 or send a fax to (770) 999-2306. The patient portal help desk hours of operation are Monday through Friday, 8:30 AM to 5 PM.

Wellstar Urgent Care Clinic in Stockbridge to Transition Operations to Southside Medical Center Sept. 3
Effective Sept. 3, Southside Medical Center will assume operations of the Wellstar Urgent Care clinic in Stockbridge. The Wellstar Stockbridge urgent care location will remain open through Thursday, Aug. 29, before transitioning operations to Southside and reopening on Sept. 3.
There will be no loss of services. After Sept. 3, Southside will continue to provide urgent care services and, in the future, expanded primary care services like immunizations and annual wellness visits will also be available. Patients will notice new signs and new staff but will continue to receive the same high-quality care from our partners at Southside that they have come to expect at this location.
We have kept our patients top of mind throughout this process, developing a thorough communications plan to notify them of this change. We will reach out to patients in the community to provide more information about this change through signage, postcards and electronic messages.
As part of this next phase of our partnership, Wellstar is contributing nearly $1 million in operational funds and donating medical equipment to ensure a successful transition of care in Stockbridge. We are committed to working closely with the Southside team to ensure a smooth transition of care.
The clinic will continue to be open seven days a week from 8 a.m. to 7:30 p.m. Urgent care services are available via appointment or walk-in and care will continue to be provided to all patients regardless of their ability to pay.
We appreciate the opportunity to serve as your healthcare partners, and we hope you will continue your care with us after this transition. Thank you for entrusting us with your care.
For more information on Southside Medical Center, visit SouthsideMedical.net.

Cooling Caps Help Reduce Hair Loss from Chemotherapy Treatments
Hair loss can be a difficult side effect to navigate for people with cancer. It affects a person both emotionally and mentally as they deal with a change to their outward appearance while undergoing a serious health battle.
“Hair loss during chemotherapy can cause patients to feel vulnerable and self-conscious,” says Andrea Rhoden, a breast oncology nurse navigator at Wellstar Georgia Cancer Center.
Emotional well-being is an important factor to your physical health, as poor emotional health can lead to higher blood pressure, a weakened immune system and other health issues that can become quite serious for patients with a cancer diagnosis.
Andrea saw a need for a way to prevent hair loss and immediately thought of cooling caps.
Cold scalp cooling caps are caps patients wear before and after chemotherapy that can help prevent hair loss by reducing the damage that chemotherapy causes to hair follicles. They work by cooling the blood vessels in the scalp and reducing blood flow to hair follicles, which restricts the amount of chemotherapy medication that enters hair follicle cells.
While this device cannot reduce hair loss by 100% for all patients, patients can see a hair loss reduction of about 50% when using a cooling cap throughout their treatment journey.
These devices can be costly, so Andrea and her collaborator, Dr. Alicia Arnold, submitted their program, Cooler Heads for Helping Hair Loss During Chemotherapy, for funding from Unite in the Fight Against Cancer 2023.
Unite in the Fight Against Cancer is a 1-mile walk that celebrates and honors all who have been affected by the disease, while raising funds for patient-centered programs.
Andrea and Dr. Arnold’s program received funding from Unite 2023, along with six other programs, covering the costs for two machines and the supplies needed to use them.
“I’m so excited for this opportunity,” Andrea said.
To learn more about this program, follow us on social media to be kept up-to-date on it and other programs funded by Unite in the Fight Against Cancer, which is held annually.

Wellstar Opens New Urgent Care Centers in Augusta
Wellstar has new urgent care centers in Evans, Grovetown and South Augusta to serve our community’s growing healthcare needs. These locations provide convenient care for minor emergencies, illnesses and injuries.
Walk-ins are always welcome, but you also have the option to book a visit online at the time that works best for you. Booking online can help reduce your wait time once you arrive.
Our new Wellstar Urgent Care locations:
307 W Robinson Ave | Grovetown, GA 30813
(706) 760-7607
Open seven days a week, 8 AM to 7 PM
Urgent Care Check-In at this location
3324 Peach Orchard Road, Suite B | Augusta, GA 30906
(706) 760-7607
Open seven days a week, 8 AM to 7 PM
Urgent Care Check-In at this location
4244 Washington Road, Suite 1 | Evans, GA 30809
(706) 760-7607
Open seven days a week, 8 AM to 7 PM
Urgent Care Check-In at this location
Wellstar Urgent Care provides:

New Leaky Heart Valve Treatment Gives Thomson Student a Bright Future
Like most seniors, Ja’Quan Hart was very much looking forward to going off to college in the summer of 2023.
The Thomson, Ga., resident had just graduated high school and as a linebacker and tight end, helped lead his Thomson High School Bulldogs to win the Class AA State Championship.
“I had these big tackles, and I caught like an 89-yeard interception pass,” he said. “That was like my best game. We won state!”
Ja’Quan’s talent and skill on the football field—and his love of the game—earned him the opportunity to play for the University of Kansas with a full scholarship.
Unfortunately, life had other plans.
Amid packing for school and booking his flights, Ja’Quan learned from a routine sports physical that he had an irregularity in his heart that could be life-threatening.
That irregularity turned out to be a leaky aortic valve—and an abrupt end to his aspirations of a college football career.
“Blood was flowing back into my heart. It wasn’t going all the way through,” Ja’Quan explained.
In a healthy heart, leaflets between the left and right ventricles open to allow blood to flow through the heart one way and then close fully to keep blood from flowing back into the heart. In a condition like Ja’Quan’s, the leaflets do not close all the way and blood does leak back into the heart.
For most people the treatment for a leaky aortic valve involves a valve replacement. But a valve replacement now will often require another replacement surgery at some point in the future, and probably more than one, said Dr. Brian Bateson, a pediatric cardiothoracic surgeon and co-director of the adult congenital heart program at Wellstar MCG Health Medical Center. The younger the patient, the more potential surgeries the patient will need to have to replace the valves when they wear out.
Because Ja’Quan had not yet reached 20 years of age at the time of his care, a valve replacement would mean multiple surgeries over the course of his life.
The solution is a new device called the HAART ring that is affixed to the support structure of the aortic valve. This stabilizes the valve and allows for further repair of the leaflets themselves, meaning the valve can close properly and prevent leakage.
“If you’re using Ja’Quan’s own valve, keeping it in place and it functions, potentially he wouldn’t need another procedure again in his life because it’s still his own tissue. It’s not going to break down. Any prosthetic valve, whether it’s mechanical, bio-prosthetic will fail over time,” Dr. Bateson said. “Nothing’s better than what you’re born with.”
The HAART device is ideal for a young patient like Ja’Quan, but would also be a good treatment option for any person—pediatric or adult—with the same condition.
Ja’Quan spent three days in the hospital recovering from his surgery. Since, he has been slowly increasing his cardiovascular activity, such as walking, and following up with Dr. Bateson for regular checkups, who said he has been recovering very well.
Ja’Quan said he plans to continue to play sports, but will need to be more selective about the sports he can play.
“I play basketball. I just won’t be playing contact sports (like football),” he said.
Though he said it was disappointing to have to change direction as far as playing college football is concerned, Ja’Quan hasn’t let it dampen his spirit. Instead of college football, he is now exploring the possibility of driving trucks with the intention of going into business for himself—as long as it isn’t too strenuous for his heart.
“I’m not going to give up. I’m going to regroup and keep going and find another path to being successful in life,” he said.

Connect with Community Resources Using Wellstar Find Help
At Wellstar, we’re committed to enhancing the health and wellness of everyone we serve, both in our facilities and in our communities. That means not only helping the individuals who walk through our doors, but meeting our neighbors right where they are. Through a variety of community programs, we can reach many—at our schools, in our places of worship, at community events in our neighborhood and at home.
With the Wellstar Find Help tool, search for free or reduced-cost resources to help you care for every aspect of your well-being, including:
The site, which is available in several languages, is one of several Wellstar initiatives to address social determinants of health, or the non-medical factors that can affect someone’s well-being, such as access to nutritious foods, housing and education.
Learn more about resources at wellstar.findhelp.com.

Wellstar Switches to Paperless Statements
You can save time and help reduce environmental impact by taking advantage of eco-friendly options for managing your Wellstar account online. Effective August 15, 2024, all Wellstar MyChart users will be enrolled in paperless statements.
Paperless statements give you a convenient and secure way to see your account balance through Wellstar MyChart.


Playing it Safe Ahead of the 4th of July Holiday
As we look forward to the 4th of July holiday, fireworks, swimming, and grilling offer plenty of fun summer activities for families across Georgia. However, it's important to be cautious with fireworks, which can quickly turn your Independence Day celebrations sour. While public fireworks displays have safety measures to protect us, fireworks at home may be less safe, especially for kids!
According to the United States Consumer Product Safety Commission, over 10,000 individuals were treated in ERs for fireworks-related injuries in 2022, 38% of which were burns.
With summer camps in full gear and celebrations right around the corner, Wellstar sat down with Dr. Danny Branstetter, the chief medical officer of Wellstar Kennestone Regional Medical Center, and Dr. Joanna Dolgoff, a Wellstar pediatrician and representative for the American Academy of Pediatrics, to learn their safety tips for staying safe while we celebrate this holiday.
According to Dr. Dolgoff, "The most common injury from fireworks is a hand burn. But it can be worse, such as a hand fracture, cuts, or gashes, or even the loss of a finger," Dr. Dolgoff continued. "Facial injuries, including burns and eye injuries, are also common. If you're going to handle fireworks, please be very careful."
We can be so caught up in the excitement of summer that we don't realize there are other seasonal injuries we should be careful to avoid. Dr. Branstetter reminds us that we see more water injuries like drownings and near drownings, water ski and boating accidents, and even head, neck and spine injuries from diving in shallow water.
He went on to share that with extreme heat, we should plan ahead to avoid heat-related exhaustion, stroke, and sunburns. And to be careful to prevent burns from items that can get hot from the summer sun, like playgrounds and seat belts.
And let's not forget those pesky summer critters, "insect and plant illnesses – from mosquito bites and allergic reactions to poison ivy, bee stings and snake bites."
As a pediatrician, Dr. Dolgoff often works with new parents who wonder if sparklers are safe. She stresses that parents should "not underestimate the danger of sparklers. Sparklers burn at about 2,000 degrees Fahrenheit, which is hot enough to melt some metals. They account for a high percentage of injuries, emergency room visits, and fires every year. The sparks can cause burns and eye injuries." And she added, remember to soak all sparklers in a bucket of water before throwing them away!
If your family plans to participate in holiday activities, remember the word FIRE with these essential safety tips!

Orthopedic Advice for the Weekend Warrior
By Dr. D. Hodari Brooks, Wellstar orthopedic surgeon
By Dr. D. Hodari Brooks, Wellstar orthopedic surgeon
As a board-certified orthopedic surgeon, I treat hundreds of patients a year who have injured themselves while exercising on the weekend. Typically, this involves activities such as pickleball, tennis, soccer, golf and running. While these activities can promote improved muscle strength, joint health and cardiovascular benefits, when they are not done correctly, orthopedic injuries can result. Some of the more common injuries include:
Achilles injuries are some of the most common injuries I treat. Often, they result from improper stretching and warm-up prior to physical activity. When the Achilles is torn, surgical repair is often, but not always, necessary. Ankle sprains are also very common and usually much less severe than Achilles tears. These injuries typically result from rolling your ankle awkwardly when jumping or running. Rest, ice, elevation and compression with a bandage or brace is an effective treatment.
To help prevent these injuries, focus on a good stretching routine for at least 10 to 15 minutes before engaging in physical activity. Proper shoes can also help, and be mindful of where you step.
Meniscal tears are one of the more common knee injuries. The meniscus is a circular disc-like cartilage located in the knee. When a twisting or torsional injury occurs, the meniscus can get torn. This can produce catching or locking type symptoms and may require surgical treatment. Injuries to the patellar tendon or quadriceps tendon are also somewhat common and usually result from a failure to stretch and warm up appropriately. Whenever the patellar or quadriceps tendon is torn, surgery is almost always required.
Focus again on stretching prior to activity. When the activity is relatively strenuous, such as pickleball, tennis or basketball, then you should build up a quadriceps strengthening program and core strengthening prior to engaging in activity.
Rotator cuff injuries are very common and can range from strains to complete tears. Injuries occur when people fall on an outstretched hand, like diving for a ball, or through other twisting motions. When the rotator cuff is strained but not torn, physical therapy will usually suffice. However, when torn, surgical treatment may be necessary.
The best way to prevent shoulder injuries is to focus on stretching prior to activity and to engage in a strengthening program.
I encourage you to engage in physical activity, but attention to stretching, strengthening and focusing on your environment can help you avoid a variety of orthopedic injuries.
Learn more about orthopedic care at Wellstar at wellstar.org/ortho.

Dr. D. Hodari Brooks, Wellstar orthopedic surgeon

Keep Up With Your Prescriptions in Wellstar MyChart
Patients who use Wellstar retail pharmacies can now keep track of their prescriptions and request refills in Wellstar MyChart.
MyChart makes viewing your prescription information easy, so you never miss a dose and have all the information you need to take charge of your health.
Find all your prescription information by selecting Medications under the MyChart menu.
When your prescription is ready, you’ll receive a text message from MyChart.
Like our expert providers, Wellstar retail pharmacies are located close to home, in the same places you already receive care—Wellstar Cobb, Wellstar Kennestone, Wellstar Paulding and Wellstar Windy Hill Medical Centers and Wellstar Acworth, Wellstar East Cobb and Wellstar Vinings Health Parks.
Wellstar clinical pharmacists are expertly trained to understand your healthcare needs. With your medical history in mind, our pharmacists collaborate with your physicians on your prescribed medications to ensure you have the resources to live your healthiest life. We also offer counseling to make sure you know how to properly take your medications.

Your Men’s Health Playbook
Your late teens, 20s & 30s
Striving for top health performance
You may feel on top of your game—even unbeatable—In your 20s and 30s. You may be tempted to think, “Why even bother with a physical?” Yet this is training season for building up lifelong healthy habits.
Establish your care coach: In your late teens to early 20s, transition from your pediatrician and establish yourself with a primary care physician, nurse practitioner or physician assistant by scheduling a physical.
“When young men show up for preventive care, we talk about the future,” said Dr. Dean Seehusen, chair of Family & Community Medicine at Wellstar MCG Health Medical Center in Augusta. “Then we talk about what that’s going to take habit-wise. What you can do in your 60s and 70s is based on what you’re doing in your 20s, 30s and 40s.”
Stay on top of your stats: The information from your annual exam can help you stay on track to live out your vision, measured in part by important health stats—like glucose and cholesterol levels, body mass index and blood pressure. Staying on top of your trending numbers can help prevent heart disease, stroke and diabetes down the road.
It’s also a good time to talk about your vaccine status, such as tetanus (needed every 10 years) and HPV. To protect yourself and your partner, it’s important to test for human papillomavirus. Also known as HPV, it’s the most common sexually transmitted infection and can cause several types of cancer for men and women, even though you likely won’t have symptoms. You may have already received this vaccine in your teens, but if you haven’t yet, it’s recommended through the age of 26.
Men may also consider self-screening for testicular cancer through self-exams during these earlier healthcare years, according to John Aaron III, a physician assistant who cares for patients at Wellstar Family Medicine in Alpharetta.
Look for weaknesses: Make your health team aware of your family medical history, from heart disease and stroke to cancer. This will help them create a personalized health plan for you. You may need screenings or tests for certain health conditions at an earlier age than the average population.
Find a Men’s Health care team near you, including the Wellstar KSU Health Center for Kennesaw State University for students.

Meet Dr. Angello Lin, New Section Chief of Transplant Surgery at Wellstar MCG Health
Dr. Angello Lin, the new transplant surgery section chief at Wellstar MCG Health Medical Center, had a light bulb moment when he took three years off during his 23-year tenure as a surgeon at the Medical University of South Carolina.
He took a break to spend time in Savannah with his father, who had turned 90 and was having health issues. During that time, Dr. Lin had time to think and realized that although he had become a transplant surgeon because the work seemed dynamic, his work had not been very dynamic lately. He had been solely focused on performing the transplantations and taking care of patients for 14 years.
“I started to wonder if I could add some dynamism back by finding different and better ways to do a transplant,” he said.
The break served him well as Dr. Lin went on to become the first surgeon to successfully connect a pancreas and a kidney before putting it into the patient’s body, rather than putting them in separately. Implanting them as one organ with one arterial inflow and one venous outflow reduced the patient’s time in the operating room from four to six hours to two to three hours, making the procedure safer and giving patients the potential for a quicker recovery.
Dr. Lin, who graduated from Emory School of Medicine, found a renewed sense of purpose in innovation in surgery and decided he wanted to work at a hospital that would encourage his innovation. That led him to Wellstar MCG Health’s transplant center, which has received grants from the Mason Trust Foundation to enhance transplant research, education and patient care. The transplant center also performed a record 105 kidney transplants last year. “The surgery department here is very supportive of me trying new ways of doing things, and I was drawn to that,” he said.
Dr. Lin joined the hospital in February and is already working on a pilot project that infuses therapeutics that will hopefully reduce injuries to kidneys after transplantation from ischemia repercussion. He will also help the transplant center restart its pancreas transplant program.
Dr. Lin spends his time outside the hospital with his wife and three daughters: Jasmine, 24, who plans to go to medical school; Camille, 21, who is studying to become a pilot; and Abigail, 13, who is in eighth grade.
Born in Taiwan, Dr. Lin moved to Tybee Island as a teen and later graduated from Emory with a bachelor’s in chemistry. He first became interested in transplant surgery during his general surgery rotations as a fourth-year resident when he saw the difference transplantation made in patients’ lives. One story that stands out to him was when he was taking care of a retired chemistry professor, a liver transplant recipient who was near death. Although the patient was depressed, he told Dr. Lin about himself, including his favorite movie—"Dead Poets Society”—and about his dream to travel the world. The next day, Dr. Lin came into the patient’s room, stood on a chair and recited the famous poem from the film to encourage the patient.
“O Captain! my Captain! rise up and hear the bells,” he said. “Rise up—for you the flag is flung—for you the bugle trills.”
The patient went on to recover and sent Dr. Lin postcards from his travels around the world.
“After a successful kidney transplant, patients are so grateful and will say, ‘I can go to the bathroom again!’” he said. “They are excited to be able to do the everyday things our bodies do that we take for granted. It’s very touching.”
Following residency, Dr. Lin became the first trainee to complete Emory’s transplant fellowship in 2000.
Now Dr. Lin estimates he’s performed over 1,500 transplant surgeries. The most difficult part of the job remains working around the nationwide organ shortage. He has to be ready to drop everything when an organ is ready to be donated and, sadly, he also has to tell patients that they are at the mercy of the waitlist.
“They look to us to be the miracle workers, and some days we come close,” he said.

Wellstar MCG Health’s Stroke Center Renews its Best-in-Class Certification
Georgia’s oldest comprehensive stroke center at Wellstar MCG Health Medical Center was approved by The Joint Commission to renew its best-in-class certification.
The healthcare accrediting body has four advanced stroke certifications. Wellstar MCG Health has once again earned its most demanding certification—the Comprehensive Stroke Center (CSC) certification—which was designed for hospitals that can treat complex stroke cases.
Wellstar MCG Health’s stroke center, which provides care to a thousand patients annually, was the first hospital in Georgia to get the CSC certification when it was first offered in 2013.
Every two years, the program must get recertified, a process that requires surveyors from The Joint Commission to visit the center to observe practices and collect data, such as complication rates.
This year, two surveyors spent two days in April doing a comprehensive review of the stroke center.
Dr. Scott Rahimi, neurosurgical director of the stroke center, said this year’s review was the best they’ve had since becoming a CSC in 2013.
“This year we took care of more stroke patients than any other facility in the CSRA,” he said.
Eight hospitals in Georgia have the CSC certification, including Wellstar Kennestone, Wellstar MCG Health and Wellstar North Fulton Medical Centers, but Wellstar MCG Health is the only in the region with the advanced certification, said Stroke Program Manager Amanda Howard.
“This particular survey was very rewarding and made it worth all the hard work we do taking care of patients,” she said.

Wellstar Receives $5.5M Healthy Start Grant to Improve Maternal Outcomes in West Georgia
If it’s true that women’s health is community health, then it will take a community approach to overcome the biggest barriers to positive maternal health outcomes.
Georgia is facing a maternal mortality epidemic where Black and brown women are three to four times more likely than white women to die from childbirth. The state ranks among the worst in the nation for maternal mortality rates. Yet 89% of these deaths are preventable.
“For too many women in communities around our state, there is a lack of access to care, especially preventative care and screenings that can be lifesaving. At Wellstar, we’re doing something about it,” said Julie Teer, senior vice president of Wellstar and president of the Wellstar Foundation.
Over the past few years, Wellstar has been committed to addressing the increasing maternal mortality rates in Georgia through its doula labor program, which provides high-risk women with the additional support they need to have a healthy pregnancy. The doula assists them through the pregnancy, labor and delivery, as well as the immediate postpartum period.
Now, with the recent award of a $5.5 million Healthy Start grant from the Health Resources and Services Administration of the U.S. Department of Health and Human Services, Wellstar can expand to a more collaborative approach that will convene a community consortium composed of more than 20 diverse, multisector partners to advise and inform activities. The group will also develop and implement plans to improve perinatal outcomes.
The Wellstar Healthy Start program will integrate into the OB/GYN care delivery model at Wellstar to directly impact the communities with the greatest need, including Spalding, Butts and Troup counties. In fact, Troup County ranks among the worst maternal and infant mortality rates in the state.
This funding enables Wellstar to provide individual and group perinatal and parenting education, expand prenatal and postpartum care for high-risk patients through nurse navigators, and increase access to community-based doulas. Additionally, it will provide important wrap-around services and care coordination for the entire family for services that address individualized challenges directly related to racial disparity and the social determinants of health, such as housing, food insecurity, domestic violence, lack of education/employment and access to transportation.
Over the five-year span of this grant, the Healthy Start program will support 3,500 women, fathers, caregivers and infants at Wellstar West Georgia, Wellstar Spalding and Wellstar Sylvan Grove Medical Centers and beyond.
To learn more about the Wellstar Foundation and how you can get involved, visit wellstar.org/foundation.
This blog post is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $5.5 million with 0% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS or the U.S. government.

Norfolk Southern Donates $250,000 to Children’s Hospital of Georgia to Support Pediatric Behavioral Health
Representatives from Norfolk Southern, members of Wellstar Children’s Hospital of Georgia Philanthropy Board and Georgia Speaker of the House Jon Burns were all in Augusta to present Wellstar Children’s Hospital of Georgia with a donation of $250,000.
The funds will be used to support the Kisner Foundation & Friends Center for Pediatric Development, Behavioral Health and Wellness, which is expected to begin construction this fall. The center will bring together a variety of pediatric mental and behavioral services already offered at Wellstar Children’s Hospital of Georgia in partnership with Augusta University into one location. It will offer a multidisciplinary approach to care tailored to each child’s needs and will include services like testing and evaluation; referrals for psychotherapy and mental health services; physical, occupational and speech therapy; and connections for parents to ancillary services.
“Norfolk Southern is honored to support Wellstar Children’s Hospital of Georgia with a $250,000 donation for the vital development of a mental and behavioral health center. Our commitment to investing in initiatives that build strong, thriving communities aligns perfectly with the hospital’s mission to provide top-tier pediatric care. We believe that enhancing mental health services for children is a critical step toward fostering overall well-being and resilience for future generations,” said Kristin Wong, director corporate giving at Norfolk Southern.
The center will cost about $6 million to build. Along with construction costs, donations are used for programs already in place that will move into the completed center, such as testing materials for autism, learning disabilities and developmental delays.
“We offer those services now, but they’re scattered across our campus. We envision a place where we can bring these services together to make it more convenient and more accessible for our patients and their families. The money you’re donating today is going to help us move forward faster with that renovation,” said Wellstar Children’s Hospital of Georgia Pediatrician-in-Chief Dr. Valera Hudson.
Hudson, who is also the department chair of pediatrics at the Medical College of Georgia at Augusta University, emphasized that Wellstar Children’s Hospital of Georgia, and thereby the Kisner Center, will serve children in Augusta and across Georgia.
Jon Burns, the Speaker of the House for the Georgia House of Representatives, thanked Hudson for her tireless efforts to serve children across the state and pledged to continue his support for initiatives that improve the mental healthcare for children. He also thanked his wife, Dayle, and fellow Wellstar Children’ Hospital of Georgia philanthropy board members King and Beth Rocker for their efforts in helping to facilitate Norfolk Southern’s support, as well as board member Carol Parrish and state representatives Jodi Lott, Gloria Frazier, Butch Parrish and Karlton Howard.
“Public dollars can’t do it all. It takes partnership between the private sector and the public sector,” he said. “It takes a group of people working together to get things done.

Wellstar Kennestone Regional Medical Center Designated a Level I Trauma Hospital
MARIETTA, Ga. (May 31, 2024) – Wellstar Kennestone Regional Medical Center has achieved the prestigious Level I Trauma Center verification from the American College of Surgeons and designation from the Georgia Department of Public Health State Office of EMS and Trauma. The ACS verification is the gold standard for trauma centers nationwide.
Each hospital verified by the American College of Surgeons as a Level I Trauma Center must demonstrate that it provides the highest level of trauma care. The evaluated criteria range from prevention through rehabilitation across the broadest spectrum of injuries, as well as academic research that helps improve trauma outcomes.
“Wellstar strives to provide compassionate, world-class care to every person, every time. The designation of Wellstar Kennestone Regional Medical Center as a Level I Trauma Center further strengthens the network of quality trauma care that exists across Metro Atlanta and Georgia,” said Candice L. Saunders, President and CEO of Wellstar Health System.
Level I verification requires consistently delivering a high level of clinical expertise for a wide range of severe injuries at all times, and further improves patient outcomes through trauma research and education.
The Wellstar Trauma Network is the largest integrated trauma network in the State of Georgia with two Level I trauma centers (Wellstar Kennestone and Wellstar MCG Health Medical Centers), one Level II (Wellstar North Fulton Medical Center), one Level III (Wellstar Cobb Medical Center), and three Level IV (Wellstar West Georgia, Wellstar Paulding and Wellstar Spalding Medical Centers), along with a Pediatric Level II Trauma Center (Wellstar Children’s Hospital of Georgia at Wellstar MCG Health Medical Center) in Augusta.

Wellstar Helps Women Stay Healthy at Every Age
From adolescence through adulthood, Wellstar Women’s Health cares for women at every stage of life and encourages patients to stay up to date on essential screenings.
You may feel invincible in your 20s, but it’s important to start healthy, lifelong habits now. Schedule an annual physical exam with your primary care team so they can check important indicators of health over time, like blood pressure, glucose and cholesterol levels. Taking charge of your health early on lays the groundwork for a lifetime of well-being.
Find a women’s health clinician near you.
By age 21, women should get an annual pelvic exam and Pap smear with an OB/GYN. Depending on your results, you may not need another Pap smear for three years. You may also want to test for human papillomavirus, or HPV. HPV is the most common sexually transmitted infection and can cause several types of cancer, even though you may not have any symptoms. Your OB/GYN may also recommend monthly self-breast exams.
Adding a yearly mammogram at this stage (or sooner, if advised) is important. You can schedule your mammogram through either an OB/GYN or a primary care clinician. Modern mammography programs can reduce breast cancer mortality by more than 40%. Wellstar has several mammography locations and offers 3D mammograms, which can help detect breast cancer at early stages when it’s easier to treat.
Starting at age 45, you should talk to your primary care team about a screening test for colon cancer. Colonoscopies are the most common procedure to detect precancerous polyps and should be repeated every 10 years or sooner, depending on your personal and family history.
In your 50s, it’s important to maintain your relationship with your care team. Ask if you need a heart screening (coronary artery calcium scoring). Individuals with a history of smoking should inquire about lung cancer screenings. Since hormone changes can lead to osteoporosis, post-menopausal women should also consider a bone mineral density test.

Exercise to Enhance Your Stroke Recovery
The road to recovery after a stroke can be long and difficult. By following exercise recommendations from Wellstar’s rehabilitation care team, you can take an active role in the process and help shorten your journey.
According to the National Institutes of Health, falling can lead to delays in recovery for stroke survivors. Muscle stiffness and loss of balance are two common issues that contribute to increased fall risks. The expert providers at Wellstar work with patients and family members to develop individualized care plans that improve steadiness and flexibility. For added benefit, they also recommend you do the following exercises on your own.
Standing up and sitting down
Begin by sitting on a chair with a firm seat. Stand up fully and then slowly take a seat. Repeat as many times as you can tolerate initially. If necessary, use your hands to push into the standing position. Gradually progress to standing without the added assistance and completing more repetitions.
Step-ups
Begin by holding on to a stair rail. Step up onto the first step and then back down to the floor. Repeat as many times as you can tolerate initially. Step up with your stronger leg and lead with the weaker leg going down. Gradually progress to not holding on to the rail and increasing the number of repetitions.
Calf raises
Using a chair or countertop for balance, raise up onto your toes, lifting your heels completely off the floor. Slowly lower your heels back to the floor. Repeat as many times as you can tolerate initially. Gradually progress to not holding on and completing more repetitions.
Marching in place
Begin using a chair or countertop for balance and march in place for as many seconds as you can tolerate initially. Gradually progress to not holding on and marching in place for longer periods of time.
Shoulder flexion
Start with your arms at your side. With your palms facing each other, raise your arms in front of you as far as you can. Return to the starting position, then repeat.
Shoulder extension
Start with your arms at your side. With your palms facing each other, raise your arms behind you as far as you can. Return to the starting position, then repeat.
Shoulder abduction/adduction (lateral shoulder arm raises)
Extend your arms out to the side. Slowly raise your arms above your head. Return to the starting position, then repeat.
Elbow extension and flexion
Start with your arms at your sides, with your palms facing forward. Bend at your elbow so that your palm touches your shoulder. Return to the starting position, then repeat.
Wrist extension and flexion
Place your arms on a supported surface such as a table or desk, leaving your wrists free to move. Turn your palms up toward the ceiling and bend your wrists up and down.
Finger flexing and extending
Place your forearms on a surface such as a table or your lap with your palms facing up. Make a tight fist then open your hand and extend your fingers out until they are straight.
Establishing a regular exercise routine outside of your scheduled therapy appointments is important for your recovery. Perhaps equally important is completing the routine in a safe manner to avoid falling and to maximize your results. The experts at Wellstar suggest following these tips to maintain your safety.
If you have any questions, talk with your doctor, physical therapist or occupational therapist. Learn more about the expert care from Wellstar’s inpatient rehabilitation program.
For more information on Wellstar Roosevelt’s specialty rehabilitation services, visit rooseveltrecovery.com.

A Recipe for Success: Heart-healthy Dishes to Reduce Stroke Risk
If you’ve had a stroke, you don’t have to replace flavorful cuisine with bland foods on your journey to recovery.
There are easy, delicious meal options that follow American Heart Association nutrition guidelines for lowering your risk of another stroke. More fiber, whole grains, fruit, vegetables and lean protein, with less trans fat, saturated fat, sodium and sugar are key to supporting your recovery efforts. Rehabilitation care teams and dietitians at Wellstar recommend keeping meals and snacks interesting with variety and new recipes like these.
Coconut Truffles satisfy your sweet tooth without any added sugar.
Ingredients:
12 medjool dates, pitted
2 tablespoons water
4 tablespoons unsweetened cocoa powder
½ cup puffed brown rice
½ cup shredded unsweetened dried coconut
Directions:
Southwestern-Style Breakfast Casserole is a great way to start your morning.
Ingredients:
6 slices hearty whole-grain bread, cut into cubes
1 10-ounce package frozen chopped spinach, thawed and liquid squeezed out
1 7-ounce jar roasted red peppers, drained and chopped (or 1 red bell pepper, roasted and chopped)
1 ½ cups (6 ounces) Mexican-style cheese
3 cups non-fat milk
8 ounces egg substitute
1 teaspoon garlic powder
1 teaspoon cumin
½ teaspoon black pepper
½ teaspoon salt
Directions:
For more heart-healthy recipes, visit American Heart Association Recipes.
To learn more about how you can partner with Wellstar rehabilitation care teams to reduce your risk of another stroke, visit https://www.wellstar.org/medical-services/treatments-procedures/rehabilitation-services/neuro-rehabilitation..
Becker’s Hospital Review Recognizes Black Healthcare Leaders to Know for 2024
Wellstar is proud to celebrate four of our leaders who have been selected for Becker’s Black Healthcare Leaders to Know. Becker’s Hospital Review is one of the hospital industry’s leading publication for insights and information.
At Wellstar, we value the unique perspectives, backgrounds, and ideals of all who come through our doors. By leveraging our similarities and differences, collectively, we create healthier communities. Our engaged and diverse workforce learns and grows while providing our patients with world-class healthcare.
Join us in congratulating our recognized leaders: Le Joyce Naylor, senior vice president and chief diversity, equity and inclusion officer, David Jones, executive vice president and chief human resources officer, Mary Chatman, RN, PhD, executive vice president of Acute Care Operations, and Ralph Turner, president of Wellstar MCG Health.
Le Joyce Naylor. Senior Vice President and Chief Diversity, Equity and Inclusion Officer at Wellstar Health System (Marietta, Ga.). Ms. Naylor offers systemwide thought leadership, strategic thinking and program direction for Wellstar Health System's diversity, equity and inclusion initiatives. Her responsibilities include the design and implementation of programs to advance diversity efforts, achieving measurable outcomes and leading the health system's diversity and inclusion advisory council. Among her many accomplishments are the formation of 11 business resource groups, the recalibration of 11 diversity and inclusion councils, and the engagement of team members in inclusive virtual and in-person conversations about everyday topics.
David A. Jones. Executive Vice President and CHRO at Wellstar Health System (Marietta, Ga.). Mr. Jones is executive vice president and CHRO for Wellstar. In this role, he has overall systemwide responsibility for establishing, enabling and maintaining organizational effectiveness and a positive employee relations environment. He is responsible for providing senior executive leadership and oversight for the delivery of HR solutions to the business, including human capital strategy, culture design and change management, team effectiveness, workforce planning, performance management planning, succession management, diversity and inclusion, and employee relations. Previously, he served as CHRO at Stanford University and Oakland, Calif.-based Kaiser Permanente's senior vice president of national human resources. Mr. Jones' nearly 30-year career in human resources has spanned across the healthcare, academic and corporate sectors.
Mary Chatman, RN, PhD. Executive Vice President at Wellstar Health System (Marietta, Ga.). Dr. Chatman's leadership and collaborative work ethic can be seen throughout the health system. She manages a team of more than 10,000 staff members. Dr. Chatman is a seasoned leader with over 30 years of healthcare experience.
Ralph Turner. Senior Vice President and Hospital President of Wellstar MCG Health (Augusta, Ga.). Mr. Turner was appointed as Wellstar MCG Health president in April 2024. He assumed the role after serving on an interim basis. Wellstar MCG Health includes a 478-bed adult hospital, 154-bed Children's Hospital of Georgia, the Georgia Cancer Center, and over 80 outpatient clinics. Prior, he served as senior vice president and president for Hiram, Ga.-based Wellstar Paulding Medical Center since 2022.
Congratulations to our leaders!

Wellstar Transforms Patient Check-in with CLEAR
Wellstar and CLEAR are launching an initiative that simplifies and speeds up the patient check-in process.
Wellstar patients who opt-in to use this free service can verify their identity with CLEAR before their appointment to simplify check-in once they arrive. It only requires two steps:
Why CLEAR?
CLEAR’s technology is trusted and secure. At the heart of this first-of-its-kind partnership is CLEAR's pioneering integration with Epic, a leader in the electronic health records market, to power seamless patient registration and on-site check-in. Wellstar co-developed the integration and is the first health system to utilize the CLEAR Verified technology application.
“Identity is foundational to making patient experiences safer, easier and more efficient in healthcare,” said CLEAR CEO Caryn Seidman Becker. “CLEAR’s collaboration with Wellstar and Epic will bring frictionless and secure check-in for patients. With the launch of this seamless experience, CLEAR is one step closer in our effort to replace the clipboard in healthcare.”
CLEAR’s identity platform is secure and HIPAA-compliant, and many patients may already be familiar with the technology. It’s used locally at Hartsfield-Jackson Atlanta International Airport and State Farm Arena.
Keeping care convenient
This new check-in option reflects the Wellstar vision of delivering world-class healthcare to every person, every time.
“Our patients’ time is precious. Introducing CLEAR’s proven, secure technology will help make the check-in process even more efficient and safe,” said Dr. Hank Capps, executive vice president and chief information and digital officer for Wellstar. “We are committed to building an ecosystem of care that includes technologies that have never been used in healthcare. When combined with compassionate care from Wellstar clinicians, we will deliver a truly world-class experience.”
CLEAR check-in is available at:
Register now and try the experience at your next appointment: clearme.com/wellstar.

Wellstar MCG Health Medical Center opens new MRI suites with funding secured by Sen. Jon Ossoff
U.S. Senator Jon Ossoff joined Wellstar and Wellstar MCG Health Medical Center leadership in cutting the ribbon on two new MRI suites that feature state-of-the-art magnetic resonance imaging (MRI) machines. The machines were purchased with $3.5 million in federal funds that Ossoff secured with bipartisan support from the U.S. Senate in March 2022.
The critically needed units are located in newly designed and built MRI suites that are conveniently located between Wellstar MCG Health and Wellstar Children’s Hospital of Georgia. The updated technology allows for faster image scanning, better quality scans, and better patient access and comfort for adults and children. The new machines and suites replace two aging machines that were located in different parts of the medical campus.
“Senator Ossoff listened to our friends at Augusta University when they shared how adults and children in Augusta and throughout Georgia would benefit from two new, state-of-the-art MRI machines,” said Ralph Turner, president of Wellstar MCG Health. “Today, we celebrate Senator Ossoff’s leadership and work to obtain federal funding that will improve the healthcare experience for people across our great state for years to come.”
“The technology in these new machines is phenomenal and will make a noticeable difference in the care of every patient and physician who uses them,” said Dr. Annette Johnson, department chair for radiology at Wellstar MCG Health and academic chair and professor of radiology and imaging at the Medical College of Georgia at Augusta University. “These state-of-the-art machines can compensate for patient breathing and other motion, anticipating the patient’s movement and modifying the scanning techniques to adapt to the motion. This level of sophistication results in a higher quality scan in less time.”
For context, a typical MRI exam consists of five to 10 individual scans, each of which takes several minutes to complete. If a patient moves during one of the scans, the scan must be repeated. This happens frequently since it’s very hard for people to be perfectly still for long periods of time.
“If everything goes perfectly, the whole exam for a cervical spine MRI, for example, should take 25 minutes. But if the patient moves a little bit during the exam, it may take 10 or 15 additional minutes because scans have to be repeated, which makes the experience more difficult to tolerate as a patient,” said Johnson.
Cutting down the amount of time spent in the machine is a win-win-win. In addition to improving the quality of the scans, it is more comfortable for the patient, reduces wait times for other patients and allows for more patients to be seen.
“I don’t know if it qualifies as AI, but it’s super-smart technology,” said Johnson. “It’s motion-sensing and even predicts the patient’s movements. This results in fewer repeat scans, which improves the patient experience and enables more people to receive scans.”
Wellstar MCG Health also has a mobile MRI machine that is located outside of Professional Building One.
“This will be so much better for our patients, being closer to other support services for pediatric patients and wayfinding for all patients. All patients who receive a MRI will now got to the same waiting room, instead of three different waiting rooms,” Johnson said.
The new machine has a stronger gradient within the magnetic field, Johnson explained, which translates to higher-resolution, thin-section imaging. This means, for example, that radiologists and other physicians will be able to more clearly see the margins of a prostate cancer or the valves of the heart.
“You can see fine detail so much better, so you can make more confident diagnostic and treatment decisions,” she said. “You can get literally a half a millimeter slice thickness with this new equipment. That’s huge for us as we help patients and physicians make the best possible decisions for a person’s care.”
The new technology also improves the ability to adapt to individual patient body shape and to better scan patients who have implanted devices such as pacemakers.
Radiology Manager Felicia Ford said she is very happy to begin working with the new machines. She even volunteered to be among the first people to be scanned, just to test it.
Ford is looking forward to providing her patients with a better experience in addition to better quality MRI scans.
“It’s really nice,” she said. “I was impressed. It’s comfortable.”

CLEAR Partners with Wellstar Health System to Launch Seamless and Secure Check-in Across Locations
Atlanta, GA -- CLEAR (NYSE: YOU), the secure identity company, and Wellstar Health System, one of the largest healthcare systems in Georgia, are launching a new initiative to further simplify and speed up the patient check-in process. The first pilot location is live with further rollout expected in the second half of 2024.
CLEAR has successfully integrated with Wellstar to enable patient registration and on-site check-in through CLEAR Verified. Wellstar co-developed the integration and is the first health system to utilize the CLEAR Verified technology application, which will become an out-of-the-box integration that CLEAR can easily implement for other healthcare partners who use Epic.
Wellstar patients who opt-in to use CLEAR’s proven technology will enjoy a smooth on-site check-in by simply verifying their identity ahead of time. Wellstar patients will receive a text a few days before their scheduled appointment to check-in using CLEAR. On appointment day participating patients simply need to take a selfie at the Wellstar CLEAR Verified kiosk to check-in for their appointment.
“Identity is foundational to making patient experiences safer, easier, and more efficient in healthcare,” said CLEAR CEO, Caryn Seidman Becker. “CLEAR’s collaboration with Wellstar Health System will bring a streamlined and secure check-in experience for patients. With the launch of this new experience, CLEAR is one step closer in our effort to replace the clipboard in healthcare.”
“Our patients’ time is precious. Introducing CLEAR’s proven secure technology will help make the check-in process even more efficient and safe,” said Dr. Hank Capps, FAAFP, EVP and Chief Information and Digital Officer for Wellstar Health System, and President of Catalyst by Wellstar. “We are committed to building an ecosystem of care that includes technologies that have never been used in healthcare. When combined with compassionate care from Wellstar clinicians, we will deliver a truly world-class experience.”
About CLEAR
CLEAR's mission is to create frictionless experiences. With more than 22 million members and a growing network of partners across the world, CLEAR's identity platform is transforming the way people live, work, and travel. Whether you are traveling, at the stadium, or on your phone, CLEAR connects you to the things that make you, you – making everyday experiences easier, more secure, and friction-free. CLEAR is committed to privacy done right. Members are always in control of their own information, and we never sell member data. For more information, visit clearme.com.
Forward-Looking Statements
This release may contain statements that constitute forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. Investors are cautioned that any and such forward-looking statements are not guarantees of future performance or results and involve risks and uncertainties, and that actual results, developments and events may differ materially from those in the forward-looking statements as a result of various factors, including those described in the Company's filings within the Securities and Exchange Commission, including the sections titled "Risk Factors" in our Annual Report on Form 10- K. The Company disclaims any obligation to update any forward-looking statements contained herein.
Epic is a registered trademark of Epic Systems Corporation.
Contact
[email protected]

MichaelCare
Presiding over weddings is one way that the Reverend Michael Teston, ThM, gives back to his community after retiring as a full-time pastor.

One recent wedding was quite different than the rest. It was with heartfelt pride that the pastor looked on as the groom—the man Michael credits with saving his life—said his vows.
“Fiyin, do you take Courtnee to be your lawfully wedded wife?” Michael asked his head and neck cancer specialist.
“I do,” Dr. Fiyin Sokoya replied, standing happily as his former patient—now friend, spiritual advisor and premarital counselor—joined him with his wife in holy matrimony.
A few years earlier, an unexpected diagnosis brought the two men together as they formed a bond that exceeded the typical doctor-patient relationship.
It began when Michael noticed a knot in his left cheek. He thought he had an infected lymph node so he went to an ear, nose and throat (ENT) doctor to get it checked out. The prognosis was that the knot was likely non-cancerous, but worth getting removed because it was growing rapidly and increased the risk for cancer. The clergyman was referred to Dr. Fiyin Sokoya, a head and neck cancer specialist and facial plastic surgeon at Wellstar North Fulton Medical Center.
Dr. Sokoya surgically removed the tumor using techniques similar to a facelift. This helped the scars heal well and meant minimal downtime during the healing process.
“If you look at my face now, you couldn’t tell,” Michael shared. “Dr. Sokoya did a phenomenal job.”
As a precaution and part of standard practice at Wellstar, the tumor taken from his face went to specialized head and neck pathologists for testing.
“I went into the doctor’s office for a follow-up visit,” Michael remembered. “The doctor said, ‘Unfortunately, it’s cancer.’”
The tumor was a rare type of chronic lymphocytic leukemia and small lymphocytic lymphoma.
“Well, that’s not what I was expecting!” Michael remembered thinking at the time. “I thought it was just a benign tumor. But Dr. Sokoya kept his manner calm, kind and never rushed. He explained things in a non-technical way to make sure I understood.”
Along with Dr. Sokoya’s demeanor, the reverend’s belief that no matter what happens, a higher power is watching out for him helped. Michael said, “My heart rate didn’t go up one bit. I never had a moment of panic.”
Fortunately, Michael was already in the right place for his care.
“We’ve become the destination center for advanced head and neck cancer care,” Dr. Sokoya said. “We can take care of him whatever his needs may be with top-notch physicians who empathize and display emotional intelligence while connecting on a human level throughout treatment.”
Aside from the surgery, Michael did not need further treatment, other than regular monitoring and bloodwork.
“Michael ended up not needing chemo because we caught it early and his medical oncologist is able to watch it closely in case any symptoms develop again,” Dr. Sokoya said.

Wellstar Sylvan Grove Medical Center Honored with the Georgia Oglethorpe Award
Wellstar Sylvan Grove Medical Center has been named a first-time Georgia Oglethorpe Award winner. The Sterling Council, established in 1992, is a public/private not-for-profit corporation supported by the Executive Office of the Governor. The Council oversees the Governor’s Sterling Award for Performance Excellence and the Georgia Oglethorpe Award, which is based on the national Malcolm Baldrige Award, with Awards being presented annually to high performing, role-model organizations, both private and public, who demonstrate superior management approaches and role model results.
Wellstar Sylvan Grove is a nonprofit, critical access hospital in Jackson, Georgia and one of 11 Wellstar Health System hospitals. The hospital operates with 25 in-patient/swing beds (subacute rehab) and a 13-bed emergency department. The swing bed unit serves patients from all over the country, and the emergency department treats over 17,000 patients annually. Wellstar Sylvan Grove receives patients from across the nation because of their excellent reputation for rehabilitative care. “Together we can achieve more” describes the mindset of the Wellstar Sylvan Grove team. The hospital’s teamwork approach is the key driver of maintaining zero hospital-acquired infections for over three years and consistently remaining in the top 75th percentile for patient satisfaction as a facility.
Wellstar Sylvan Grove consistently remains one of the top-performing hospitals on the Great Place to Work® Survey, a national employee engagement survey, which resulted in the health system being named one of the Fortune 100 Best Companies to Work For®, earning the award in 2024 for the sixth time. The family culture extends outside of the four walls of the hospital to the people in the community. Wellstar Sylvan Grove participates in many community events, including a mobile market that helps to provide nutritious food and health education to the community at no cost.
Wellstar Sylvan Grove Medical Center is a first-time recipient of the Georgia Oglethorpe Award and is the sixth hospital that is part of the Wellstar Health System to be recognized with the Sterling Oglethorpe Award.
Wellstar Sylvan Grove will be formally recognized on Friday, May 31, at the Hyatt Regency Orlando at a banquet honoring their accomplishments and attainment of this recognition.

Honor Cancer Survivors Day with Wellstar
Wellstar supports people with cancer throughout their journeys, from early screenings to diagnosis to treatment. But our encouragement and dedication to delivering world-class, compassionate care doesn’t end in remission.
Across our system, Wellstar honors the bravery and strength of survivors every day, rejoicing in each milestone. This National Cancer Survivors Day, June 2, we are proud to pay tribute to the people who have conquered cancer and offer hope to those still fighting.
This year’s Cancer Survivors Day theme—In the Joy of Living, Hope Grows—exemplifies our commitment to being a steadfast source of encouragement for cancer survivors and fighters across Georgia.
“On Cancer Survivors Day, we reflect on our patients’ journeys and cherish victories over cancer. We also offer compassion and support for people currently fighting cancer, so they and their loved ones know they’re not alone,” said Wellstar Director of Oncology Melissa Higdon.
Several Wellstar facilities will host events—and you can be a part of the celebration!
Wellstar Cobb Medical Center
May 31
12 to 2 PM
1700 Hospital South Drive, Austell
Behind the building in the garden and parking lot area
To RSVP, contact Ashley Dapremont at
[email protected]
or
(470) 732-4523.
Wellstar Douglas Medical Center
June 1
11 AM to 2 PM
8954 Hospital Drive, Douglasville
Surgical services lobby
To RSVP, contact Diane Harris at
[email protected]
or
(470) 644-6613.
Wellstar Kennestone Regional Medical Center
June 1
11 AM to 2 PM
320 Kennestone Hospital Blvd., Marietta
First floor
To RSVP, contact Nancy Page at
[email protected]
or
(470) 793-7470.
Wellstar Paulding Medical Center
June 2
1 to 4 PM
144 Bill Carruth Parkway, Hiram
Second floor auditorium
To RSVP, contact Kellie Mitchell at
[email protected]
or
(470) 644-8106.
Wellstar West Georgia Medical Center
June 2
1 to 3 PM
111 Medical Drive, LaGrange
Enoch Callaway Cancer Center
To RSVP, contact Sarah Hersey at
[email protected]
or
(706) 845-3848.
Wellstar North Fulton Medical Center
June 2
2 to 4 PM
3000 Hospital Blvd., Roswell
Main lobby in hospital
To RSVP, contact Pam Plasket at
[email protected]
or
(770) 410-4556.
Wellstar Spalding Medical Center
June 5
12 to 2 PM
Drive-thru event
608 South 8th St., Griffin
Women’s Center
To RSVP, contact Sherry Connell at
[email protected]
or
(470) 935-5526.
Learn more about cancer care at Wellstar.

Cobb County Mother and Son Make Service A Lifestyle
Determination and service are family traits shared by the mother-son duo of Claudette Owens and her son Mayor Michael Owens of Mableton. The two have been serving their community in Cobb County for decades leading Michael to become the first Mayor of Mableton in 2023.
Claudette found her calling in nursing and served at Wellstar Cobb Medical Center from October 1998 to April 2012 when she retired. As we celebrate National Nurses week, she expressed that “once you are a nurse, you are always a nurse.”
During her time at Wellstar, she was a staff nurse and a charge nurse. “I think all nurses probably feel the same way. When our patients come in with chest pain, shortness of breath and chest pains so unstable, it is such a good feeling to care for them and bring them back to good health. That was my reward from Wellstar Cobb Hospital when I served on 2 North.”
At that time, her son Michael was pursuing his dreams and attending college. “If he set his mind to do something, he was going to find a way to do it,” Claudette said. “I think determination was his guiding force.”
On the eve of Mother’s Day weekend, Claudette fondly remembers her son when he was young. “He would bring me little pictures and we would go over them. He played basketball with his friends and brothers and was even into modeling and acting. He always kept me busy too because I was always running him here and there, but it was really fun for me.”
Michael started his life of service as a teenager by joining the United States Marine Corps before going on to college. “He’s always been moving towards something,” she said.
“I joined the Marines at 17. My father was in the Marines and my grandfather was in the Navy. Leadership is an extension of serving my country – I am now serving locally,” Michael said.
After enlisting with the Marines, Michael graduated from high school and went to Paris Island for basic training. He served for eight years and then attended North Carolina A&T State University, Georgia Institute of Technology, Harvard University and the U.S. Army War College. He launched a career in cybersecurity and dedicated time to public service. When Cobb County residents voted to create the City of Mableton in 2022, Michael set his sights on his next chapter of community service.
Michael’s drive and inspiration is evident in his mother. “Before she was a nurse, she opened her own beauty salon in a small town in North Carolina,” he said.
Michael’s fondest memory of his mom is when she became a registered nurse. “She inspired me, and she still inspires me. She has always had an appetite for the world and working hard. She was relentless in wanting the best for us as a wife, mother and daughter. She was constantly trying to be everywhere at the same time.”
As Claudette reflected on her time as a nurse, she recalls, “I was welcomed from the very beginning. I always felt welcome there [at Wellstar] and I still feel that way today.”
Michael shared that some of his mother’s best friends served alongside her.
“I used my vacation time back then to make sure to get our family together,” she remembers describing the summers when she would get her entire family, including five children, their spouses and grandchildren together.
The camaraderie she experienced on the floor with her fellow nurses is memorable. “And we all knew one another’s children even though we didn’t see them, but we knew when there was a graduation or birthday.”
Now that she is retired, Claudette is still active in the Mableton community, attending events and enjoying many of the activities the city has to offer, and spending time in her garden and with her family.
For Michael, his service is about “improving the quality of life for everyone.” With strong role models growing up and in adulthood, he is committed to his community. After spending the first year of his term “putting the blocks together” for the newly established city, he’s excited about Mableton 2045, a comprehensive citywide plan that’s being developed.
“The goal is to come up with a flexible and comprehensive plan to determine how the city is going to change and build,” he explained.
Mableton is now the largest city in Cobb County and home to 80,000 people.
The mayor and his mother will have much to celebrate this Mother’s Day, including their legacy of serving their growing community.

Spotting a Stroke FAST
When someone has a stroke, it’s crucial that they get treatment right away.
If you think you or someone else is having a stroke, call 911 immediately. Ambulance crews can start treatment on the way to the hospital, speeding up care and saving brainpower.
“Many people think that they can sleep it off, or that they can go to bed and they'll be better in the morning,” said Dr. Rishi Gupta, Wellstar director of stroke care. “If you have a loss of sensation, you cannot move your arm or your leg, you have trouble speaking or you have trouble with your vision, the faster you get to the emergency room, the more likely we are to reverse your disability.”
Learn the warning signs of a stroke, and if you notice any of these in yourself or someone else, BE FAST.
Reduce your risk of a stroke by living a healthy lifestyle. Your Wellstar provider can partner with you in creating a treatment plan to stay in good health. To learn more about brain, spine and nerve health services at Wellstar, visit our neuro care page or call (770) 956-STAR (7827).

Wellstar Opens New Urgent Care Centers
Wellstar has three new urgent care centers in Austell, Rome and Woodstock to serve our community’s growing healthcare needs. These locations provide convenient care for minor emergencies, illnesses and injuries.
Walk-ins are always welcome, but you also have the option to book a visit online at the time that works best for you. Booking online can help reduce your wait time once you arrive.
Our three new Wellstar Urgent Care locations:
1025 East-West Connector
Austell, GA 30106
(678) 273-3071
Monday - Friday, 8 AM - 8 PM; Saturday - Sunday, 8 AM - 4 PM
Urgent Care Check-In at this location
1314 Turner McCall Blvd.
Rome, GA 30161
(706) 728-3240
Monday - Friday, 8 AM - 8 PM; Saturday - Sunday, 8 AM - 4 PM
Urgent Care Check-In at this location
4477 Towne Lake Parkway
Woodstock, GA 30189
(770) 249-5620
Monday - Friday, 8 AM - 8 PM; Saturday - Sunday, 8 AM - 4 PM
Urgent Care Check-In at this location
In addition to the three new locations, Wellstar Urgent Care in Kennesaw has relocated to a larger space only a mile from its previous location. Visit us at:
3980 Jiles Road
Kennesaw, GA 30144
(770) 426-5665
Seven days a week, 8 AM to 7:30 PM
Urgent Care Check-In at this location
Wellstar Urgent Care provides:

Make Mental Health Your Habit
Your body supports you in everything you do, from everyday activities like grocery shopping to milestones and memories with friends and family.
But while you may make sure you eat healthy, get your exercise and see your doctor to keep up with your physical health, it’s important to check in on your mental health, too.
Wellstar offers a full range of behavioral health services close to home in convenient locations, so you can feel your best both physically and mentally.
If you’re dealing with feelings of anxiety and depression, you may turn to your primary care physician or another healthcare provider for help. Wellstar is removing barriers to behavioral healthcare by integrating those services into many of our locations.
On-site behavioral health providers work at many of our primary care and specialty clinics, making it a little easier to take that first step in improving your mental health. Wellstar also provides access to on-site and virtual behavioral health specialists in hospital emergency departments and on the medical floors.
“We know that patients are already struggling with stigma, and sometimes it takes a lot for a patient to come into care with a behavioral health professional, and we wanted to remove that stigma,” said Dr. Ryan Breshears, chief behavioral health officer at Wellstar.
About 1 in 3 patients with a physical health condition also could benefit from some form of mental health support, Dr. Breshears said. Wellstar providers work together across specialties to ensure each patient receives “whole person care”—addressing both their mental and physical well-being.
“When you address the mental health components that an individual is dealing with, you’re going to improve the physical outcomes,” Dr. Breshears said. “In the same way, if you address the physical health outcomes, you’re probably going to provide care that improves the mental health outcomes as well.”
Wellstar Psychologist Dr. Shawn Coyne works with cardiac patients to provide that whole person care to patients like John Petrick and his daughter Janin as they adjust to cardiac diagnoses.
Cardiac health and behavioral health are closely tied, Dr. Coyne said—if someone is depressed, they are twice as likely to have a cardiac health issue or twice as likely to experience a second cardiac event. Heart patients are also three times as likely to be depressed as the general population.
In addition to cardiovascular behavioral medicine, Wellstar also offers several other specialized programs to assist patients with the mental and emotional challenges of a medical condition:
With our PeopleCare approach, Wellstar providers tailor care to each patient, taking the time to get to know their needs and create a customized care plan.
“You as the patient are part of the treatment team,” Dr. Coyne said. “You are involved, you can participate, you give feedback, you engage and we get a better end product when we work as a strong team.”
To learn more about outpatient behavioral health services, call (770) 644-1570.
If you or a loved one requires immediate care for a behavioral health condition, our inpatient behavioral health units provide 24-hour care for adults ages 18 and older.
Inpatient behavioral health services include round-the-clock monitoring, medication management, individual and group therapy, and educational resources for both the patient and their family.
If you have questions, you can reach our Behavioral Health Assessment & Resource Center anytime at (470) 732-3789. However, in the case of an emergency, call 911 or go to the nearest emergency department.

Wellstar Appoints John Hatfield Executive Vice President and Chief External Affairs Officer
Marietta, Ga. (May 1, 2024) – Wellstar Health System has selected John Hatfield as Executive Vice President and Chief External Affairs Officer. He will lead the nonprofit community health system’s Marketing, Communications, Government Relations, Community Development and Foundation teams in a new integrated group called External Affairs.
“We serve Georgia communities in a challenging, rapidly changing environment for healthcare. It is increasingly vital that we engage effectively with our stakeholders, including policymakers, civic and community leaders, and the media. I am confident we found the right individual to lead this new group,” said Candice L. Saunders, President and CEO of Wellstar.
Through a 30-year career in public affairs, John has held senior executive positions with large corporations, public relations agencies, political campaigns and elected officials. Most recently, John served as Vice President of Corporate Communications at Norfolk Southern Corporation, where he was responsible for brand strategy, reputation management, strategic communications, community affairs and corporate giving, including the Norfolk Southern Foundation. He previously worked in the electric utility industry, where he built strong advocacy and local community engagement programs.
John and his teams will work collaboratively with donors, patients, families, media, legislators and community partners to raise awareness and build support for Wellstar’s vision and efforts to transform healthcare.
Before beginning his professional career, John received his bachelor’s degree in politics from Princeton University. He lives in Buckhead with his wife and daughter.

Make Health Your Habit to Prevent Stroke
While strokes have become relatively common—more than 795,000 people in the United States have a stroke each year, according to the Centers for Disease Control and Prevention—many risk factors for stroke can be managed in partnership with your healthcare provider.
Manage your risk factors
Factors that can increase your risk of experiencing a stroke include:
High blood pressure
Hypertension, or elevated blood pressure, increases the risk of a stroke. Stay up to date on your annual physicals to know your blood pressure levels, and if you have hypertension, talk to your provider about managing it. “High blood pressure is the most modifiable risk factor, meaning it’s the one that is most treatable and has the most impact on one’s risk,” said Wellstar Neurologist Dr. Ashis Tayal. “It is vastly underdiagnosed and when it is treated, it’s often undertreated.”
High cholesterol
Cholesterol can build up and lead to clotting in the blood, which can cause a stroke if the clot travels and blocks blood flow to the brain. Your primary care provider can help you monitor your cholesterol with a blood test and manage levels with medications or lifestyle changes.
Diabetes
People with diabetes are at increased risk of experiencing a stroke. Talk to your provider about diabetes screenings. If you are diabetic, discuss managing the condition with your provider.
Smoking
Smoking can increase your risk of a stroke, so if you are a smoker, it is beneficial to quit. “Cigarettes accelerate atherosclerosis, or clogging in the arteries, and cause inflammation in blood vessels that then increases people’s risk of stroke and heart attack,” Dr. Tayal said.
Atrial fibrillation
Atrial fibrillation, a heart arrythmia, can cause clots that then travel to the brain, leading to a stroke, according to Dr. Tayal. If you have atrial fibrillation, also known as AFib, partner with your healthcare provider to manage the condition.
Other risk factors
While many of these risk factors can be controlled through medication or lifestyle changes in collaboration with a healthcare provider, other risk factors for stroke can be out of your control. People of any age can experience a stroke, but stroke risk increases with age.
The risk of having a first stroke is nearly twice as high for Black adults as for white adults, and Black adults and Pacific Islander adults have the highest rates of death from stroke, according to the CDC. Hypertension is more common in Black patients, according to Dr. Tayal. People in rural communities may also experience higher rates of stroke due to limited access to healthcare and nutritious foods, he added.
To help lower stroke rates in our communities, Wellstar Community Health will distribute over 100 blood pressure cuffs in 2024 and educate community members about stroke risk and blood pressure monitoring at Wellstar Mobile Markets. The team will identify and distribute blood pressure home monitors to those coming to the markets who are diagnosed with high blood pressure, on blood pressure medication and do not have a home monitor.
Live to the Beat. Powered by Wellstar. is a pilot program to help community members at two East Point churches take charge of their cardiovascular health. Through the program, participants will meet monthly with a Wellstar Community Health community health worker to have their blood pressure checked and discuss ways to keep their heart healthy, such as proper nutrition, exercise and caring for mental health.
How to recognize a stroke
Learn the warning signs of a stroke, and if you notice any of these in yourself or someone else, BE FAST and call 911 right away.
Balance
Look for a sudden loss of balance or coordination. This can also appear as a sudden, severe headache or dizziness.
Eyes
Blurred vision, double vision or loss of vision can be signs of a stroke. If you think someone else may be having a stroke, ask if they are having trouble seeing out of one or both eyes.
Face
One side of the face may be feeling numb or appear to be drooping. Ask the person to smile and see if it appears uneven.
Arms
Check for sudden arm weakness or numbness. See if the person can lift both arms without one drifting downward.
Speech
Watch out for slurred speech or difficulty speaking. Ask the person to repeat a simple sentence to find out if they are having trouble talking.
Time
Don’t wait to seek care. If you notice any of these symptoms, call 911 immediately. The more treatment is delayed, the more the brain is damaged.

Live to the Beat. Powered by Wellstar. Connects Community Members with Heart Health Resources
Live to the Beat. Powered by Wellstar. is an initiative of the Wellstar Center for Health Equity and Wellstar Center for Cardiovascular Care, in collaboration with the American Heart Association, the CDC Foundation and Million Hearts. Through the program, participants will meet monthly with a Wellstar Community Health community health worker (CHW) to have their blood pressure checked and discuss ways to keep their heart healthy, such as proper nutrition, exercise and caring for mental health.
Funding has been provided by the Wellstar Foundation to support a partnership with the Georgia Department of Public Health Chronic Disease Prevention Section for a CHW, who is trained using a Morehouse School of Medicine education curriculum.
Participants for the program have been identified through the Wellstar Congregational Health Network, which partners with local faith communities to connect congregants with health resources. Live to the Beat. Powered by Wellstar. will launch in May with 50 congregants from First Baptist Church East Point and Mount Olive Seventh Day Adventist Church, also in East Point. Participants will receive blood pressure cuffs and other tools for promoting health and wellbeing.
The program is one of several Wellstar community initiatives to address social determinants of health, or the non-medical factors that can affect someone’s well-being, such as access to nutritious foods, housing and education.
“If we want to reduce poor health outcomes and reduce heart attacks and stroke in our community, we have to also look at all those other factors at play,” said Wellstar Assistant Vice President for Community Health and Wellstar Center for Health Equity Elise Lockamy-Kassim. “If an individual does not have access to food and we expect them to maintain good heart health, what could happen is they have to resort to having limited nutrition. They may choose high calorie foods just to feel full, not necessarily nutritious foods. Not having food also contributes to stress, which we know contributes to weakening your body.”
The Wellstar Find Help tool connects community members to assistance for housing, transportation, food and other resources.
Learn more about the Wellstar Center for Health Equity. To learn more about the national Live to the Beat campaign, visit Live To The Beat.
Wellstar Experts Treat Head & Neck Cancers, STAT
At Wellstar, every patient’s care plan is tailored to their needs. When it comes to head and neck cancers, a team of expert specialists form an interdisciplinary care team that supports the patient and their family through the whole treatment process.
In Wellstar STAT Clinics—short for Specialty Teams and Treatments—patients can see multiple cancer specialists to be diagnosed, have questions answered and finalize a treatment plan in a single day at one location. This reduces the need to drive to different locations and helps the patient start treatment faster.
“The concept of multidisciplinary care is tried and true and shown to be effective for cancer patients,” said Dr. Fiyin Sokoya, a Wellstar head and neck cancer surgeon. “This model decreases the time to proceed with and receive care.”
First, a team of medical experts, including a head and neck cancer surgeon and facial plastic surgeon, a radiation oncologist, a medical oncologist, a pathologist and a neuroradiologist, review the patient’s pathology and imaging as a group to diagnose, stage and create a personalized treatment plan.
Next, the patient and their family meet with the experts. This is an opportunity for the patient to learn about the recommended treatments and ask questions.
“Traditionally, patients must drive to several different appointments to learn the stage of their cancer, meet with different specialists and make decisions,” said Wellstar Medical Oncologist Dr. Nagender Mankan. “At that point, four to five weeks have gone by. In STAT Clinics, we are expediting the complicated decision-making process.”
The patient also meets with a nurse navigator. This specialized nurse helps coordinate many aspects of care for the patient including scheduling appointments and connecting patients with support team members, such as a registered dietitian, a speech therapist or a dentist who may help relieve irritation in the mouth and throat.
While Wellstar is well-equipped to help you fight head and neck cancers, there are steps you can take to prevent cancer from forming, including limiting exposure to the sun and cutting out tobacco and alcohol. Your Wellstar care team can work with you on a plan to keep your head and neck healthy and set achievable goals to prevent cancer.

Wellstar Family Medicine in Morrow is Relocating
Wellstar Family Medicine in Morrow is relocating to Douglasville.
Starting April 29, you can find us at:
Wellstar GME Family Medicine - Douglasville
6002 Professional Parkway, Suite 220
Douglasville, GA 30134
(770) 968-6464
We appreciate the opportunity to serve as your healthcare partners, and we hope you will continue your care with us in our new location.
Our last day in Morrow is April 19. If you have an appointment between April 22 and April 26, we will contact you to reschedule. Patient appointments scheduled for April 29 or later will take place in Douglasville.
We are committed to helping you find a location that is both convenient and the right fit for your health needs. Call us at (770) 956-STAR (7827) if you would like assistance in finding a new provider. Several options for continuing care in the Morrow area are:
1. The Family Health Centers of Georgia will begin operating from our current Morrow location (1000 Corporate Center Drive, Suite 200) in early May. They are a Federally Qualified Health Center that provides primary care, family planning and other specialized health programs—regardless of ability to pay. They will move to their newly renovated space nearby at 6685 Merchants Way in July 2024. Learn more about FQHCs.
2. CenterWell Senior Primary Care 1821 Mount Zion Road, Morrow, GA 30260 (470) 491-2020
3. Mayuga Family Medicine 236 Stockbridge Road Suite B, Jonesboro, GA 30236 (770) 742-9326
4. Wellstar Primary Care 3890 Redwine Road Suite 100, Atlanta, GA 30331 (404) 344-0059
5. Wellstar GME Internal Medicine Clinic 747 South 8th St. Suite B, Griffin, GA 30224 (470) 604-8250
6. Wellstar Primary Care 708 S. 8th St., Griffin, GA 30224 (770) 228-5402

Make Health Your Habit This Spring
When the weather starts to warm up, many people start getting ready for the spring season. Along with cleaning and decluttering your home, you should also spruce up the space you live in every day—your body.
When you prioritize your well-being and do the proper up-keep for your health, it may help you stay ahead of potential medical issues.
To feel your best this spring and beyond, we’re sharing our top tips to keep you healthy.
Check for a clean bill of health
Setting our clocks forward can also be your reminder to set up a visit with your primary care provider.
“People should definitely add a wellness exam to their spring-cleaning checklist, regardless of age. Routine preventative care every year is very important,” said Wellstar Primary Care Physician Dr. Nayab Dhanani.
During a wellness exam, your provider will check your Foundational 4 numbers—body mass index (BMI), blood pressure, blood sugar and cholesterol levels.
From there, your provider can help create a screening plan to help keep you ahead of chronic conditions or serious diseases. Recommended screenings may vary depending on your family history, gender and age, as well as your provider's recommendations.
“The importance of screenings is really to be proactive instead of reactive,” said Wellstar Primary Care Physician Dr. Facia Dew. “It’s better to know a person’s risk factors so we can screen accordingly. Our goal is to meet their unique medical needs and help them live a healthy life.”
Be sure to bring up any other medical concerns, health questions or wellness goals at the appointment. Wellstar providers are partners in your care, committed to keeping you feeling your best physically, mentally and emotionally.
Stay ahead of health concerns
It can be easy to put your own health on the backburner as life gets busy. This spring, make a commitment to yourself to get the essential screenings you need.
For women, screenings like pelvic exams, Pap smears and mammograms can help catch cancer, sexually transmitted diseases and other issues. These important physical and gynecological health exams can help you stay ahead of potential medical concerns, such as breast cancer, cervical cancer and ovarian cancer.
Along with a routine physical to stay in top shape, men can benefit from a prostate-specific antigen test. Having this simple blood test done can help catch prostate cancer in its early stages, often when it is more treatable. Men who are 50 or older should start getting screened for prostate cancer. Those at higher risk—including Black men and those who have had a close relative diagnosed with prostate cancer—may start screenings even sooner.
Talking about colon health can feel a little uncomfortable, but getting screened could save your life. Starting at age 45, everyone should get a colonoscopy. Those with a higher risk or family history of colorectal cancer may need to start screening even sooner. Learn more about the importance of colon screenings.
Freshen up your mindset
For people who experience seasonal depression during the fall and winter months, spring’s longer hours of light may bring a renewed sense of hope. Still, lingering feelings of sadness or other difficult emotions could be more than just the “winter blues.”
“We have a screening test called PHQ-2, which is used to screen for depression,” Dr. Dhanani explained. “Patients typically have to answer two questions, and it is a preliminary screening to see if you have any signs or symptoms of depression.”
“Plenty of times, patients don’t even know they have depression. Often, a person may have had the condition for a while and it could be untreated,” Dr. Dhanani said.
If you feel overwhelmed and need support, we’re here for you. Reach out to your provider or one of our behavioral health specialists for help.
Looking for more ways to stay well? Learn about screenings to help keep you healthy.

CJCare
Former former major league baseball player CJ Stewart didn’t want to have a colonoscopy. He dreaded the liquid diet. The needles. The IV sedation. The possibility of cancer.
So how did CJ face his fears—and what happened next?
It started in 2020 when CJ scouted a new primary care provider. He chose Dr. Randy Hines II, Wellstar Primary Care. He said Dr. Hines was the most straightforward doctor he had ever visited.
“I was overweight,” CJ remembered. “My health changed positively because Dr. Hines said things to me in a very positive way. He was direct with me and that helped save my life.”
Dr. Hines learned CJ’s father was a diabetic and had quadruple bypass heart surgery to treat a heart attack. CJ remembered him saying, “‘You’re on track to have the same thing but you can control it.’”
CJ admitted that he had a daily dose of French fries and two peanut butter and jelly sandwiches before bed. Dr. Hines challenged him to rethink his relationship with food if he wanted to see his daughters walk down the aisle one day. It was tough talk and it meant something.
“I really love my daughters!” CJ said. “It made me change.”
As a result, he modified his diet, took up running and lost 45 pounds.

Then CJ’s mom revealed a family history of colon cancer.
“My wife and daughters were like, ‘We really need you to go get checked to make sure you’re good,’” he said.
Because of his fears related to the colonoscopy, CJ wanted to have Cologuard, an at-home screening test for colon cancer. But Dr. Hines recommended the 47-year-old have a preventive colonoscopy screening instead, explaining that if pre-cancerous polyps are detected during the procedure, they can be removed before becoming cancerous.
“I didn’t want to hear it,” CJ laughed. “But hearing that from a fellow African American man, I trusted that it was the right thing to do.”

Expert Treatment for Head and Neck Cancers at Wellstar
Head and neck cancers include several different types of malignant tumors affecting parts of the head and neck, including the nose and sinus cavities, mouth, throat, voice box and salivary glands. Head and neck cancers typically involve the mucosa, or the tissues lining these areas, and represent about 4% of all cancers diagnosed in the United States each year.
If you are diagnosed with cancer, Wellstar provides expert care. Oropharyngeal cancers are typically treated with surgery (with or without radiation therapy) or radiation therapy (with or without chemotherapy) at equivalent cure rates. Goals of treatment are to remove the cancer, prevent its return and limit side effects.
“Wellstar providers work with patients to tailor care to their needs—based on effectiveness of the treatment, tumor location and stage, accessibility of the tumor to a surgical approach, risk of side effects and patient choice,” said Dr. Kia Jones, a Wellstar ear nose & throat physician.
In the Head and Neck STAT Clinics at Wellstar Cobb, Douglas and North Fulton Medical Centers, the patient meets with their entire treatment team in a single day during treatment planning and may start treatment sooner, which may improve outcomes for patients and provides more peace of mind.
Transoral robotic surgery, offered at Wellstar North Fulton, has changed the way oropharyngeal cancers are treated surgically.
“In this procedure, the surgeon accesses the cancer by passing tools through the mouth rather than making an incision,” said Dr. Jones, who performs the procedure.
For those patients with early-stage tumors and limited disease in the neck, the surgery offers the patient a cure at a single intervention without the need for tracheostomy or abdominal feeding tube, faster return to taking food orally, improved outcomes and faster recovery. This is preferred over traditional surgical methods, which require splitting the jaw and/or the tongue or gaining access to the throat via neck incision.
You can take action against common risk factors by decreasing tobacco and alcohol use and getting the human papillomavirus (HPV) vaccine.
Some well-known risk factors for the development of head and neck cancers include heavy alcohol and tobacco use, especially if someone uses alcohol and tobacco together. Men are three times more likely to be diagnosed with oral and throat cancer compared to women, according to the American Cancer Society.
An additional risk factor is HPV infection, which is related to the development of oropharyngeal cancer specifically. The oropharynx is the midsection of the throat and includes the tonsils and the root of the tongue or tongue base where the vast majority of these tumors originate. HPV-related oropharyngeal cancer is more prevalent now than HPV-related cervical cancer in women. HPV-related oropharyngeal cancer has been increasing in the United States over the last three to four decades, while the incidence of tobacco and alcohol-related tumors has been declining. More than 22,500 people are diagnosed with HPV-related oropharyngeal cancer each year.
Learn more about how Wellstar cares for head and neck cancers.

Advancements in orthopedic care
Republished Content: Atlanta Business Chronicle
This article was originally published on Atlanta Business Chronicle on April 12, 2024.
Orthopedic care has evolved from injury treatment and corrective surgery into a critical component of modern healthcare. As primary care remains foundational in managing overall health, the demand for orthopedic services has surged, reflecting changing lifestyles, demographics and expectations. In any given year, 12% to 14% of the adult population will visit their physician for back pain, according to the United States Bone and Joint Initiative (USBJI).
Against this backdrop of widespread musculoskeletal issues, Wellstar recently convened with the Atlanta Business Chronicle for a panel discussion to delve into the changing landscape of orthopedic care. This insightful forum explored key trends, challenges and innovations shaping the field, with leading healthcare professionals offering valuable perspectives. These discussions unraveled the complexities of orthopedic care, ranging from preventive strategies to cutting-edge treatments. Among the panelists was Steve Quehl, a former college football player for Notre Dame, who started as a tight end before transitioning to a center. Other panelists were Dr. Hodari Brooks, orthopedic surgeon, Wellstar Health System; Dr. Joseph Burns, chief musculoskeletal officer, Wellstar Health System; Dr. Timothy Oswald, pediatric orthopedic surgeon, Wellstar Pediatric Orthopedics. Moderator was David Rubinger, market president and publisher, Atlanta Business Chronicle.
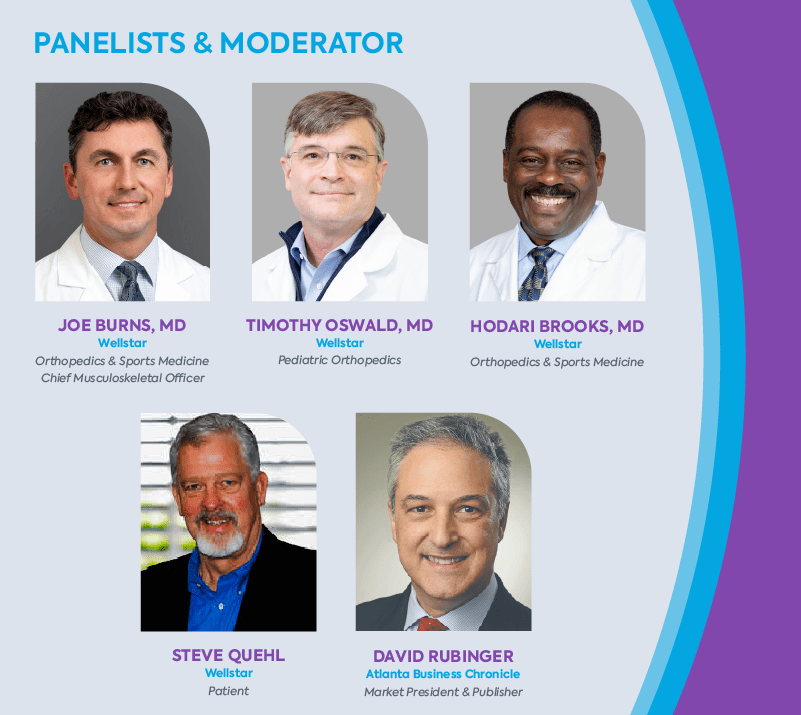
David Rubinger: There’s an uptick in the demand for orthopedic services and these specialists have become increasingly essential to healthcare. What societal changes drive this heightened need for specialized ortho care?
Dr. Joseph Burns: We’re facing an aging population alongside a growing desire for an active, pain-free lifestyle. In the past, individuals had to endure their limitations and pain for life. Today, people have more options. Technology, techniques and training advancements now provide surgical alternatives that significantly enhance quality of life well beyond middle age.
Wellstar conducts numerous community campaigns through various channels, including community events, the media and in our offices and hospitals, highlighting the value of maintaining health and establishing a relationship with a primary care physician.
Dr. Hodari Brooks: Societal changes for both our youth as well as adults have resulted in the increased need for orthopedic care. Physical activity has decreased, with fewer kids participating in physical education. This leads to more injuries related to obesity and lack of activity. The need for joint replacements is soaring, driven by both baby boomers aging and younger individuals seeking treatment earlier. Half of my practice is caring for patients under 55, a shift from when people would wait years for treatment. Now, we prioritize improving quality of life sooner rather than later.
Patients, including those seeking joint replacements, are opting for earlier interventions. They are less inclined to wait for treatment, indicating a shift within the healthcare system towards promptly addressing patient needs.
Rubinger: What new injury trends are emerging in sports due to changing physical activity patterns, especially with the rise of extreme sports and diverse workout routines?
Dr. Burns: The rise in overuse injuries among our younger population is disheartening. Young athletes don’t diversify their sports as they once did, leading to year-round specialization and an increased risk of injury. This relentless pursuit of success often comes at the cost of rest and diversity in physical activities.
We’re also encountering complex medical issues that require specialized treatment, reflecting both advancements in medical care and the aging population’s evolving healthcare needs. Conditions once considered untreatable are now within our reach, marking a significant shift in the scope of orthopedic care over the years.
Rubinger: Dr. Oswald, as a pediatric orthopedic specialist, have you frequently observed the concept of subspecialization and the decline in diversification among young athletes?
Dr. Timothy Oswald: It’s a significant area of concern for us, and we’re conducting more research. Recent studies have highlighted the insufficient breaks and rest periods given to children, as well as the trend of starting high-level athletics too young, which aligns with the issue of subspecialization. Kids are not miniature adults. Their orthopedic stresses differ due to growth plates and differing stress responses.
We’re educating the community, including coaches and parents, about the importance of rest periods during training through channels like social media. We aim to implement better training methods so young athletes can continue playing into their college years, as we’re noticing a concerning trend where many high-level athletes quit sports as early as eighth grade.
Rubinger: Steve, as a former college athlete yourself, what’s your observation of the sports world’s changes regarding how injuries are approached, especially compared to when we were younger?
Steve Quehl: I view this issue through the lens of my grandchildren and their friends, and I agree with the insights shared by these doctors. Their perspectives must influence parents’ decisions, particularly regarding the early specialization trend. Parents often have unrealistic expectations of their children becoming professional athletes, which can lead to overtraining and injuries. Kids should have a balanced approach to sports. I’m grateful my daughters chose activities like swimming over contact sports for their children, considering the risks to growing bones and muscles.
Prior to my enrollment at Notre Dame, I appreciated the joy of playing multiple sports during each season for fun, without the pressure of turning it into a professional pursuit.
Rubinger: I’ve noticed remarkable changes in my lifetime regarding the duration of procedures and the efficiency of hospital stays or visits to outpatient surgery centers. I’m curious about your perspective on this shift away from extended hospital stays. Do you believe it’s ultimately beneficial or detrimental to patients? What are your thoughts on this evolution of the time spent in hospitals or surgery centers?
Dr. Brooks: There’s been a significant shift in the duration of hospital stays, especially concerning joint procedures. In the past, patients would typically spend several days in the hospital before and after surgery. In my practice, around 90% of primary joint patients can return home the same day, which is remarkable. This change is not only due to patient preferences for quicker recovery but also has medical benefits, such as reducing the risk of infection. Outpatient joint replacement is not done everywhere, however, and it is important to discuss this option with your individual surgeon.
Insurance companies have started incentivizing shorter hospital stays. While this trend has clear advantages, it also comes with challenges, such as pressure to discharge patients quickly. The ability to expedite recovery and minimize specific complications is a positive development I believe will continue.
Rubinger: Do we have data showing a decrease in complications due to the trend of shorter hospital stays, particularly for joint procedures?
Dr. Burns: Evidence indicates improved outcomes for outpatient procedures, with data supporting this trend. The shift involves a comprehensive approach beyond simply performing the surgery and discharging the patient. It requires a multidisciplinary effort, with investments in establishing preoperative optimization programs, patient education classes and a coordinated team approach on the day of surgery.
Patients undergo physical therapy before returning home, but the care doesn’t stop there. We must ensure effective pain management, minimize infection risks and create a safe home environment to support their recovery. This process goes beyond safely discharging patients. It’s about ensuring their complete and safe recovery. I’m proud of the extensive teamwork and complex processes that Wellstar has implemented to support these programs.
Quehl: When it was time to correct my right shoulder this past year, I went in the morning and came back home in the evening. Dr. Burns assured me that I’d be home the same day, and it was a wonderful experience. I didn’t want any overnight stays. It was well-planned and executed, with proper anticipation and expectations set. The follow-up was excellent, too.
Dr. Brooks: Patients are shocked or hesitant when I inform them that they’ll go home the same day. It’s about managing expectations and explaining the benefits, especially as it relates to improved outcomes. Involvement in these programs gives physicians more control over the process. It’s a serious undertaking but rewarding because we can provide more input, especially in an outpatient setting. Collaboration with anesthesia colleagues has improved, particularly with techniques like regional blocks, as patients need to be up and about after surgery. Almost universally in my experience, patients prefer their outpatient surgical experience to any previous hospital stays.
Rubinger: This leads me to my next question regarding opioids and pharmacology. Has pharmacology evolved over the last decade to improve patient treatment?
Dr. Burns: Most of us are employing what we refer to as multimodal pain control, which involves a process aimed at sparing, if not entirely eliminating, the need for opioids as a primary method of pain management. By utilizing different medications that target distinct pain receptors, we can effectively manage pain while minimizing potential side effects that may arise from relying solely on opioids or multiple doses of the same medication. Advancements in regional blocks, administered by anesthesiologists, allow injections that can provide numbing effects in the affected areas for several days, alleviating initial post-operative pain and reducing patients’ overall need for pain medication over time.
Dr. Oswald: The opioid crisis in the greater Atlanta area is a significant concern for both children and adults, and it’s something we’re all acutely aware of. We’ve initiated extensive research efforts at Wellstar to address this issue and lead advancements in pain management that don’t rely on narcotics. Similar to the approach described in the total joint experience, we’ve been observing this trend for some time now, even in pediatric cases.
When I trained for pediatric spine surgery 20 years ago, patients stayed in the hospital for at least a week post-surgery. By implementing multimodal approaches, we’ve managed to reduce narcotic use by nearly 90% while also transitioning from a week-long hospital stay to just a 23-hour observation period for certain procedures.
Patient satisfaction is higher with these approaches, directly correlating with their overall experience. Are we expediting discharge solely for the sake of pushing people out? Actually, no. It’s about ensuring patients feel empowered in their recovery process, with their pain managed effectively, and their ability to return to the quality of life they desire. These patient-centered care programs optimize outcomes and enhance the overall healthcare experience.

Feeling ‘Backed Up’? Your Provider Can Help You Fix Constipation
Constipation can be defined as a change in frequency of stool, consistency of stool or both. Normal frequency of bowel movements is thought to be anywhere between three times a day to three times a week. Additionally, having very hard or pellet-like stools is an indication of constipation.
Constipation can be caused by a variety of things, including dietary changes (like decreased water or fiber intake), thyroid issues, slow gut motility, electrolyte imbalances, medication changes and sometimes even more serious medical disorders such as cancer.
“It is important to talk to your provider if you’re experiencing an issue with constipation,” said Wellstar Gastroenterologist Dr. Shani Clay. “There are specific laboratory studies and even imaging that can be done to further evaluate abnormal stools. If you're noticing blood in your stool or unexplained weight loss, a colonoscopy may even be warranted to rule out a more serious condition.”
Wellstar gastroenterologists can help you determine the cause of your constipation.
If you are feeling a little “backed up,” there are also a few things you can do to help you have more regular bowel movements. Ensuring you are drinking at least 64 ounces of water daily helps to soften your stool so that it can pass more easily out of the colon. Further, it is important you follow a diet high in fiber. This includes eating things like raspberries, pears, apples with skin, green peas, broccoli, whole wheat spaghetti, oatmeal and black beans. If dietary changes do not work, there are a variety of both over-the-counter and prescribed medications that your provider may recommend to help get you going.
Constipation occurs quite frequently in the general population and may warrant further work-up. Increasing water intake and modifying your diet to include more fiber may help, but it is important that your symptoms are conveyed to your provider in case additional testing needs to be done. Staying regular helps you to feel better, both physically and mentally. Gut health is important, so make sure you are keeping it clean!
Learn more about how you can start healthy habits to benefit your digestive wellness.

Wellstar Recognized as a Top Employer Nationwide
Wellstar Earns Top Hospital Recognition for Community Investment
A new Fair Share Spending Report from the Lown Institute, an independent healthcare think tank, listed Wellstar’s hospitals among the top in the nation for financial assistance and community investment. The recognition is based on what the Institute estimates Wellstar’s invested in the community compared to its 2021 tax exemption, resulting in what the Institute calls a “fair share” surplus. According to the Institute, only 20 percent of nonprofit hospitals nationwide were recognized for their fair share surplus.
Lown calculated Fair Share Spending by comparing the estimated value of private, nonprofit hospitals’ tax exemptions to the amount spent on financial assistance and meaningful community investment—including community health improvement activities, cash and in-kind contributions to community groups, community building activities, and subsidized health services.
This report follows a recent recognition from Modern Healthcare noting that Wellstar provides the second-highest percentage of charity care among large nonprofit U.S. health systems. According to Modern Healthcare, Wellstar devoted 6.11% of its operating expenses in fiscal year 2022 to charity care.

Wellstar MCG Health Celebrates Progress on Wellstar Columbia County Hospital with Ceremonial Groundbreaking
With a mound of red dirt piled behind him and wearing a hard hat, Gov. Brian P. Kemp lifted a purple-bowed shovel full of gray dirt Monday, April 1, ceremonially breaking ground on Wellstar Columbia County Medical Center.
Joining him in this symbolic event were First Lady of Georgia Marty Kemp; Candice L. Saunders, president and CEO of Wellstar Health System; University System of Georgia Chancellor Sonny Perdue; Ralph Turner, president of Wellstar MCG Health Medical Center; Brooks A. Keel, president of Augusta University; Doug Duncan, chairman of the Columbia County Board of Commissioners; and other esteemed dignitaries to commemorate construction of the new hospital and medical office building.
They were among the first to sign a purple beam with a Wellstar logo commemorating the momentous event. The 8-foot-long ceremonial beam will next travel to the Wellstar MCG Health campus so team members who provided input on the facility’s design can also sign it.
“Today’s groundbreaking is a great symbol of the incredible partnership between the state, local and private sector leaders and what is being done every day to expand access to quality, affordable healthcare to Georgians throughout the state,” said Gov. Kemp. “Through this partnership, Columbia County and the surrounding rural area will be able to experience innovative care, and the state will benefit from the generations of new minds that will be molded to provide care in the years to come.”
When Wellstar Columbia County Medical Center and the adjacent medical office building open in 2026, the full-service acute care hospital will feature 100 inpatient beds; an emergency department expected to become a Level II trauma center; a surgical platform that will include operating rooms, catheterization laboratories, and interventional radiology and endoscopy; and a 90,000-square-foot medical office building that will offer primary care, women’s health care and other specialties.
Wellstar Columbia County Medical Center will bring the world-class care already provided at Wellstar MCG Health to the residents of Columbia County and the surrounding areas. The new hospital’s close proximity to I-20 will make accessing that care more convenient and will create more jobs for the community.
“I can’t stress enough how important this partnership is to the people of Columbia County as well as the state of Georgia,” said Perdue. “This facility will expand access to quality healthcare, create more opportunities for students and prove to be a huge turning point in medical provision in Georgia.”
Wellstar is a nonprofit community health system that works to ensure every person has access to personalized, high-quality healthcare. The 11-hospital health system has a deep and long-standing dedication to providing care for diverse communities, those in need and underserved Georgians.
“At Wellstar MCG Health, our mission is to enhance the health and well-being of every person we serve,” Turner said. “We look forward to continuing to work with our community partners in ensuring the patients and the community we serve have the best care possible.”
Wellstar has committed to invest more than $800 million in capital expansion across Richmond and Columbia counties. Wellstar Columbia County Medical Center will complement and expand the world-class resources that are already provided at Wellstar MCG Health.

Wellstar MCG Health Appoints President
Ralph Turner has been appointed senior vice president and hospital president at Wellstar MCG Health Medical Center. Prior to his time serving in the role on an interim basis, he served as SVP and president for Wellstar Paulding Medical Center since 2022.
“Ralph has enthusiastically welcomed MCG Health team members into the Wellstar family. He’s doing an extraordinary job leading the integration of our people, processes and technologies into a culture that honors every voice and celebrates academic and clinical excellence,” said Mary Chatman, PhD, RN, Wellstar executive vice president of acute care operations.
Turner has held leadership roles at large, complex healthcare organizations, including MedStar Washington Hospital Center, University of Wisconsin Hospital and Clinics, and Cleveland Clinic. Turner received his doctorate in business administration from the University of Wisconsin-Whitewater and master’s degrees in healthcare administration and public administration from the University of Maryland and Troy University at Dothan, respectively. He served for more than 21 years in the U.S. Army before launching his healthcare career at Walter Reed Army Medical Center as director of the Clinical Engineering Division.
Wellstar MCG Health includes the 478-bed adult hospital, the 154-bed Children’s Hospital of Georgia, the Georgia Cancer Center and more than 80 outpatient clinics across Georgia and South Carolina. The organization partners with Augusta University’s Medical College of Georgia and offers an industry-leading cancer care and telestroke network, the region’s only Level I Trauma Center and the only Level IV Neonatal Intensive Care Unit for critically ill infants with an air transportation team.
Serving as the regional coordinating hospital for Georgia’s East Central District, Wellstar MCG Health responds to statewide natural disasters and events impacting the health of Georgians everywhere.
Wellstar Kennestone Regional Medical Center Appoints New President
Wellstar Health System has hired Lorrie Liang to be senior vice president and hospital president of Wellstar Kennestone Regional Medical Center and Wellstar Windy Hill.
“Lorrie is well poised to lead the complexities of Wellstar Kennestone and Wellstar Windy Hill,” said Mary Chatman, PhD, RN, executive vice president of acute care operations and former president of Wellstar Kennestone. “She will be accountable for leading Kennestone's executive team, collaborating with the other Wellstar markets, partnering with our physician enterprise and engaging with key community stakeholders to further the outstanding work and successes we’ve seen at both hospitals in recent years.”
With a background in running large, complex organizations, Liang brings more than 25 years of experience in hospital operations, service lines, physician practices, graduate medical education and research in academic and community hospitals and healthcare systems.
Liang is currently the president of Sarasota Memorial Hospital, which includes 900 beds, 6,400 employees, 1,300 medical staff, a Level II Trauma Center, a Comprehensive Stroke Center, a 60-bed inpatient rehabilitation hospital, an 82-bed behavioral health inpatient and outpatient facility, a 56-bed dedicated oncology tower, a 120-bed skilled nursing facility and a free-standing ER in southwest Florida.
She holds a Master of Health Services Administration degree from The George Washington University School of Business and an undergraduate degree from the University of Maryland Baltimore County.
Wellstar Kennestone Regional Medical Center is a 633-bed hospital located in Marietta, which offers best-in-class multidisciplinary care: state-of-the-art cardiac program, collaborative vascular program, renowned Women’s Center, Level III Neonatal Intensive Care Unit, multidisciplinary STAT cancer treatment and more. Wellstar Kennestone operates the second busiest emergency department (ED) in Georgia and the second largest ED in the U.S. with the capacity to care for more than 220,000 patients annually.
Wellstar Windy Hill is a Total Joint Center of Excellence where experts tailor orthopedic care and provide comprehensive outpatient rehab services and pediatric services. Windy Hill’s Long-Term Acute Care unit is staffed by specialized critical care physicians and specialized nurses who provide care in all-private rooms.

Transforming Healthcare Through Tech at SXSW
Catalyst by Wellstar led this year’s South by Southwest Conference (SXSW) with conversations on how investing in women in the tech space will have rippling effects on our healthcare ecosystem and how it all comes together to transform the patient experience.
From announcing an investment in Betty’s Co., a startup that provides in-person and virtual services in gynecology, behavioral health and wellness with a multi-faceted approach to healthcare for Gen Z women, to working with Gabbi, a startup on a mission to eradicate late-stage breast cancer, and Marani Health, an AI-powered maternal healthcare platform and direct investment announced in 2023, Catalyst has shown its commitment to fostering connections that drive access and clinical growth. These leaders shared the journeys that drove them to build their companies and exemplified the significance of having heart drive innovation.
Jaimie Clark, head of innovation at Catalyst by Wellstar and the director of innovation and venture strategy for Wellstar Health System, spearheaded the panel in an open conversation on how to best meet women's needs today and in the future. "This investment reflects Catalyst's commitment to caring for the women in our communities and beyond, providing them with innovative tools to access healthcare sooner and boosting the next generation of companies in this space," Jaimie said.
Nick Peddy, chief technology officer at CLEAR, and Dr. Hank Capps, chief information and digital officer of Wellstar Health System and president of Catalyst by Wellstar, joined a discussion moderated by Stephen Konya, a senior advisor to the deputy national coordinator for health IT and innovation portfolio lead at the U.S. Department of Health and Human Services (HHS). They shared their vision of transforming the patient experience within healthcare by utilizing cutting-edge technology and insights to make the process more efficient, secure and patient-friendly.
The panels at SXSW discussed how ingenuity can blend with an ecosystem of collaboration to harness and reshape the status quo of an industry. The panels at the conference shared insightful dialogue on raising the bar of healthcare for the next generation. Diagnosed as infertile at the age of 17, Betty's Co. founder and CEO Jennifer Newell experienced firsthand the unique healthcare needs of younger women, and she shares how often the current approach to healthcare for this population lacks in genuinely reaching them. Jennifer shared her powerful story and mission of "creating spaces where every Gen Z woman feels comfortable getting the care they need."

Make Digestive Health Your Habit
Your digestive system works hard to keep you healthy—be proactive about protecting it!
“Your digestive system plays an essential role in your well-being, helping your body absorb nutrients and provide energy and fuel for your favorite activities,” explained Wellstar Gastroenterologist Dr. Arif Aziz.
That’s why it’s so important to do your part to protect your gut health.
Wellstar providers help your digestive system stay on track, so you can feel your best and keep doing the things you enjoy most.
Your digestive system is made of an entire team of organs: the esophagus, stomach, intestines (small and large), pancreas, liver, gallbladder, rectum and anus.
“With so many parts working together, your digestive system requires expert care to stay well,” said Wellstar Gastroenterologist Dr. Inder Tandon. “Regular check-ups with your Wellstar provider can help identify potential digestive issues early.”
At a routine exam, your primary care provider can screen for serious diseases like colorectal cancer and help identify chronic and common digestive conditions.
“If specialized care is needed, your primary care physician can refer you to our expert team of gastroenterologists right away,” Dr. Tandon shared.
Wellstar gastroenterologists offer a full range of services to diagnose, treat and manage both common and complex disorders, including constipation, diarrhea, irritable bowel syndrome (IBS), Crohn’s disease and gastroesophageal reflux disease (GERD).
At Wellstar, we understand digestive issues can disrupt your everyday life—and talking about them can be tough.
Wellstar Gastroenterologist Dr. Cameron Body addressed this issue, encouraging patients to be honest about their health.
“Many people may feel uncomfortable discussing digestive issues, but it’s important to speak up and have an open dialogue with your provider,” Dr. Body said. “Wellstar has a team of specialists to help treat your symptoms and keep you feeling well.”
See how our gastroenterologists care for you.
Inside the digestive system, most colorectal cancer starts as a growth, or polyp, in the colon or rectum. Because polyps develop slowly over time, you may experience few warning signs and not know you have a medical issue for months or even years.
That’s why it’s so important to get a colonoscopy—it could save your life. When caught early before it spreads, colorectal cancer has a 91% five-year relative survival rate, according to the American Cancer Society. The relative survival rate compares people with the same type and stage of cancer to the general population.
People with average risk should have a colonoscopy starting at age 45. Those at high risk or with a family history of colon cancer may start screenings even sooner. Talk to your provider about your screening plan.

Let’s Get to the Bottom of Your Colonoscopy Questions
In people under 50, colorectal cancer is now the number one cancer-related killer of men and the number two killer of women. Black communities are 20% more likely to get colorectal cancer and 40% more likely to die from it. But this doesn’t have to be the case—colorectal cancer is preventable. When people have a screening colonoscopy, doctors can remove pre-cancerous polyps, stopping them from ever becoming cancer.
Colonoscopies are now recommended starting at age 45 for the general population, and younger for people at higher risk or with a family history. But you have questions:
I’m above average healthy—do I really need a colonoscopy?
How do I know my risk level?
Will the procedure be painful?
How much time should I take off of work?
A panel of gastrointestinal health experts and a patient answer your questions and more here.

Who needs a colonoscopy
I eat well, exercise and am in good general health. Do I really need to go through the hassle of a screening colonoscopy?
Dr. Shani Clay, gastroenterologist: Unfortunately, we discover colon cancer in quite healthy individuals. While it is true that smoking and consumption of red meat increases your risk, we also see colorectal cancer in patients who follow very healthy diets and exercise regularly, hence the need for all people to get screened for colon cancer.
Samantha McInturff, colon cancer survivor: The screening age used to be 50 before they changed it to 45, so I had never had a screening. I was 48 when I had symptoms that led to a colonoscopy and I was diagnosed with stage 4 colon cancer. I am a rule follower. I always get my mammograms. I never smoked. I have no family history. I thought, ‘How can I have cancer?’ What I’ve been through really highlights the importance of screening early. Don’t be scared. Getting screened for colon cancer is a small inconvenience that’s completely worth it.
When should I start having colon cancer screenings and how often will I need to have one?
Dr. Clay: For people at average risk, meaning people with no alarm symptoms and no family history of colon cancer, screening begins at age 45.
How frequently you should have a colonoscopy depends on a few things, including family history, the number and type of polyps that are found during your colonoscopy and how clean the colon is at the time of the procedure. Repeat procedures can be anywhere from six months up to 10 years, depending on the results.
Colon cancer is in my family. When should I start screening?
Dr. Sahir Shroff, surgical oncologist: We’re seeing more and more young patients with colon cancer. If a patient has a strong family history, the screening should start sooner than 45 years of age. For example, if your parent died of colon cancer, you should begin colonoscopies at the age of 30. It depends on the risk factor. Talk to your primary care doctor about your personal risk level.
Dr. Clay: If you have high-risk factors, you should be screened earlier. For example, if a person has a first-degree relative with colon cancer who was diagnosed at less than 60 years of age, that individual should get a screening colonoscopy at either 40 years of age or 10 years younger than the age at the relative’s diagnosis. Additionally, there are certain genetic syndromes that also warrant earlier colon cancer screening with a colonoscopy at less than 45 years of age. Wellstar has a Genetic Risk Assessment Program for people with hereditary risk factors or a family history of cancer.
Should I see a doctor if my stool looks different than before?
Nancy Page, oncology nurse navigator: If you’re having changes in your bowel habits like blood in or on your stool or black stool, you need to let your doctor know soon. Consistent changes like constipation, diarrhea and, it may sound gross, but skinny stools that look like a pencil for a few weeks or more are signs to talk to your doctor. Other changes to be aware of are unexplained weight loss, unexplained fatigue, abdominal pain and even anemia. Don’t put it off. Don’t think, ‘I work a lot. I have kids. I’m busy.’ Let your doctor know now. If it’s colon cancer and it’s diagnosed early, there’s a 90% cure rate.

Keep Your Head & Neck in Check
Take charge of your head and neck health. Talk to your care team about how you can stay ahead of serious concerns before they start.
Most head and neck cancers—including oral, throat and thyroid cancers—begin in the mouth or throat.
Here are a few steps you can take to keep your head and neck in top shape, so you can live your healthiest life.
Tobacco use, including smoking and the use of smokeless tobacco such as chewing tobacco or snuff, is a major risk factor for head and neck cancers. The use of alcohol and tobacco together can be especially risky.
Inhaling anything other than a prescribed medicine, including the use of e-cigarettes and marijuana, could increase the risk as well, according to Dr. Timothy Ryan, a Wellstar ear, nose & throat physician.
“Abstinence from smoking any substance is always the best answer when it comes to your head and neck health,” Dr. Ryan said.
Ultraviolet light, such as exposure to the sun or artificial UV rays like tanning beds, is a major cause of cancer on the lips and scalp. Protect your lips by using a lip balm with sunscreen, and make sure to wear sunscreen on your face and neck when you go outside, even in colder weather. Protect your head from sun exposure with a hat.
According to Dr. Ryan, human papillomavirus, or HPV, is one of the main risk factors for head and neck cancers.
“There are two main risk factors for head and neck cancers that we see most commonly. One is from smoking,” he said. “That can be made worse from alcohol use. The other is actually a virus, and it’s a really well-known virus, human papillomavirus.”
About 70% of cancers in the oropharynx (which includes the tonsils, soft palate and base of the tongue) are connected to HPV, according to the Centers for Disease Control and Prevention.
HPV is the most common sexually transmitted infection. Talk to your provider about HPV prevention and exposure, and seek treatment if you are showing signs of HPV. Although many people with HPV don’t have symptoms, some develop warts in the genital area.
Gardasil-9, the vaccination against HPV, protects patients against the types of HPV that cause most HPV cancers. Patients from age 11 to 46 should consider vaccination after speaking with their clinician.
Some jobs can also be risk factors. The construction, textile, ceramic, logging and food processing industries can cause exposure to substances like wood dust, formaldehyde, asbestos, nickel and other chemicals. These increase the risk of cancer in the nasopharynx, or the top part of the throat.
And if you have been infected with the Epstein-Barr virus, which causes mononucleosis and some other illnesses, you could be at higher risk. Previous radiation treatments to the head and neck can also increase your risk.
“Talk to your healthcare provider about your health history so they can help you evaluate your risk,” said Dr. Fiyin Sokoya, a Wellstar head and neck cancers surgeon. “They can help you take action and prevent cancer.”
Symptoms of head and neck cancers will vary based on which part of the head and neck they appear. Signs include:
While it’s important that everyone look for symptoms of head and neck cancers, these conditions are more likely to affect men. Men are three times more likely to be diagnosed with oral and throat cancer compared to women, according to the American Cancer Society.
If you are showing any symptoms of head and neck cancers, contact your healthcare team.
“Annual dental and oral examination by your dentist is the best way to screen for head and neck cancers,” Dr. Sokoya said.
Learn more about how Wellstar cares for head and neck cancers.

Wellstar Team Members Voted Best of Cobb in 2024
The care teams at Wellstar are dedicated to enhancing the health and well-being of everyone we serve, and we thank our team members for their commitment to world-class care. We also thank Cobb residents for
trusting the expertise of Wellstar to keep their families healthy and provide them with more than healthcare, PeopleCare.
Several Wellstar team members have been voted among the Best of Cobb:

How My Sister's Cancer Prepared Me For Mine
It is often said that we cannot define the bond of sisterhood. When that bond was tested not by distance or careers or even children but by stage IV cancer just 18 months apart, sisters Samantha McInturff and Amanda Glass, now 51 and 48 respectively, stepped up to help the other fight the biggest battle of their lives.
It was October of 2019 when Samantha McInturff's sister Amanda Glass was diagnosed with invasive ductal carcinoma, stage IV breast cancer, at the age of 44, through a routine mammogram. The cancer had metastasized to her liver, and she was placed on two different chemotherapy cocktails. Amanda had been living with Samantha and her family, who helped get her to treatments and doctor appointments. Scared they were going to lose Amanda, Samantha stood by her sister as she began her healing journey from the surgeries and the 38 rounds of daily radiation until September 2020, when she rang the bell! Today, Amanda is cancer-free.
Eighteen months to the day of Amanda's diagnosis, in March of 2021, Samantha found herself needing a colonoscopy after a positive noninvasive at-home colorectal cancer screening test from what she believed to be symptoms of hemorrhoids. At that moment, Samantha's life flashed before her eyes when her gastroenterologist told her she had colon cancer at 48 years old. She was now a stage four colorectal cancer patient with a small tumor in her lower colon and several tiny nodules on her lungs. What were the chances of two sisters finding their bond grow even stronger in the battle of their lives?
"I am thankful for my sister who walked through this before me. She was there for me when I needed her. My boys were in middle school when I was diagnosed. They weren't scared because they had watched my sister, who lived with us then, walk through her battle," Samantha shared.
Samantha had her first infusion treatment in April of 2021, and it was now Amanda's turn to stand by her sister. The treatments worked, and quarterly scans showed Samantha's nodules shrinking and disappearing. Nearly two years later, Samantha received the results the sisters had been waiting for—no evidence of residual, recurrent or metastatic disease. Samantha, too, was stable.
The sisters have one message—get screened! According to American Cancer Society research, colon cancer cases under age 50 are on the rise, and the recommendation is to get your colonoscopy at age 45. Furthermore, colorectal cancer is now the leading cause of cancer death in men and the second in women under 50 years old, making the overall lifetime risk of developing colorectal cancer about 1 in 23 for men and 1 in 25 for women. However, each person's risk might be higher or lower than this, depending on their risk factors.
Wellstar cares for the health and well-being of every person we serve, making a difference in thousands of lives every year—providing deeply compassionate care that takes each person’s unique life story into account and allows people to live their best lives. If you have a family history or symptoms, it is important to get screened earlier. Screening can prevent colorectal cancer by detecting and removing precancerous growths (polyps) and by detecting cancer at an early stage, allowing the treatments to be more successful. Regular adherence to screening reduces the risk of colorectal cancer incidence and death.
Wellstar is actively engaged with the American Cancer Society on several initiatives that address and support patients undergoing cancer treatments in Georgia. Visit cancer.org/getscreened to learn more.

Amanda Glass (left) and Samantha McInturff (right)

Fact or Fiction? Wellstar Cardiologist Breaks Down 5 Heart Health Trends
Every beat of your heart helps you do the things you love—it's vital to take care of your cardiovascular health. However, it can be challenging to know where to start and where to find informative, trustworthy resources, especially online.
Wellstar Cardiovascular Disease Specialist Dr. Eddie Hackler examined five trending heart health topics to help you separate fact from fiction.
You may have heard that fatty foods can actually boost your heart health, and that can be true—with some foods.
“Some fats are good for your heart. And my apologies to all the bacon-lovers out there, but the fats I’m talking about don’t come from red meat,” Dr. Hackler said.
Monosaturated fats, polyunsaturated fats and omega-3 fatty acids can support a healthy heart and lower your cholesterol. You’ll find these fats in foods such as olive oil, sunflower seeds, fatty fish—like salmon—and avocados.
We've all heard about fad juice cleanses and how they can “flush out toxins,” but the truth is they can do more harm than good.
“Most people who do juice cleanses frankly aren’t eating enough solid food to meet their nutritional needs,” Dr. Hackler said. “This quickly leads to tiredness, headaches and irritability.”
Instead of juicing, Dr. Hackler recommends eating fruits and veggies whole.
“You’ll get the vitamins without sacrificing the fiber and set yourself up for a healthier day.”
Can power walking make a difference in your heart health? Yes! You can actually walk your way to a longer life.
“A recent study shows that only 10 minutes a day improves your sleep, metabolism, mood, cognitive health and obesity risk,” Dr. Hackler said. “Look, it’s quick, affordable and completely worth it. Think about it as just a few songs’ worth of walking per day for a longer, healthier life. I’d take that deal.”
Some people say eggs are great for you. Others say they’re sure to increase your cholesterol. The truth? It’s somewhere in between. Eggs can still be enjoyed in moderation as part of a heart-healthy diet.
“Egg yolks have high cholesterol levels, but for generally healthy people, a modest intake of no more than one large egg per day has not been found to increase your risk of heart attack, stroke or any type of cardiovascular disease,” Dr. Hackler said.
Most of the cholesterol in our bodies doesn't come from many of the foods we eat, but from those high in trans and saturated fats, according to Dr. Hackler.
“Cholesterol levels can still increase with egg consumption, so you can eat eggs, but try not to eat more than one a day. And if you’re looking for a healthy alternative, try egg whites.”
Can late nights lead to heart disease? Most adults need seven to eight hours of sleep a night. Without it, the body releases chemicals that make it harder to keep your heart rate and blood pressure low. Both are factors that contribute to heart disease.
“If you commit to meeting that seven- to eight-hour mark, you could lower your risk for heart disease by 20% compared to short sleepers,” Dr. Hackler said.
Getting a screening through the Know Your Heart program at Wellstar helps catch potential heart issues at the start—before they become a bigger problem. That means you can take action early and keep your heart going strong. The preventative assessment arms you with knowledge about your current cardiovascular health status. After the screening, you’ll understand your risk of heart disease, stroke, high blood pressure and other conditions. Call (770) 956-7827 to schedule a screening.
Learn more about how Wellstar supports patients with heart health concerns.
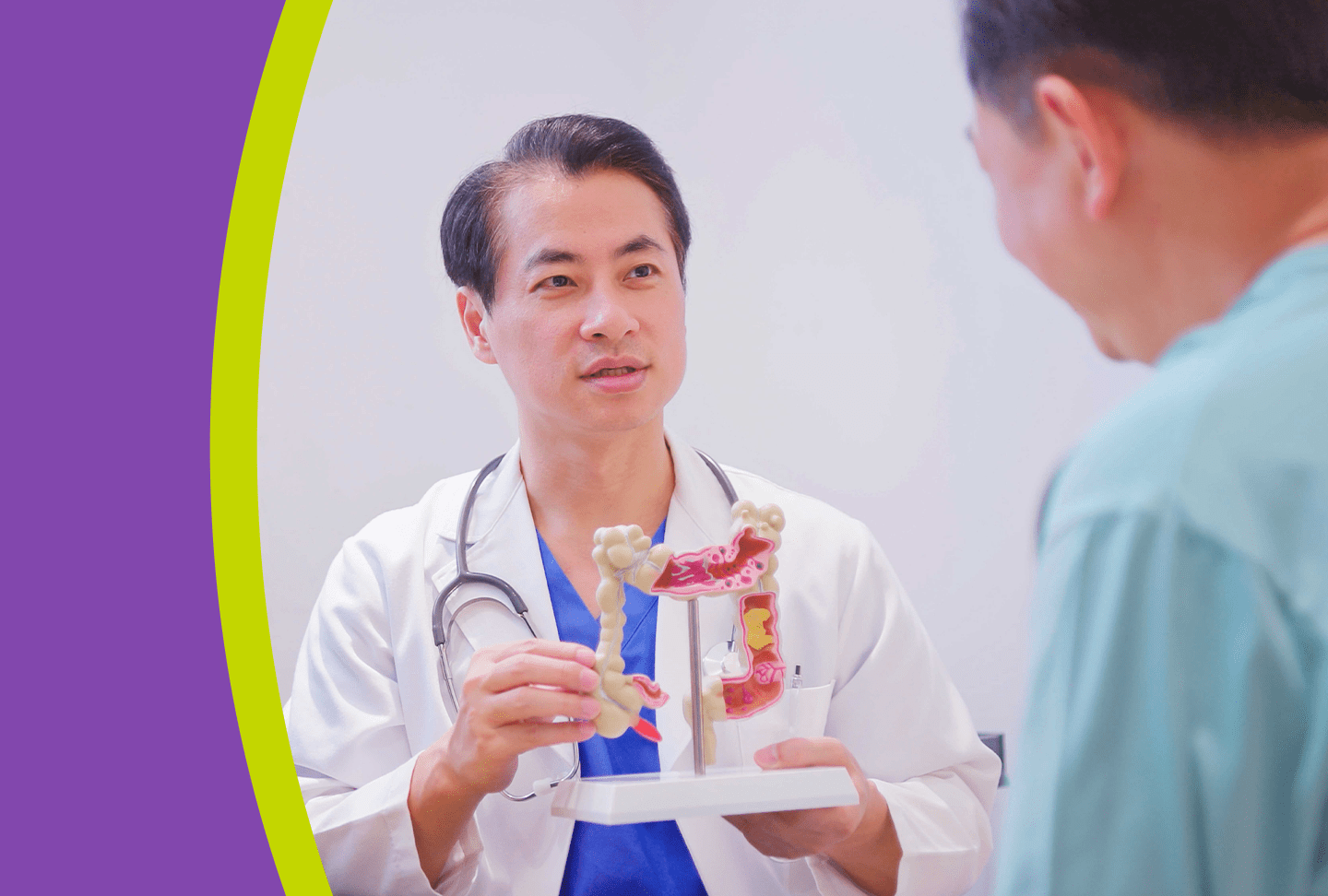
What to Know When You Are Diagnosed with Colorectal Cancer
More young adults—people in their 30s and 40s—are being diagnosed with colorectal cancer.
“I was in absolute shock,” said Samantha McInturff, a mother of two school-age children when she was diagnosed with stage 4 colon cancer at 48. “I was stunned. I probably didn’t ask enough questions.”
Like Samantha, patients don’t always think to ask questions on the spot. But questions come up once they’ve had a little time to process the news. That’s why we brought together a panel of gastrointestinal health experts and a colon cancer survivor to answer the questions you may have here.

What stage is my cancer and how will that affect my treatment plan?
Dr. Sahir Shroff, surgical oncologist: The staging of the cancer is a way to evaluate if the cancer is localized or if it has spread. It involves multiple imaging studies and blood tests.
For colon cancer, we mostly use CT scans of the chest, abdomen and pelvis with contrast. Sometimes we do a PET scan. CT scan results typically are in within a week of having the scan. For rectal cancer, the staging is a little more involved. We also do an MRI of the rectum itself to delineate the exact location and relationship of the tumor with related structures in the pelvis. Clear identification really helps us evaluate the best treatment for each patient.
The other part of staging is looking for a tumor biomarker called carcinoembryonic antigen—or CEA—a protein in the blood. Patients excrete excess amounts of CEA if they have colorectal cancer. Checking the CEA throughout treatment is a benchmark to see if the treatments are working. We typically have bloodwork results within a few hours.
If a patient has surgery, we send tissue removed during the operation to be analyzed and tell us a more accurate stage to determine the next phase of treatment.
Colorectal cancer treatment
What are my treatment options?
Dr. Shroff: Treatment of colorectal cancer is an evolving field. There have been so many changes around the most effective combinations of chemotherapy, immunotherapy, cancer surgery and radiation oncology. Recently, a non-operative treatment option has become available for patients with an excellent response to chemotherapy.
At Wellstar, we give patients access to the most comprehensive care for colorectal cancer, which includes genetic testing, clinical trials and the highest level of complex surgical procedures. Our specialists work collaboratively and follow the latest evidence-based practices. Everything we do is geared toward giving patients the most personalized care.
The types of treatment and the order of the different treatments vary depending on the type of cancer—rectal cancer or colon cancer—and personal factors such as the stage and location of the cancer.
Dr. Shani Clay, gastroenterologist: Patients can bring their family members in to accompany them at the time of their visits so that everyone has a good understanding of the treatment plan.

Wellstar Experts Demonstrate the Latest Robotic Technologies Used in Lung Cancer Care
Only 3.8% of those at high risk for cancer in Georgia are screened, according to the American Lung Association’s 2023 State of Lung Cancer report. To help enhance awareness and share the latest robotic technologies with healthcare professionals and community members, Wellstar held a Lung Cancer Showcase February 21 at the Atlanta Marriott Northwest in Cobb County. The event was held in a mobile laboratory with mock operating rooms and robotic surgical systems.
During the event, attended by several medical experts, Dr. Theolyn Price, Wellstar thoracic surgeon, and Dr. Timothy Udoji, Wellstar interventional pulmonologist, demonstrated how they use the Ion robotic bronchoscopy and da Vinci Xi surgical robotic system consecutively under a single anesthesia event to locate, biopsy and treat patients with early-stage lung cancer.
As she demonstrated how to control the da Vinci robot’s spider-like arms to perform surgeries, Dr. Price said, “See how I can use this clutch to move my arms up and down?” From there, she explained in detail how she cut away the cancerous tissue.
Dr. Udoji told participants how he uses the Ion robotic navigation bronchoscopy system to perform biopsies on potentially cancerous lung tissue, “This blue line shows exactly the pathway leading to the nodule inside the patient’s lung.”
The Ion robotic bronchoscopy system has safety features that ensure the instrument does not cause complications in other parts of the lung. Physicians can navigate and biopsy nodules in almost any part of the lungs.
Surgery is just one part of the treatment journey for some patients. Wellstar oncology nurse navigator Pam Plasket said, “We are dedicated to removing barriers to care and treatment. We promptly schedule appointments, connect patients to financial assistance and social support resources, and address transportation, housing and food insecurity needs.”
Wellstar nurse navigators know that shortening the journey for the patient is key and provides personalized care. At the Wellstar Specialty Teams and Treatments (STAT) Clinic, the goal is to move lung and esophageal cancer patients from diagnosis to initiating treatment within 14 days, which is facilitated by the multidisciplinary team of experts individualizing their care.
“It’s a privilege to help them. They have all my contact information and can reach out to me, and so can their caregivers,” Plasket said.
In addition to nurse navigators, several other teams were present to share information, including genetics, screening and lung cancer care. At Wellstar, patients have access to a suite of integrated services encompassing incidental lung nodule management, dedicated lung cancer screening and multidisciplinary lung cancer clinics (STAT Clinics).
Dr. Bill Mayfield, medical director of the Wellstar incidental lung nodule and lung cancer screening programs, explained, “Our goal is to broaden Wellstar’s ability to find lung cancers early and save more lives.” Additionally, patients with lung nodules not diagnosed with cancer but at high risk are monitored through regular lung cancer screening CTs or serial chest CTs if they do not qualify for lung cancer screenings.
Showcasing technologies and sharing the strengths of a comprehensive lung cancer program is just one step the team takes to enhance awareness of this unique and special program, available to all patients, from early detection to advanced treatment. Lung Cancer Awareness Month is held in November, but the team continues to increase outreach efforts year-round to build connections with consumers and educate the communities we serve.
You may learn more about the Ion robotic bronchoscopy and da Vinci Xi surgical systems online and read about our expert approach to comprehensive lung cancer at wellstar.org/lungcancer.
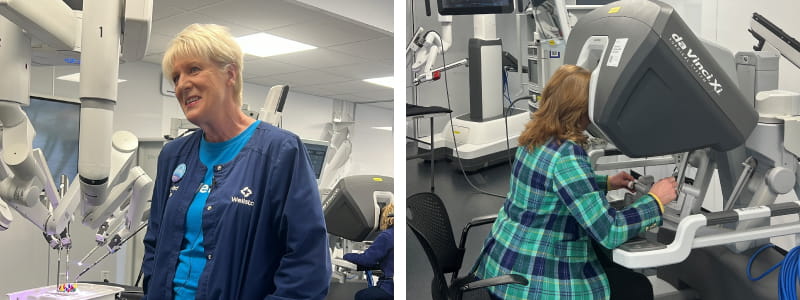
Left photo: Pam Plasket, Wellstar oncology nurse navigator, speaks with participants at the recent Lung Cancer Showcase. Right photo: Dr. Theolyn Price, Wellstar thoracic surgeon, explains how she uses the da Vinci robotic system to perform lung surgeries.

Forty Thousand Hand-Knit Happy Caps and Counting
There's no cap on giving back for thirteen-year lung cancer survivor Kathy DeJoseph. It was her first day getting chemotherapy when a woman approached Kathy and gifted her a knitted cap in appreciation for her kindness during her husband's cancer treatment. That simple act of gratitude inspired Kathy—and after completing treatment for her own cancer diagnosis, she decided to pay it forward by knitting caps for patients also undergoing chemotherapy and cancer treatments.
This passion project became a purpose project for Kathy as she soon found herself recruiting others who knit from across the nation. Knitters have joined from Pennsylvania to Michigan and Alabama to right here in Georgia to help Kathy's Happy Caps thrive.
Fostering meaningful connections within the Wellstar community is part of the charge for the group of volunteers, whose workshop is located at a Wellstar facility in Cobb County. The volunteers work multiple days a week to hand-knit and package caps donated to cancer patients at metro Atlanta oncology facilities, starting with the Wellstar Health System Cancer Centers.
Together, the group has donated more than 44,000 handmade caps and has no plans to slow down. So, we sat down with Kathy to learn what fuels her passion for knitting.
"So, they are each handmade with love by someone who cares and wants to make a difference for those facing cancer."
“Never! The first few years after I was sick, I volunteered to meet with newly diagnosed cancer patients so they could talk to a survivor.
At the five-year mark, my family suggested that I find another way to help cancer patients. I remembered how I felt when a stranger made me a hat when I was sick, and I decided to try my hand at knitting.
In just a couple of months, hats started showing up non-stop. Within a year, my house was full of hats, and we rented storage space where our volunteers would sort and process them. A year later, there were a couple of hundred volunteers, and after almost six years, we needed more space, and Wellstar met that need.
Sadly, there is no shortage of cancer patients, and so we continue to get new requests for Happy Caps from cancer centers. Now that I am getting older, and so are our volunteers, our volunteer base is getting smaller.”
“Just in metro Atlanta, tens of thousands are diagnosed with cancer each year. Most of our volunteers or someone they care about have been affected by cancer. Many are retirement age, but dozens are younger.
Some already knew how to knit or crochet, and others we taught or learned with online videos. They have even formed groups and meet at libraries or senior centers.”
“I need help reaching potential and current volunteers to meet the high demand. We receive donations that keep us in yarn to provide to volunteers, Wellstar generously provides us workspace, and no one is paid.”
Kathy and her volunteers are looking to grow their knitting network and asking their new friends across the country to pick up their needles and yarn and work to keep their mission thriving.
If you are interested in knitting Happy Caps or joining the team during their weekly knitting dates, reach out to Kathy at [email protected].

Left photo: Wellstar President and CEO Candice L. Saunders joins Happy Caps Founder Kathy DeJoseph. Right photo: Some of the more than 44,000 hats knitted by Happy Caps volunteers.

Make Colon Health Your Habit
For many people, talking about colon health can be a little uncomfortable. However, medical issues don’t just go away if you ignore them.
Being proactive about your well-being with preventative care can help catch colorectal cancer or another serious condition early, often before it becomes a bigger problem.
Wellstar is committed to keeping your colon healthy with preventative screenings and expert care, so you can continue to live well.
Early detection is the best prevention, especially when it comes to colon cancer. If caught early, colorectal cancer has a survival rate of 91%.
“Colon cancer is the second most common cause of cancer death in the United States, so it’s very important that everyone gets screened,” said Wellstar Gastroenterologist Dr. Cameron Body. “For an average risk person, screenings should begin at age 45.”
Those with a higher risk or a family history of colorectal cancer may need to start screening sooner. Partner with your provider to create a personalized screening plan—and stick with it to stay ahead of the disease.
“Recently, colon cancer has been a major trending topic in public discourse, and it has been impacting younger individuals each year. It is important to start colon cancer screening at the age of 45 or sooner if you have a family history of colon cancer,” said Wellstar Gastroenterologist Dr. Nikhil Kadle. “This is a preventable disease, so please speak with your primary care provider or gastroenterologist to help get you screened. Colonoscopies can help prevent colon cancer, diagnose and help direct early treatment if you are diagnosed.”
The death rate for colon cancer in older adults has been decreasing for the past several decades due to screenings, according to the American Cancer Society. Screenings can identify polyps before they become cancerous and can catch cancer earlier when it is more easily treatable. However, in people under 55, death rates from colon cancer have been increasing by about 1% per year since the mid-2000s.
During a colonoscopy, a Wellstar gastroenterologist will view the inside of your colon and look for polyps or any other abnormal tissue that could be cancerous. This preventative testing is key to catching colorectal issues at the start.
“A colonoscopy is the gold standard when screening for colon cancer. The procedure itself is not painful, and we make sure you’re comfortable throughout the process,” Dr. Body said. “The goal is to do a high-quality exam with a good prep to find polyps when they’re small and get them removed to minimize the risk of them subsequently developing into cancer.”
Polyps take about five to 15 years to evolve into an invasive cancer, according to Dr. Carmen Klass, oncologist and hematologist with Northwest Georgia Oncology Centers, a care partner of Wellstar.
“If you have a colonoscopy every five to 10 years, they can remove the polyp and it will never be declared an invasive cancer,” Dr. Klass said. “In fact, if all Americans did their screening colonoscopies every five to 10 years, the death rate for colorectal cancer would drop by 50%.”
See how colorectal cancer screening saves lives.
If you experience any of these symptoms, contact your care team right away.
If you have been diagnosed with colorectal cancer, count on Wellstar for comprehensive, personalized care. Our specialists will work together with you to form a tailored treatment plan and offer support every step of the way.
“When a patient is diagnosed with cancer, we walk with them and guide them on this difficult journey,” Dr. Klass said, sharing how Wellstar provides compassionate care.
Wellstar offers medical expertise close to home, clinical trials and state-of-the-art surgical procedures to treat colorectal cancer. We also have a multidisciplinary gastrointestinal (GI) tumor board that diagnoses and creates treatment plans collaboratively.
Along with cancer surgeons, medical oncologists and other experts, our care team also includes nurse navigators, dietitians, social workers, psychologists, psychiatrists and counselors to provide complete care and support.
Learn how Wellstar cares for colorectal cancer.
Whether you have been diagnosed with colorectal cancer or are concerned about the chance of developing it, genetic testing can help you understand your risk of getting the disease.
If your parent, sibling or child has had colorectal cancer, you are two to three times more likely to develop the condition compared with someone with no family history. Our genetic counselors can help determine how genetic testing could benefit you and your family.
“Wellstar offers support from genetic counselors to help keep other family members safe in the future,” Dr. Klass said.

Wellstar Pediatric Orthopedics Helps Gymnasts Get Back in Action with Gymnast’s Wrist Care
Gymnast’s wrist is a common overuse injury often seen in young gymnasts due to the repetitive high impact stresses put on the wrist during tumbling and vaulting. This injury is caused by irritation and inflammation to the growth plate at the end of the radius (the forearm bone on the thumb side of the wrist). Growth plates are often the site of injury in children and adolescents as they are made of cartilage, which is softer and weaker than the mature bone or ligaments around them.
Studies have shown that up to 88% of young gymnasts complain of wrist pain, with nearly half complaining of pain that lasts more than six months. If identified early, gymnast’s wrist responds wonderfully to nonoperative treatment. If there is a significant delay to treatment, it often requires lengthy immobilization and physical therapy.
Unlike other sports, gymnasts bear weight on their upper extremities and can transmit up to 16 times their body weight through their wrists during tumbling and vaulting. This repetitive high impact microtrauma leads to inflammation of the radial growth plate. This inflammation eventually causes damage to the growth plate that can be seen on X-rays as irregular bone edges, scarring or widening at the radial growth plate.
If not treated appropriately, gymnast’s wrist can lead to premature closure of the radial growth plate, causing the radius to be shorter than the ulna. This resulting asymmetry in length of the two forearm bones results in uneven stress distribution at the wrist with impact activities, which leads to chronic pain, stiffness and difficulty competing in gymnastics.
Patients experiencing gymnast’s wrist will feel pain, often described as aching, at the top of the wrist when they do an impact activity like tumbling. The pain usually starts gradually over a few weeks or months, typically when the patient has increased their physical activity or is trying a new activity.
“The patient may initially only feel the pain when they’re doing gymnastics, but it often progresses to bother them in daily life,” said Wellstar Sports Medicine Physician Dr. Steven Schulenborg. “They may have swelling and a decreased range of motion in their wrist.”
To remove stress from the growth plate and give it time to heal, providers will put the patient’s wrist in a brace or cast and recommend they avoid impact activities. Depending on the severity of the symptoms, treatment can take between six weeks and four or five months.
The team at Wellstar Pediatric Orthopedics is skilled in treating bone and joint conditions like gymnast’s wrist. To find a provider or make an appointment, visit our pediatric orthopedics page or call (404) 321-9900.

A Diamond-Cut Heart
Heart attack is the leading cause of death in Georgia, according to the American Heart Association. To save more lives, Wellstar provides advanced heart care services, ranging from minimally invasive procedures to open heart surgery. The health system recently expanded its offerings to bring an advanced technology called rotational atherectomy to more people in our community. The tool our physicians use for this procedure is called a Rotablator, which has a small but mighty diamond tip.
Who rotational atherectomy helps
Wellstar has offered percutaneous coronary intervention (PCI), formerly known as angioplasty, for a number of years. This procedure helps treat the main cause of heart attacks—the build-up of cholesterol filled plaque within a coronary artery. The build-up decreases blood flow and oxygen to the heart. By opening the artery, blood and oxygen can move freely once again.
The benefits of having a PCI typically include fewer complications, faster recovery time and shorter hospital stays.
Not everyone is a candidate for PCI, especially when the blockage is heavily calcified. But rotational atherectomy changes that.
“For heavily calcified coronary blockages, rotational atherectomy works as a drill to decrease the bulk of calcium,” said Wellstar interventional cardiologist Dr. Omer Mirza.
This technology makes non-surgical heart attack treatment available to people with more complex blockages that could not typically be cleared with balloon angioplasty.
Rotational atherectomy has been available at Wellstar Kennestone Regional Medical Center, and now we have expanded availability recently to Wellstar Cobb Medical Center.
“By expanding Wellstar Cobb’s technology, we can offer more comprehensive care for the patient and prevent transfers and subsequent delays to patient care,” Dr. Mirza said.
How rotational atherectomy works
At Wellstar, a rotational atherectomy is performed using a Rotablator, a small, diamond-tipped tool. This revolving instrument is inserted into the blocked artery using a catheter while a patient is under local anesthesia.
When the interventional cardiologist guides the Rotablator to the blockage, it begins to rotate, going as fast as 190,000 rpm. It gently breaks apart the blockage, making the plaque particles small enough to pass safely through the bloodstream.
Stents are then placed in the artery to widen it so blood can flow through. This procedure can improve blood flow and heart function within minutes.
Effective treatment with advanced technology
Studies indicate that rotational atherectomy results in high procedural success rates.
Giving patients the ability to resume normal activities within a few days, the recovery time for this procedure is significantly less than open heart surgery. Patients undergoing a rotational atherectomy typically spend one night in the hospital.
Learn more about interventional cardiology at Wellstar or find a specialist near you.

Overcoming obstacles: How one health system is creating a more inclusive health care future
Republished Content: Atlanta Business Chronicle
This article was originally published on Atlanta Business Chronicle on January 6, 2024.
Primary care is the initial and ongoing healthcare individuals receive from pediatricians, internal medicine or family care providers from prevention to the management of common health issues. Primary care fosters enduring patient-clinician relationships and facilitates specialized care when needed. Insufficient primary care can lead to delayed or inadequate medical attention, resulting in undetected health issues, unmanaged chronic conditions and increased reliance on emergency services—which can have significant cost impacts.
Without a robust primary care system, preventive measures, early intervention and continuity of care are compromised, contributing to poorer health outcomes, higher healthcare costs and strain on emergency resources. According to data compiled by the Kaiser Family Foundation, approximately 3.3 million—a third of Georgians— reside in an area grappling with a shortage of primary care. Recognizing the urgency and importance of addressing this issue, leaders from Wellstar Health System joined the Atlanta Business Chronicle for a panel discussion. The conversation delved into the crucial significance of primary care and the challenges that persist, shedding light on the need for strategic solutions in healthcare management.

David Rubinger: What strategies can community health providers use to reach out to individuals who haven’t sought medical care until they end up in the emergency room with a chronic condition? What specific approaches does Wellstar employ to effectively bring people into the healthcare system in a more manageable and proactive manner?
Dr. Jeffrey Tharp: Outreach is pivotal in addressing the root issues you mentioned. We understand that a person’s health significantly influences their lifestyle and quality of life. At Wellstar, we actively raise awareness, an integral part of the fabric that emphasizes the importance of a healthier lifestyle. Interestingly, insurance companies play a role in this by recognizing the cost benefits of keeping individuals healthy. Many insured individuals receive outreach, even in their homes, encouraging health assessments and connecting with primary care physicians.
Wellstar conducts numerous community campaigns through various channels, including community events, the media and in our offices and hospitals, highlighting the value of maintaining health and establishing a relationship with a primary care physician.
Elise Lockamy-Kassim: To add on to what Dr. Tharp said about reaching out to the community, we know health results are driven by non-health issues. The majority of our health outcomes are attributed to other things like where we live, where we go to work, where we send our children. Health literacy is needed outside health providers’ offices. Wellstar partners with organizations like Ser Familia to reach Spanish speakers and connect them with health resources in their community. Another example is our partnership with BLKHLTH. African Americans are about 20% more likely to get colorectal cancer and about 40% more likely to die from it than most other groups according to the American Cancer Society. Together, we distribute colorectal cancer kits to the community members that enable them to test and get results at home.
Rubinger: What factors contribute to men’s lower likelihood of seeking medical attention?
Dr. Dean Seehusen: It hasn’t been a cultural norm in America for men to seek out healthcare. I think part of it is also about the interaction that families have had with medicine over the years. Women get screening tests at a much younger age than men, like pap smears and mammograms, on a regular, ongoing basis. Considering traditional family dynamics, who also takes children to the doctor? Traditionally, it was the mother. She was going to the doctor herself annually, and men waited until they had chest pain for the first time. There wasn’t that equivalent of an annual exam associated with screening tests that men had in customary American medicine.
Rubinger: I’ve noticed a positive shift in the American health community acknowledging and addressing the reluctance of men to prioritize health check-ups. Recent advertising featuring athletes, unconventional in traditional public service ads, indicates a cultural change. How do you perceive the impact of technological advancements in further influencing the healthcare narrative and possibly addressing the healthcare-seeking behavior within the male dynamic?
Lockamy-Kassim: If I put on an equity lens, I could think of the male population as an underserved group in healthcare in certain ways. We’re addressing that, especially in the Center for Health Equity here at Wellstar, because we are bringing care, awareness, health literacy and health education to people where they are.
We’ve had many campaigns with people at churches and social service agencies where they just live their lives. We will bring the healthcare to you and that represents a shift. Across the industry, we’re returning it to where it used to be when you had a doctor make house calls. We see the benefits of that model.
Rubinger: Amid the challenges of COVID, a silver lining is the increased accessibility of healthcare through telemedicine. The positive aspect lies in the enhanced efficiency of interactions and features like online scheduling. How has that changed how you all practice medicine?
Dr. Seehusen: Wellstar is leading the way in telehealth. We are contacting many rural parts of Georgia, not just the Augusta or Atlanta area. There’s a statewide network that we are reaching out to via telehealth that includes ICU and emergency care, and we’re even doing a lot of hospital-type care at home now. It’s paving the way for the future of what healthcare can look like.
On the flip side, when we try to deliver primary care via telemedicine, equity becomes an issue. There is a subset of our patients who do not have the hardware or do not live in a neighborhood that has Wi-Fi connectivity. There is still work to be done on the primary care side with telemedicine. Once you get into the more specialized care, we’re doing some fantastic things that I’m proud of.
Dr. Tharp: To echo Dr. Seehusen, what has been done at Augusta University has really led the way for much of what the rest of us have learned along the way. Virtual care is a skill set that primary care physicians rarely had before COVID—how to perform it or what was appropriate to do via telemedicine.
The access issue is a double-edged sword. It does help some people, but on the other hand, there are areas where broadband is not great, or you have elderly folks who may not know technology. We must ensure that we give appropriate care when it needs to be in-person versus virtually and provide access to technology to as many people as possible who can’t afford that luxury.
Lockamy-Kassim: Evolving patient needs have forced us to grow as innovatively and quickly as the industry grows. In a church setting, we provide broadband hotspots, laptops and free services to individuals we encounter. You’re going to learn the signs and symptoms of whatever health topic we’re addressing. We will give you the tools to access primary care. We’ve had to be creative with our funding and partnerships to make sure we’re not creating more inequity as we pursue this new space.
Dr. Tharp: An example of patient care improvement as a result of the pandemic, particularly with the diabetes epidemic, is the advent and promotion of virtual diabetic education classes. Previously, multi-hour comprehensive diabetic classes could be difficult to schedule with respect to work and family responsibilities and transportation. Having the ability to do all that virtually has increased people’s knowledge, and we’re seeing metrics improve in diabetic control, almost to the same degree as adding on another medicine. It’s a vivid example of how we’ve been able to use this technology and help people’s lives on the primary care side.
Rubinger: Unfortunately, people would use their emergency room as their primary care physician. What can be done to help educate people on where they should go first, and how do you decide which care is best for your medical situation?
Tharp: There are different values when having a relationship with a primary care physician, such as access, quality of care and individualized care. When starting that relationship, there’s often an access problem since there are so few primary care physicians in the state and nation to accommodate our needs.
One tactic in building relationships with patients is connecting them with a specific physician or practice when they visit the emergency room. Although the process isn’t perfect, having a designated contact helps streamline communication. When a patient is identified, the initial step is knowing who to call, and from there, the referral process can begin. While it may not always be as fast as desired, establishing this relationship can also involve routing the referral through an urgent care facility in some instances. Having your own primary care physician can help you overcome some of the difficulty in navigating the U.S. healthcare system. Those benefits we see with that primary care patient relationship must start with knowing who to call.
Seehusen: Once a patient has experienced primary care with a provider they regularly see, establishing a relationship with true continuity occurs. This provider ideally knows not just the patient but also their entire family and medical history. It’s about getting them into the door. Then, we must develop systems where, again, access exists. The faces are stable enough that even if it’s not the same one face, it’s at least a small team of clinicians who are seeing that patient repeatedly.
A small team might be made of one physician and a couple of nurse practitioners and that small team really gets to know that patient and vice versa. You won’t have to convince those patients of the value of primary care. Those patients are much less likely to show up at an urgent care center or the emergency room because they know they want to see that team.
Lockamy-Kassim: While conducting our Community Health Needs Assessment, we held a Community Summit—a community-centered event similar to a focus group. With community members in each of our service areas, we identified access to care as a critical community challenge. One of the first aspects they mentioned as being the best asset in their community was the presence of a Wellstar Graduate Medical Education clinic or primary care facility. We know that neighborhoods are comprised differently. One of the ways that we can make entry points for primary care instead of the emergency room is to have primary care facilities in high-need ZIP codes.

The Heart of the Matter
With Valentine's Day approaching, there seems to be more than love in the air; there is loneliness, too. So, how does love affect our health?
Humans desire connections; we are wired to love and be loved. Feelings of closeness help individuals navigate challenges in both their physical and mental well-being. Being close to others is crucial for mental health, and loneliness can often play a role in worsening psychiatric conditions and major depressive disorders.
In this season of love, Wellstar is dedicated to providing support and care, helping individuals navigate the emotional challenges that may arise, and fostering a community connected by compassion and well-being.
For advice on this timely topic, we asked Dr. Justin Ayankola, medical director of Wellstar Collaborative Care Psychiatry, to help us understand how the heart affects the mind.
"Giving ourselves permission to love and be loved is critical to our well-being because love is the glue that ties communities together.”
For some, this season can trigger depressive feelings, so we wondered how we could go about preparing ourselves for the emotions we might feel during the upcoming holiday.
"The best way to prepare for a difficult time is to optimize your physical, emotional, mental, and spiritual health. Emotionally, being surrounded by people you love and care about is important. It is not the time to explore or salvage relationships.
Practices such as meditation and gratitude journaling can help increase resilience and decrease feelings of loneliness."
Did you know that research indicates both pleasant conversations and physical touch trigger the release of oxytocin? Just 30 minutes of in-person interactions, including a hug, can help release this hormone in our brains.
There is a common misconception that being in a relationship brings an individual "wholeness." Still, a critical part of finding love is loving oneself first, so how does nurturing that relationship help our mental health?
"Prioritizing self-care is equally important in tending to our mental health. Surprisingly, the most significant barrier to forming relationships often lies not in our feelings toward others but our feelings about ourselves.
Love is about connections. These healthy connections take effort to form and trust to keep. We should be aware that even when we focus on self-love, it is an action that is still dependent on relationships with others. It isn't easy to love ourselves while not giving love to others. The work of self-love and giving love must happen simultaneously."
There has often been a connection between Valentine's Day and loneliness or reminders of toxic situations affecting our mental health.
"Toxic relationships are connections that are destructive. There are numerous ways in which these types of relationships manifest; however, the result is often isolation and stress. Stress has both biological and psychological effects.
Biologically, there is an increase in cortisol, which, if elevated chronically, can make individuals more susceptible to depression and anxiety. The isolation that often accompanies toxic relationships only exacerbates these issues."
For many, the pressures of dating and finding "the one" can cause anxiety. Some find online dating a way to seek companionship, but swiping right and left can overwhelm the heart and mind. How do the brain and heart handle the ways of modern love?
"Online dating apps can be invaluable tools for connecting with others. In fact, many people who meet people on dating apps say it led to an exclusive, romantic relationship. However, they should be used responsibly, considering one's vulnerabilities and insecurities.
One size does not fit all. I recommend using apps that do not cater to a person's more problematic habits. Dating apps can facilitate connections for individuals but should not be the sole means for bringing love into their lives."
If you are wondering where to turn if you need help, scheduling an appointment with your primary care provider can be a great way to connect with a behavioral health clinician.

Wellstar Announces Retirement of Jim Budzinski, EVP & Chief Financial Officer After 15-Plus Years of Service
Please join us in extending best wishes to Jim Budzinski, executive vice president and chief financial officer, on his decision to retire.
Jim joined Wellstar in 2008 and has led critical initiatives and strategies that created the foundation for the Wellstar we know today. He has worn many hats during his tenure, including bold champion of our managed care division during significant periods of payer and provider discourse, first president of our highly successful Medicare Accountable Care Organization, head of information systems during our successful Epic implementation and leader of our supply chain team.
Jim has been recognized by the healthcare industry throughout his career. The American Hospital Association designated him an International Emerging Healthcare Leader early in his career. He received a bronze and silver award from the Healthcare Financial Management Association and was honored as one of Atlanta’s top CFOs by the Atlanta Business Chronicle. Last September, Jim was invited by the American Hospital Association to provide expert testimony before a United States House Committee on Ways and Means hearing on the patient impact of surprise medical billing.
Jim’s servant-leader heart and his passion to help others are evident in his decade of volunteerism with organizations like MUST Ministries and The Tommy Nobis Center, where he was recognized as a Thomas A. Slaughter Award recipient in 2016 and as a Community Champion in 2022.
We would like to thank Jim for his years of dedicated service to Wellstar, our patients and our communities. We wish him all the best and can be assured that after a career that spanned five decades, with the last 15-plus years at Wellstar, Jim has earned the opportunity to enjoy his retirement with his wife Deb, his three adult children and his seven grandchildren.

Newsweek Names Wellstar Among America's Greatest Workplaces for Diversity
Wellstar is honored to be recognized by Newsweek as one of America's Greatest Workplaces for Diversity in 2024. According to Newsweek, Wellstar and the other large and mid-size companies were identified for “genuinely respecting and valuing individuals from different walks of life.”
“Our commitment to diversity, equity, inclusion, and belonging is part of our roadmap for success as a healthcare organization,” added Le Joyce Naylor, SVP and chief diversity, equity, and inclusion officer at Wellstar. “It is mission-driven work that touches everything we do, beginning with how we care for our patients, team members, and communities. It is also an ongoing journey that impacts our every action and is demonstrated in the compassionate care we provide to the people in the communities we serve.”
For a second year in a row, Wellstar was named to the list. Newsweek and market data research firm Plant-A Insights Group utilized public data, interviews with HR professionals and an anonymous online survey to determine the scoring. Wellstar, with more than 31,000 team members, is included in the large company category.
With the support of systemwide DEI ambassadors, physicians and team members are trained to increase their cultural competency and awareness of patients, team members and community members from all walks of life. Examples of this programming includes:
“We are cultivating an environment where every individual feels valued, heard, included, and can have a true sense of belonging,” said Naylor. “Fostering a sense of belonging is more than a goal. It’s a fundamental part of our culture. We’re creating spaces where everyone can thrive, contribute their unique perspectives, and become an integral part of our collective success."
PatCare
Pat Gelisse has been dancing for 30 years. She even taught the Carolina shag for a while. It’s a partner dance, sometimes compared to Swing dancing to beach music.
But severe heart failure downgraded Pat’s dancing queen status for close to 10 years.
“I went from feeling happy to feeling like a nothing,” she remembered of that time in her life.
With a team of Wellstar heart specialists working together for her, Pat found hope and new life on the dance floor.
It started more than a decade ago when Pat lived in central Georgia. She scheduled a doctor’s appointment for what she thought was acid reflux. She popped in on a quick break from her marketing job, assuming it wouldn’t take long.
Blood work and an EKG got Pat a ticket straight to the hospital and a quadruple bypass.
“My heart got worse; it wasn’t pumping blood,” Pat said.
She was in acute heart failure, a life-threatening condition where the heart doesn’t pump well enough to deliver the necessary amount of oxygen to her body. Pat’s ejection fraction (EF)—the percentage measurement of the blood that leaves the heart each time it pumps—was only 10%. The normal range is 50 to 70%.
It was a scary time, and with a family history of heart problems, Pat was worried. She’d lost both parents to heart failure, as well as other family members.
“I just knew for sure I was going to be next,” said Pat.
Doctors from various academic institutions discussed serious treatments ranging from LVAD to transplant, but because the pumping performance of her heart improved, she was no longer a candidate for those procedures. Instead, Pat spent close to nine years managing her heart failure with a pacemaker and various medications—treatments that failed to get her back on the dance floor.

Wellstar Pediatric Orthopedics Cares for Children’s Growing Bones
Children are not just smaller-size adults. Their bones and joints are still growing, and they need specialized expertise. Children and adults require different care and treatments, and the providers at Wellstar Pediatric Orthopedics are experts in caring for children’s bones.
The skeleton is continuously renewing itself throughout our lifetime. During this process, older bone is removed and replaced with newer bone.
“As the child grows during childhood through adolescence, their body forms new bone quicker than the older bone is removed,” said Wellstar Pediatric Orthopedic Surgeon Dr. Lindsay Stephenson. “It is this process that allows for the bones to become denser.”
Peak bone mass is usually achieved in our 20s. In addition to a healthy diet, regular weight bearing and resistance exercises are also beneficial to building a strong skeleton.
There are many other differences between the bones of children and adults. In fact, when born, the body has about 300 bones. Some of these bones fuse together during growth and the final count in the adult skeleton is 206 distinct bones.
Another important difference is that children’s bones are still growing. This growth is both in the length of the bone and the diameter (or width) of the bone. Bones grow longer from a specialized area of the bone called the physis, which is also known as the growth plate. Because children have an active (or open) growth plate, there are special considerations when the bone is fractured. One of these is an advantage for children. Because of the growth capacity in their bones, it is possible that fractures that are not perfectly aligned can heal and the bone may straighten out during the process of natural growth. This means that fractures that would require surgery in an adult do not necessarily require as intense treatment in a child.
The disadvantage, however, is that in some cases, the fracture can involve the growth plate, known as a physeal fracture. In some patients, usually those with more severe physeal fractures, there is a risk that the growth plate is damaged and can result in abnormal growth of the bone after the fracture is healed. A pediatric orthopedic surgeon is trained to treat these injuries and to monitor the bone for evidence of a developing issue with bone growth.
Wellstar pediatric orthopedic specialists evaluate the whole child to assess how an orthopedic condition affects their overall health and wellness. To schedule an appointment for your child, visit wellstar.org/pedsortho or call (404) 321-9900.

Can Vitamins and Supplements Support Me in My Wellness Goals?
Many patients take dietary supplements to fill the gaps in their diet or be proactive against disease. But with all the different brands and products available, it can be difficult to decide which vitamin or supplement could be beneficial—and what could even be harmful or detrimental to your health goals.
According to the National Health and Nutrition Survey, 57.6% of adults aged 20 and over reported using any dietary supplement in the past 30 days, and dietary supplement use is more common among older adults, with 74.3% of adults 60 and older reporting supplement use.
Since 1994, dietary supplements have not needed the authorization of the U.S. Food and Drug Administration to be manufactured and sold, due to the Dietary Supplement Health and Education Act of 1994. This act left manufacturers to their own devices to evaluate the safety of their products, as well as the labeling on those products.
One of the problems in assessing multivitamins is the vast selection of options available. One brand of multivitamin may contain different amounts and different vitamins compared to another brand. Therefore, it is hard to accurately evaluate the benefits of taking multivitamins and their possible effect on conditions such as cardiovascular disease and cancer since these vitamins are often made differently.
If you’re concerned about getting the vitamins and minerals you need to stay healthy, your Wellstar primary care provider can work with you on a tailored nutritional plan and can refer you to a dietitian if needed.
“The majority of the vitamins that individuals are attempting to supplement when they take vitamins are already available in their diet,” said Wellstar Primary Care Physician Dr. Randy Hines.
Vitamins and minerals are better used and absorbed by the body when eaten rather than consumed in a pill, according to Dr. Hines.
The various B vitamins are available in lean meats, grains, fish and nuts. The antioxidant vitamins (A, C and E) are plentiful in dairy products, fruits and vegetables. Those who truly need to take supplements may have dietary restrictions, chronic conditions such as alcoholism or live in food-deficient areas where vitamins aren’t readily available. Those who don’t fit into those categories can supplement vitamins and minerals through changing their dietary habits.
It’s also important to make sure that there will not be any interactions between supplements and medications that could lead to health concerns or change the medicine’s effectiveness.
Find a Wellstar primary care provider who can work with you to accomplish your health and nutrition goals.

Access Customized Care Plans Online with Wellstar E-Visits
If you’re a MyChart user, E-visits are a convenient way for you to receive care from a Wellstar provider without needing to schedule an appointment or come to the clinic.
In addition to virtual visits and WellstarON, our online urgent care service, Wellstar has expanded access to care with E-visits. These visits are completed using our secure patient portal and offer treatment for non-emergency conditions.
Through MyChart, tell us about your health concern by answering a few questions about yourself and your symptoms, then a primary care provider will respond in MyChart with your care plan.
Conditions that can be treated with an E-visit include:
Log on to MyChart and click Symptom Checker from the menu in the top left of the screen. Select your condition and confirm you are currently located in Georgia. We’ll ask for information about your medications, allergies, health history and preferred pharmacy so that our team can tailor care specifically for you. Next you’ll see the estimated cost for your visit. Finally, click Submit to contact our care team. One of our providers will follow up with your care plan.
“A Wellstar primary care provider will review the information about your symptoms and health history, and we’ll create a customized care plan just for you,” said Wellstar Primary Care Physician Dr. Monika Karakattu. “E-visits offer the same personalized care you’d receive in person at Wellstar, conveniently delivered online and on your schedule.”
Learn more about getting care with an E-visit.
If you don’t have MyChart, you can make an account online if you are an established Wellstar patient. With MyChart, you can securely access all your health records with a single username and password. Once you’re connected, you can view your test results, schedule appointments, request prescription refills and pay your bills.
Not a Wellstar patient yet? Find a primary care provider here.

Accessing COVID-19 Medications with Wellstar
If you test positive for COVID-19 and are experiencing mild to moderate symptoms, your Wellstar care team can help you get back to feeling better with Paxlovid.
Paxlovid is an antiviral medication that can be prescribed to patients who are 12 or older and weigh at least 88 pounds. It’s best to start the medication as soon as possible, and you must begin taking it within five days of your first symptoms. Paxlovid is a pill you can take at home.
Read the U.S. Food and Drug Administration’s fact sheet about Paxlovid.
If you are feeling sick, you have several options for care. Learn more about the types of care available at Wellstar and what is right for your health needs.
If you have tested positive for COVID-19 with a home test and have mild symptoms, you can speak with a provider using WellstarON, our virtual urgent care service. The WellstarON provider will evaluate your symptoms and work with you on a personalized care plan, including a prescription for Paxlovid if appropriate.
Patients who have tested positive with a home test can also call their Wellstar primary care provider about a Paxlovid prescription or visit a retail pharmacy to be assessed by a pharmacist.
Wellstar retail pharmacies and many other pharmacy locations can fill Paxlovid prescriptions. Your Wellstar provider can send your prescription to your local pharmacy.
Find a location that offers COVID-19 testing and treatment. At these locations, patients are either tested on site or can bring in a positive test result from another testing site or an at-home test. Eligible patients will receive a prescription and can have that prescription filled on site.
As new variants of COVID-19 emerge, it’s important to remain vigilant. You can do your part to “stick it to COVID” and keep yourself and the community safe by getting vaccinated. The COVID-19 vaccine is available at a Georgia Department of Public Health location or your local retail pharmacy. Find a vaccination site near you.
Wellstar Honors 2024 MLK Day with Live Event featuring Ambassador Andrew Young
On Thursday, January 11, Wellstar presented its annual Martin Luther King, Jr. Program. The live-streamed event paid tribute to Dr. King’s impact and provided an opportunity to reflect on his extraordinary life and legacy. The 2024 celebration featured a performance from members of the world-renowned choir, Kevin Lemons’ Higher Calling, and a compelling conversation between Ambassador Andrew Young, Congressman, Mayor, revered Civil Rights icon and close friend to Dr. King, and Monica Pearson, former Atlanta news anchor and current host for CBS46 and Peachtree TV.
Ebenezer Baptist Church, located in the heart of Atlanta’s historic Auburn Avenue, served as a preeminent location for the program’s discussion and recording. Functioning as a central hub for several pivotal moments in the Civil Rights Movement and Dr. King’s ministry, Ebenezer Baptist Church served as a powerful setting for the events of the program and added a significant connection to our shared history.
The featured discussion between Ambassador Young and Monica focuses on Dr. King’s words, “Our lives begin to end the day we become silent about things that matter." Over the course of the conversation, Ambassador Young shares firsthand experiences from his work alongside Dr. King, including reflecting on how Dr. King’s first speech came to be recorded, how the King family’s positive impact and influence in the Atlanta business community contributed to the legacy of Ebeneezer Baptist Church and the global reaction to Dr. King winning the Nobel Peace Prize. He also addresses his instrumental role in the Civil Rights Movement – often serving as a negotiator and mediator in pivotal moments or times of conflict. Further exploring these elements, Ambassador Young highlights the importance of Black and White Atlantans working together and the city’s transition as it progressed from the early Civil Rights Movement to the present day.
Ambassador Young concludes by emphasizing the important impact healthcare team members make in the communities they serve, noting that this work is critical to the progress and prosperity of every city, state and nation. He underscores that robust, balanced healthcare systems like Wellstar are essential to the survival of every community and to the health and well-being of their members.
Wellstar is steadfast in its commitment to ensuring a safe and inclusive environment for every patient, family and team member. Delivering personalized care, comprehensive programs and valuable tools and resources that enrich and empower all Georgians is critical to nurturing a culture of belonging and advancing health equity in our communities. The Wellstar Office of Diversity, Equity, Inclusion and Belonging pioneers the creation of initiatives, including the annual Martin Luther King, Jr. event, that aim to enhance cultural competency, develop workforce diversity, positively influence health equity and amplify community engagement.
To view our 2024 Martin Luther King, Jr. Program, click on the video below.

Cancer Surgeon Finds New Hope in a Newfound Talent
A cancer surgeon at Wellstar Health System since 2005, Dr. Sahir Shroff never thought his journey to medicine would lead him to find a passion for art. Referring to it as a "serendipitous encounter with painting," Dr. Shroff’s career led him to be a world-class cancer surgeon who sees sick patients as the Surgical Oncology Subsection lead and the Kennestone Cancer Steering Committee Chair. Throughout the years, he realized he needed an outlet to help compartmentalize his life and destress. That is where his newfound passion came into play.
Officially, his journey into art began about a year ago; painting became a means of meditation for Dr. Shroff. As time passed, he realized this hobby offered him something more valuable than he had ever dreamed of- peace and tranquility. "More than what I'm doing - it is what I need to do. It allows me to focus on things other than medicine." The instant he picked up the brush and started painting, he felt a weight lifted from his shoulders.
"I do not consider myself an artist. I am an amateur. I am self-taught; I experiment with different paint mediums and brushes to create the desired effect." Dr. Shroff continued, "Art has never been a big part of my life in the past. Being a physician, I have naturally gravitated towards the STEM topics."

Dr. Shroff was born in Mumbai, India, and completed his residency and fellowship in the United States. He met his now wife, Dr. Paulomi Shroff, a breast surgeon with Wellstar Health System in medical school, and they share a beautiful family. After becoming empty nesters in the past few years, Dr. Shroff realized converting one of his children's bedrooms into an art studio was the perfect culmination of his life's works and his newfound passion for art. Not only is it helping him, but Dr. Shroff has also found that art is a beautiful tool to connect to his patients. His canvasses line the walls at Kennestone Regional Medical Center's Cancer Center, where patients can find a time for respite from the chemotherapy and radiation treatments that so often fill their lives with the angst of the "C Word."
From his art titled "Home Coming" featuring the wildebeests and huts he has found along his travels to villages in Tanzania to the hyenas and big moon in his art 'Blue Moon in the Serengeti' and a cheetah and her cub in 'Now You See Them, Now You Don't.' These moments have inspired Dr. Shroff in so many ways. With this reflective approach to better understanding life's purpose, the love of art has been life-changing for Dr. Shroff, "our role as humans on this earth and our responsibility to safeguard this delicate ecosystem."

Wellstar Treats Atrial Fibrillation with Comprehensive, Tailored Care
Atrial fibrillation, also called AFib, occurs when the upper chambers of the heart—known as atria—beat irregularly and fail to pump blood efficiently to the rest of the body. It’s the most common heart arrhythmia, and at Wellstar, you’ll find comprehensive care and multiple treatment options for this condition.
The heart in AFib often responds by beating too fast, with potentially dangerous results. A normal heart rate is between 60 and 100 beats per minute, but a heart in AFib beats 100 to 175 times per minute. Though the heart is working hard, it is inefficiently pumping blood through the body and may restrict oxygen delivery.
The poor pumping function may also leave blood to collect in the atria, where clots can form. If a clot is pumped through the heart and into the body, it could reach the brain and cause a stroke. The risk of experiencing a stroke is about four to five times higher if someone has AFib, according to the American Heart Association.
Symptoms of AFib include:
If you experience any of these symptoms, seek medical care right away.
“If you are diagnosed with AFib, your Wellstar cardiologist will tailor your treatment plan, considering the condition of your heart and any other medical conditions you may have,” said Wellstar Cardiac Electrophysiologist Dr. Mohammad Kooshkabadi. “Their goals will be to reset your heart rhythm, prevent blood clots and reduce the risk of your AFib returning.”
Treatment options for AFib include:

Dietitian Reacts: 5 Health Food Trends
Christen Miller, Wellstar registered dietitian
By Christen Miller, Wellstar registered dietitian
In the ever-evolving world of diet and wellness, social media has become a breeding ground for the latest health food fads. As a registered Wellstar dietitian with experience helping hundreds of people lose weight and keep it off, my goal is to help you cut through the internet noise and develop a clean, balanced diet. So, without further ado, here are the 5 most popular health food fads and 5 corresponding tips to help you eat better than ever.
When you put fruits or vegetables into a juicer, you’re left with a liquid that contains most of the vitamins, minerals and plant chemicals found in those foods. If you’re someone who really doesn’t enjoy eating fruits and vegetables, then juicing is a good way to add those foods to your diet. However, there are downsides to juicing. Whole fruits and vegetables are packed with healthy fiber, which is lost during the juicing process. Fiber plays a big role in digestive health, so my recommendation to juicers is to consider putting your fruits and vegetables into a blender rather than a juicer. Blending still delivers all the vitamins and minerals of the fruit or vegetable while preserving the dietary fiber your stomach needs to run smoothly.
It might seem like a niche beverage, but mushroom coffee has exploded in popularity in the last few years. Typically, these products contain a mix of ground mushrooms and ground coffee beans. Marketers of these products make numerous claims regarding their health benefits, including stress reduction, reduced inflammation and better sleep. While it’s true that the adaptogens found in mushrooms may help achieve these effects, it’s important to note that the benefits are largely unproven. If you consume mushroom coffee and feel that it is beneficial, continue to enjoy it. This product, however, can be difficult to process, particularly if you have kidney or digestive issues. An alternative option is to simply enjoy fresh mushrooms added to meals and snacks instead.
Whether it’s on the internet, on a podcast or from a friend, almost everyone has heard about the keto diet. At a high level, the keto diet is a high-fat, low-carb diet designed to switch your body from using glucose (produced by carbohydrates) to using ketones (produced from fat) for energy. Typical foods consumed on the keto diet include things like eggs, avocados, salmon, butter, nuts (such as walnuts and pecans), low-carb veggies (like broccoli, spinach and kale) and unprocessed cheese. While there’s still not enough long-term data to conclusively say the diet is safe over a long period, it has produced great results for overweight or diabetic patients. This approach to food can help get your body out of metabolic crisis and into a healthier state. If you’re considering trying the keto diet, my recommendation would be to consult with your healthcare provider before doing so. They can make you aware of potential medical risks, so you can make an informed decision.
Despite the spicy taste of ginger shots, many people consume them to reap the root’s many health benefits. Perks of consuming ginger include helping with digestion and reducing inflammation, thanks to the active ingredient gingerol. There's some evidence that it can improve insulin sensitivity, helping to stabilize blood sugars, and it may even help to reduce cholesterol levels. Despite these benefits, one should still be mindful about this product. Ginger is known to cause heartburn in some people. If you're prone to heartburn, dilute ginger juice to help prevent this side effect. Additionally, if you already take a ginger supplement, there's no need to also take ginger shots. Consuming too much ginger may cause nausea and gastric reflux.
Collagen is one of the most universal protein sources in the body. It's a major component in our hair, skin, cartilage, tendons and even our bones. Recently, collagen supplements have risen to the top of many people’s daily wellness routines, thanks to their purported skin, hair and nail benefits. While the effectiveness of topical collagen skin creams and serums is doubtful, oral collagen supplements may actually be beneficial. Research is limited yet some studies have found that oral collagen supplements produce substantive improvements to skin elasticity as well as joint mobility. There are, however, notable conflicts of interest with many of these studies, given that most are funded, in some part, by related industries.
While social media can be a valuable source of inspiration, it's crucial to approach health food fads with a discerning eye. There's no one-size-fits-all solution to nutrition and balance is key. As a dietitian, my advice is to prioritize whole, minimally processed foods, tailor your choices to your individual needs and, when in doubt, seek guidance from a qualified nutrition professional. To schedule an appointment with an expert, visit Wellstar Center for Best Health, where you’ll find customized plans for childhood and adult obesity, diabetes management, cardiovascular disorders and so much more.
Christen Miller completed her dietetic internship at Life University and has more than 10 years of experience as a dietitian. She currently serves as a bariatric dietitian with Wellstar.

Wellstar’s social media content, and all related media, are provided for educational and informational purposes only and does not constitute providing medical advice or professional services. Consult a physician for the diet that’s best for you.

5 Fun and Easy After-School Snacks
Dr. Joanna Dolgoff, Wellstar pediatrician
By Dr. Joanna Dolgoff, Wellstar pediatrician
When school is in session, finding the perfect after-school snack that balances nutrition and deliciousness can feel like quite a task. As a board-certified Wellstar pediatrician, I understand the importance of fueling growing bodies with the right nutrients. With that, I'm excited to share five wholesome after-school snack ideas that are easy to make and fun for kids to eat.
This creative snack recipe offers a good balance of protein from peanut butter, along with a variety of fruits and vegetables, providing essential vitamins and antioxidants for growing children.
What You’ll Need:
Peanut butter
Celery
Grapes
Blueberries
Grape tomatoes
Candy eyes
Directions:
This recipe is excellent for kids as it combines the crisp sweetness of apples, a good source of fiber and vitamins, with protein-rich peanut butter and the added crunch of Cheerios to create a tasty and nutritionally balanced snack. Toothpicks may be a choking hazard for children, so supervise as your family makes and enjoys this snack.
What You’ll Need:
One apple
Peanut butter
Cheerios
Low-fat cheese
Toothpicks
Directions:
This krazy kabob recipe is a playful and nutritious way to encourage children to enjoy a variety of fruits. Filled with hydrating watermelon, sweet cantaloupe, refreshing honeydew, juicy pineapple, antioxidant-rich blueberries and grapes, these skewers provide a spectrum of vitamins and flavors, promoting a fun and healthy snacking experience for young taste buds.
What You’ll Need:
Watermelon
Cantaloupe
Honeydew
Pineapple
Blueberries
Grapes
Wood skewers
Fruit-shape cutters (stars, hearts, etc.)
Directions:
This wholesome veggie car recipe is a fun way to encourage children to enjoy their vegetables. With vibrant baby peppers and baby cucumbers, the snack not only provides essential vitamins, but also engages kids in a fun, hands-on experience of assembling their own veggie cars, promoting both healthy eating and interactive play. Toothpicks may be a choking hazard for children.
What You’ll Need:
10 baby peppers
Six baby cucumbers
Toothpicks
Directions:
These banana lollipops offer a delightful and healthier alternative to traditional sweets. With the natural sweetness of bananas and the richness of dark chocolate, the recipe makes for an enjoyable, nutritious after-school snack for kids of all ages.
What You’ll Need:
One banana
Chopped dark chocolate bar
Popsicle sticks
Wax paper and baking sheet
As a pediatrician dedicated to the well-being of children, these snack ideas offer more than delicious bites—they pave the way for a lifetime of healthy habits. Incorporating a variety of fruits and vegetables, these recipes not only provide essential vitamins and minerals, but also engage young minds in the joy of preparing and enjoying wholesome foods. Learn more about how to keep your kids happy and healthy by scheduling an appointment with a world-class Wellstar pediatrician today.
A graduate of New York University Grossman School of Medicine, Dr. Joanna Dolgoff is a board-certified pediatrician with Wellstar.

Wellstar’s content, and all related media, are provided for educational and informational purposes only and does not constitute providing medical advice or professional services. Consult a pediatrician for the diet that’s best for your child.

Santa Claus Visits Patients at Wellstar Children’s Hospital of Georgia
Santa Claus’ cheery “Ho, Ho, Ho” boomed through Christian Norris’ hospital room seconds before the jolly man entered the room himself.
Christian, age 3, wore a Santa and sat in the middle of his hospital bed at Wellstar Children’s Hospital of Georgia. He broke into a wide smile as the Jolly Old Elf came near. Santa gave Christian a large stuffed bear, a stuffed animal and a wrapped Christmas present.
On Christmas morning, Santa made his rounds at Wellstar Children’s, visiting patients like Christian, who couldn’t be home for Christmas.
Christian’s mother, Charlene Norris, said it meant a lot to her that Santa took the time to visit. “There’s joy for the children in times like this when they don’t understand anything. They don’t understand why this is happening to them,” she said. “Just to see them smile and to know that Christmas isn’t all about gifts at home. People came out to make sure that he had a Christmas, even if he was in the hospital.”
On Christmas Eve, Christian’s stomach began expanding and he started to dry heave. Not knowing what was wrong, Charlene brought him to the emergency room at Wellstar Children’s and the staff began running tests. Doctors are still working to determine what’s causing the problem, but they have ruled out a cancerous tumor, Charlene said.
She knows first-hand that Christian is in good hands.
“Believe it or not, I was a patient as a child here years ago under the old Medical College of Georgia,” said Charlene, who is an Augusta resident. “I’m a cardiac patient myself. Being here as a child and then being here as a parent with a child—it makes you more grateful that we didn’t have to go far.”
As she spoke, Christian unwrapped his gift. It was a toy doctor’s kit, and he busied himself exploring different tools inside and putting a cloth band aid on his leg.
“Some people have to come so far to get here. We are grateful to have this hospital here,” Charlene said.
Learn more about Wellstar Children’s and its pediatric services.

Creating Your PeopleCare Plan
At Wellstar, we deliver personalized care to every patient, every time. That’s because we know you are more than a number, diagnosis or medical chart. Our dedicated experts support you through every stage of your wellness journey, providing care that is as unique as you.
That’s what PeopleCare is all about.
Because we know preventative care plays a major role in staying healthy, our primary care providers (PCPs) will build a PeopleCare plan just for you.
Your PeopleCare plan is your unique blueprint for better health. It doesn’t look like anyone else’s. PCPs create tailored treatment plans for each patient, based on your health concerns, family medical history and results from routine wellness exams.
Using these building blocks, PCPs can form an action plan and often get ahead of major health problems like cancer, diabetes, and heart disease.
Wellness exams arm you with knowledge, so you can take control of your health.
No matter your age or medical history, it is recommended to get a medical check-up at least once a year. At your next doctor’s visit, make sure to “know your numbers” for:
For both men and women, basic wellness exams are an important step in staying healthy.
To schedule a primary care appointment, call (770) 956-STAR (7827) or click the “Book Now” button at the top of the page.

Wellstar Health System Provides Second Highest Charity Care Percentage Among Large U.S. Health Systems
According to a Modern Healthcare analysis of data from 255 health systems, Wellstar Health System provides the second-highest percentage of charity care among large nonprofit U.S. health systems. The rankings are based on a review of charity care reported as a portion of operating expenses for fiscal year 2022[1].
Wellstar devoted 6.11% of its operating expenses to charity care, making the system the top provider of charity care in the state and the second nationwide. As a nonprofit healthcare system, Wellstar is committed to bringing expert, compassionate health services to those who need them.
“Wellstar is committed to providing compassionate, expert care to the communities we serve,” Julie Teer, SVP and President of Wellstar Foundation, said. “As a nonprofit health system, we rely on the generosity of donors and strategic partnerships to help us expand access and impact. The Wellstar Foundation is the philanthropic arm of the health system and is fueling innovation and action to address the state’s most pressing health needs.”
Our nine safety net hospitals[2] care for every patient that comes through our doors, regardless of their ability to pay. Wellstar intentionally focuses on philanthropy and partnerships that support health equity, behavioral health, innovation, workforce development and clinical excellence initiatives. Each is critical to the health system’s efforts to provide holistic, tailored care that meets people’s health needs at every age and stage.
As we lead the way to a healthier Georgia, Wellstar is the only health system in the state with an established Center for Health Equity. The Wellstar Center for Health Equity (WCHE) is critical to reaching underserved communities. Every three years, a Community Health Needs Assessment is conducted to help better understand the unique health needs of the communities we serve – further enabling us to create and implement a plan to improve care and promote healthy lifestyles for every person regardless of their race, gender, culture or income.
“We are able to reach a broader range of people in need because of the partnerships we’ve formed,” Elise Lockamy-Kassim, AVP of the WCHE, said. “As a community, we are stronger together. Working with organizations like Goodr; Wholesome Wave Georgia; Healthy Mothers, Healthy Babies; Ser Familia, and hundreds of other partners, we’re able to make a much greater impact.”
Food insecurity is one of Wellstar’s six strategic initiatives because of the WCHE’s findings. Wellstar and the Wellstar Foundation first partnered with Goodr in 2020 to tackle food insecurity during the pandemic. Our partnership initially focused on Mobile Markets, pop-up grocery markets that provide food and fresh produce to thousands of families each year.
The partnership has evolved to also include a Surplus Food Recovery service where leftover food from hospitals and donated to community-based organizations. Most recently, the system launched an Organic Recycling Program with support from Goodr, the Wellstar Foundation, Catalyst by Wellstar and Wellstar Strategic Community Development.
At Wellstar, our strong commitment to clinical and community initiatives, designed to help enhance care and create a healthier Georgia, has recently grown with the addition of Wellstar MCG Health and Children’s Hospital of Georgia.
Please consider supporting Wellstar’s nonprofit work by making a tax-deductible donation through the Wellstar Foundation at wellstar.org/give.
[1] Source: Merritt Research Services, an Investortools Company
[2] Source: Georgia Department of Community Health, Safety Net Hospitals (2019 Data Year)

Make Your Preventative Care a Priority
From a balancing a busy work schedule to running errands around town, it can be easy to keep putting off important wellness appointments. However, an annual visit with your Wellstar primary care clinician is one of the best investments you can make in your health.
Just like building savings in a bank account, each preventative care appointment adds more value to your health. That’s because, instead of just getting treatment just when you feel sick or experience symptoms of a serious condition, preventative care helps you stay ahead of potential medical problems.
Taking the time to schedule an annual wellness exam can pay off in the long run.
At Wellstar, we believe preventative care is the key to living your fullest, healthiest life. During an annual exam, our primary care team uses preventative screenings to help catch major diseases early and prevent chronic conditions.
While different types of tests may be recommended based on your age, gender and medical history, common screenings include a:
Atypical results may indicate an increased risk of certain diseases like diabetes, heart disease or high blood pressure. Your primary care team may order extra testing or refer you for follow-up care with a Wellstar specialist, such as a cardiologist, neurologist or oncologist.
Medicare Annual Wellness Visit
The Annual Wellness Visit (AWV) gives you the opportunity to meet with your primary care provider to:
If you have a chronic disease or new illnesses, they should be discussed during your wellness visit. Treatment(s) may need to be addressed separately.
Learn more here:
Medicare.gov
Cigna.com
Humana.com
Aetna.com
Wellcare.com
Knowledge is power. Understanding the results of your wellness exams can help you take charge of your health and make informed decisions about your care.
The results of your health screenings may reveal certain personal risk factors. Some of your risk factors can’t be changed, such as your age, genetics or family medical history. Others are under your control and can be adjusted to help you live well, including eating a balanced diet, getting regular exercise and choosing not to smoke.
Understanding your test results and risk factors can help you become your own wellness advocate. Armed with knowledge about your health, you can often reduce the effects of a serious condition, improve your outcome or avoid certain health complications altogether.
Your wellness check-up is also a safe space to discuss your health goals and medical concerns. Whether you need help maintaining a healthy weight or managing a chronic condition, your Wellstar primary care clinician will create a tailored care plan just for you, based on your unique health needs.
Don’t delay your annual exam. Schedule a visit today by clicking the "Book Now" button at the top of any webpage.

Wellstar East Point clinic transition urgent care services to Southside on Jan. 12, 2024
ATLANTA (December 12, 2023) – After more than a year of collaboration and partnership between Southside Medical Center and Wellstar Health System to expand preventive and primary care services to the East Point community, the partners will complete the transition of urgent care services from Wellstar East Point Health Center (EPHC) to Southside Medical Center’s East Point clinic on Jan. 12, 2024.
As part of the partnership, Wellstar is investing $5 million over five years to help increase services and expand the Southside East Point clinic’s size and capacity. Wellstar is also committed to a thoughtful process to determine the future of the AMC South site, which includes ongoing cooperation with Dr. David Williams, president and CEO of Southside Medical Center, a Federally Qualified Health Center (FQHC).

About the Transition
Since announcing the partnership between Southside Medical Center and Wellstar in October 2022, the organizations have been working together to establish a medical home for patients who have received episodic care through the Wellstar EPHC urgent care facility.
With coordinated ongoing care, including preventive visits and management of chronic conditions, patients have had fewer medical needs that require urgent care visits. As a result, the average urgent care volume at Wellstar EPHC has dropped by almost 65%, from nearly 80 patients per day in October 2022 to 28 patients per day in November 2023.
Beginning the first week of January, Southside, a Federally Qualified Health Center (FQHC), will expand its urgent care hours of operation to seven days a week, from 8 a.m. to 7 p.m., for all patients regardless of insurance status or ability to pay.
Expanded Services
People who previously received urgent care services at Wellstar EPHC will have access to a greater range of services at Southside Medical Center's East Point clinic, which is located next door. In addition to urgent care, patients can receive primary care, pediatric care, dental care, OB/GYN services and immunizations at Southside’s East Point facility and support like mental health care services virtually.
Patients can also access substance abuse support and other specialty care like podiatry, basic optometry and urology at the main Southside Medical Center clinic location, located at 1046 Ridge Avenue, less than 10 minutes away from the East Point clinic.
As an FQHC with a patient-centered medical home (PCMH) designation, Southside’s East Point clinic provides enhanced patient access and other benefits, such as decreased pharmaceutical costs and free transportation to medical appointments.
Team Member and Community Transitions
Wellstar is committed to supporting all EPHC team members through this transition and is offering them positions at other Wellstar locations. Additionally, if any impacted Wellstar team member wants to continue serving the East Point community, Wellstar and Southside’s human resource teams will collaborate to offer them opportunities at Southside Medical Center locations.
Both organizations will also work throughout this final transition phase in close alignment with community leaders and partners.

PGA TOUR player Luke List Donates $250,000 to Wellstar Children’s Hospital of Georgia Through RSM Birdies Fore Love
Luke List, a PGA TOUR player, and his wife, Chloe, presented a check for $250,000 to Wellstar Children’s Hospital of Georgia Thursday, December 7. The donation, which was made possible by the proceeds earned when Luke won the RSM Birdies Fore Love charity competition during the 2022-2023 PGA TOUR season, will support the expansion of the Pediatric Intensive Care Unit at Georgia’s second largest children’s hospital.
The Lists’ son, Harrison, was born prematurely on June 5, 2021. After leaving the hospital, Harrison was soon readmitted due to RSV, a respiratory virus, and was intubated for two days. Ultimately, Harrison spent two weeks in the Pediatric Intensive Care Unit at Wellstar Children’s. Helping expand the unit is a cause that is near and dear to the Lists’ hearts.
“It means so much to me and my family to have this opportunity to give back,” Luke said. “We want to share our story just to have people know what they do here and how much they’re really giving and really changing lives.”
Wellstar Children’s is home to the highest level (Level I) Pediatric Intensive Care Unit referral center in the region, providing critical care to children suffering from trauma or serious illnesses. Its team of dedicated pediatric intensivists delivers round-the-clock care to more than 1,000 children annually. Currently, the Pediatric Intensive Care Unit has 14 private rooms to care for children. After the expansion that number will increase to 22 rooms, allowing more Georgia families to benefit from the expert care at Wellstar Children’s.
The RSM Birdies Fore Love competition awards the top player who accumulated the most birdies (or better) during the FedExCup Fall events with the opportunity to donate to their choice of children- and/or family-focused charitable organizations. The List family decided that Luke’s winnings would go to Wellstar Children’s.
Representatives from RSM joined the Lists to present the check to Wellstar Children’s. Since the program’s inception in 2018, RSM Birdies Fore Love has raised $5.25 million in donations for players’ charities, supporting over 85 different organizations. Four players have started their own foundations as a direct result of RSM Birdies Fore Love funds.

23rd iHeart Media Radiothon Raises $262,693 for Children's Hospital of Georgia
Christmas carols and telephones ringing filled the Wellstar Children’s Hospital of Georgia lobby December 7 through December 9, 2023 for the 23rd annual iHeartMedia Cares for Kids Radiothon.
Thanks to the generosity of supporters, a check for $262,693 was presented to Wellstar Children’s at the conclusion of Radiothon on Saturday, December 9.
Throughout the event, radio stations 104.3 WBBQ, 96.3 Kiss-FM and 105.7 The Bull broadcast live from the lobby while WRDW News 12/NBC 26 shared stories of hope. Families of pediatric patients who have successfully finished treatment or are undergoing treatment at Wellstar Children’s, which is a member of the Children’s Miracle Network, stopped by to share stories of the world-class care their children received from the caring staff and expert caregivers.
“Every dollar that’s raised this weekend with Radiothon stays right here at Wellstar Children’s Hospital of Georgia and directly benefits the care of the children,” said Pediatrician-in-Chief Dr. Valera Hudson. “We’re the second largest children’s hospital in Georgia and the only children’s hospital outside of Atlanta. We offer the highest level of care to the sickest and most complex children. We hope you never need us, but if you ever need us, we’re here.”
Donations to Radiothon are used to purchase much-needed items that are unique to a children’s hospital, such as a vein finder for the neonatal intensive care unit. This device shines a red light through an infant’s arm or leg and helps caregivers find their tiny veins without having to stick them with a needle multiple times to administer fluids and medications.
The funds are also used to provide additional supplies for patient care as needs arise.
Though Radiothon is over, pledges are accepted year-round by calling (706) 721-4004 or by visiting the Cares for Kids Radiothon website.

Wellstar Health System and Wellstar Foundation Recognized as the Only System in Georgia and One of 25 Nationwide to Receive a $2M Grant from The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA)
With nearly one in five Georgians struggling with mental health challenges annually, treating mental health conditions and assessing suicide risk is a group effort between health professionals and state, local, and community partners. The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), recognized Wellstar as the only system in Georgia and one of 25 nationwide to be awarded funding as part of a $2M Grant from the Biden-Harris Administration. The grant falls in the Cooperative Agreements to Implement Zero Suicide in Health Systems in the form of an intervention and prevention model for adults throughout our health system.
Wellstar launched a system-wide suicide prevention program in 2017 when the Behavioral Health Service Line adopted the national best-practice Zero Suicide Initiative (ZSI) framework developed by the Suicide Prevention Resource Center (SPRC) and the National Alliance for Suicide Prevention. During the earliest phases of implementation, Wellstar invited national experts from the SPRC to advise on best practices, hosted a series of focus groups with various Wellstar medical specialties and departments, conducted an organizational needs assessment, and convened a Zero Suicide Oversight Steering Council to oversee the development, implementation, and fidelity of the program.
"Behavioral health cannot own the problem alone independent of other members of the healthcare team. We have to consider a systemic approach – how we screen, assess, deliver care and address gaps throughout the entire healthcare continuum," explained Ryan Breshears, PhD, ABPP, chief of Wellstar's Behavioral Health service line and a board-certified clinical health psychologist.
Since the initial 2017 launch, Wellstar's Suicide Prevention Team has implemented an improved suicide screening process for all Wellstar emergency departments and medical floors. These experts have also routinized collaborative safety planning to ensure safety interventions are initiated at the onset of the patient encounter and throughout the duration of care.
“The support of our executive leadership to launch this program in 2017, ongoing system collaboration, and commitment from our suicide prevention team has helped to save lives. The infusion of the SAMHSA grant funding received, in partnership with our Wellstar Foundation, will further enhance our reach and impact to the individuals in this vulnerable population,” says Trisha Velasco, assistant vice president of the Behavioral Health service line.
Wellstar's receipt of the SAMHSA grant builds on the system's established infrastructure through the provision of additional educational resources to healthcare clinicians and the community. It also increases access to evidence-based treatments shown to reduce suicidal thoughts. Specifically, funding will enable follow-up care for high-risk adults who are struggling with suicidal thoughts and/or have experienced a recent suicide attempt. Through this grant, SAMHSA aims to aid the program in continuing to reduce suicide ideation, suicide attempts, and deaths due to suicide.
This grant's objectives align with Wellstar's goals of reducing suicide attempts and suicide death rates among Georgians ages 18 and older by growing the existing Wellstar Zero Suicide Initiative. Adding community-based and treatment-focused strategies, including suicide prevention training throughout the organization coupled with identification, treatment, and care transition, Wellstar will continue strengthening the community. At least 5,000 patients across six Wellstar hospitals and emergency departments will receive care, including to residents in Bartow, Cherokee, Cobb, Douglas, Forsyth, Fulton, Harris, Paulding, Polk, and Troup counties.
Suicide is a leading cause of death in the United States, affecting people of all ages. While mental health plays a role, there are many other factors that may lead someone to contemplate suicide, and there are some warning signs to pay close attention to because they may indicate that someone is at risk of suicide, which include:
The research is clear that enhancing feelings of belonging and connection is a powerful method of reducing suicidal thoughts and behaviors. While suicide can be a difficult topic to talk about, speaking about it non-judgmentally can offer hope. In contrast, avoiding the discussion can contribute to feelings of isolation, further contributing to devastating outcomes.
If you suspect a loved one is at risk for suicide, talk with them. Here are some tips to help guide your conversation:

Mary Chatman, Executive Vice President of Acute Care Operations for Wellstar Health System, Elected Chair of the Georgia Hospital Association Board of Trustees
ATLANTA – Mary Chatman, PhD, RN, executive vice president (EVP) of Acute Care Operations for Wellstar Health System, was elected chair of the Board of Trustees of the Georgia Hospital Association (GHA) earlier this month. Chatman, who has served on the GHA Board since February 2020, will lead the Board in developing strategies for GHA hospital members, advocating for the highest quality care for patients, and supporting adequate reimbursement for hospitals.
“Mary Chatman’s extensive leadership experience and skills make her well-equipped to lead our Board,” said GHA President and CEO Caylee Noggle. “She is a strong patient advocate, and her experience will serve our members well.”
Serving as a Wellstar EVP, Chatman oversees the operations of Wellstar’s 11 hospitals, post-acute services, and emergency departments. In 2020, she led the opening of Wellstar Kennestone Regional Medical Center’s new emergency department, the largest in the Southeast.
Prior to serving in her current role, Chatman was the chief operating officer and chief nursing officer at Memorial Health University Medical Center in Savannah, where she was responsible for managing the 654-bed hospital and its nursing operations. She also served as interim chief information officer for Memorial and completed the electronic health record conversion to EPIC.
In 2021, Gov. Brian Kemp appointed Chatman to the state’s Healthcare Workforce Commission, where she has helped address challenges in the hiring and retention of health care workers.
Chatman has been recognized locally and nationally as a prominent leader and strong patient advocate in health care. Atlanta Daily World recognized her among the 2018 Women of Excellence. Diversity MBA Magazine named her among the 2018 Top 100 Under 50 Executive & Emerging Leaders and 2020 Top 100 Women of Influence. Profiles in Diversity Journal named her a 2020 Women Worth Watching® in STEM award winner. Chatman was recognized by Atlanta Magazine among the 2021 Women Making A Mark honorees and by Becker’s as one of the 75 Black Healthcare Leaders to Know 2022. She was also named the 2020 West Cobb Citizen of the Year for serving on the frontlines for Cobb County, fighting COVID-19, and collaborating with local leaders.
Chatman is deeply involved in the community, serving as board member for United Community Bank and active in the fight to find a cure for type 1 diabetes. She is a member of the American Nurses Association and the American College of Healthcare Executives. She earned her Bachelor of Science, Master of Science, and Doctor of Philosophy degrees from East Carolina University in Greenville, North Carolina.
About GHA Founded in 1929, GHA serves nearly 150 hospitals in Georgia and promotes the health and welfare of the public through the development of better hospital care for all Georgia’s citizens. The mission of GHA is to advance the health of individuals and communities by serving as the leading advocate for all Georgia hospitals and health care systems. GHA represents its members before the General Assembly and Congress, as well as state and federal regulatory agencies, and is an allied member of the American Hospital Association. For more information, please call 770-249-4500 or visit gha.org.

Wellstar Primary Care Providers: Partners in Your Care
Are you getting the most out of your healthcare experience? If you don’t have an established Wellstar primary care provider (PCP), you could be missing out on some major benefits.
Some people visit a different provider each time they need a check-up or just whenever they feel sick. Similarly, many patients use the walk-in convenience of urgent care as a substitute for primary care. However, in both of these cases, it can be difficult for you to build a lasting health partnership and leave your care feeling incomplete.
Having a designated Wellstar primary care provider—and specialty medicine providers within the same health system—gives you an entire team of health experts that are invested in you and your well-being.
The main role of a primary care provider is to keep you healthy at every age and stage of life. To keep you feeling your best, these experts are trained to:
As you get older, your healthcare needs will change. That’s why many people keep the same Wellstar primary care provider for years, even decades.
Your provider can help you stay ahead of health issues and deliver tailored care for your unique needs, as they change over time. These experts are your first defense against many preventable diseases and can catch major illnesses earlier, so you have the best possible outcome.
Ready to find the right Wellstar primary care provider for you? We make it easy to get expert, comprehensive primary care at many convenient locations across metro Atlanta and West Georgia. To find a location near you, simply click “Book Now” at the top of any page.

Give Yourself the Gift of Health
Between cookie baking, busy shopping trips and being with family, the holiday season can pass by in a blur. Through all the hustle and bustle, Wellstar health experts warn it can be all too easy to put off your wellness.
“During this hectic time of year, health may be the last thing on your mind. However, the best present you can give yourself is prioritizing your well-being,” said Dr. Umme Nur, internal medicine physician with Wellstar.
“Seeing your provider now can help you stay on track this season,” Dr. Nur explained. “It can also help you jumpstart your health goals in January and already have a care plan tailored to your needs.”
It’s easy to let your normal routines slip during this time of year. However, you can take small steps to stay on track every day.
Remember, the perfect gift isn’t something wrapped with a bow—it’s putting your health first. That means partnering with Wellstar Primary Care and scheduling a wellness exam.
Your primary care team will help you take charge of your health and create a personalized plan just for you. Because your clinician is a pro at preventative care, they’ll help keep you ahead of potential medical problems.
After your annual check-up, you’ll know your stats for:
At your exam, be sure to bring up any health goals, such as weight loss or managing a chronic condition. Your care team will work with you to create a custom treatment plan for your unique needs.
Depending on your gender, age and family history, your care team may also recommend other preventative tests to screen for diseases before they start, such as a mammogram or colonoscopy.
Your clinician can also help you understand your potential health risks with:
Learn more about how having an established primary care team can keep you well.

Holiday Blues: Why the Holidays Can Sometimes be More Stressful Than Joyful
The holidays can be challenging, especially for those struggling with mental health. Familial factors, unrealistic expectations, past trauma, and grief/loss can all play a role in why sometimes the holidays can be more stressful than joyful.
Physical and behavioral health outcomes are intertwined and provide a holistic view of our health. Physicians refer to assessing depression as “a vital sign” -- like checking blood pressure and heart rate. Considering the assessment of depression is essential for a person’s overall health status.
With nearly one in five Georgians struggling with mental illness yearly, treating mental health conditions and assessing suicide risk is a group effort between health professionals and state, local, and community partners. Wellstar’s director of adult & pediatric primary care behavioral health integration, Dr. Janna Williams-Pitts, helps us to understand why the holidays can be so stressful.
“When the stress response becomes activated due to something we are excited or concerned about, it can have a physiological and psychological impact. This occurs for those with and without a diagnosed mental health condition. The stress response, and more specifically chronic stress, can play a role in the onset of a depressive episode or the recurrence of heightened anxiety symptoms.”
Women are about twice as likely as men to be diagnosed with an anxiety disorder. In speaking with Dr. Williams-Pitts, we wanted to understand how specific risk factors like age and gender can make facing these holiday stressors more challenging.
“Research suggests that there are gender differences in the stress response due to biological factors, specifically hormonal differences. Women appear to be more likely to experience depression due to chronic stress, whereas men may be more likely to develop substance use disorders due to chronic stress. The APA completed a survey to assess for Stress in America in 2022. The results of this survey indicate that inflation, concerns about violence, and the racial climate in America are a few of the factors that contribute to differing experiences with stress for participants. Age differences emerged as well. Forty-six percent of adults under 35 reported feeling so stressed that it impacted their functioning whereas 42% of adults aged 35-44, 16% 45-64, and 4% of adults 65+ reported the same.”
People respond to stress in a variety of ways. Often, individuals can hide their symptoms from those closest to them. But we learned there are signs to look for in loved ones who might be experiencing stress blues during the holidays. Social withdrawal, increased substance use, change in hygiene/self-care, shifts in sleep, and experiencing feeling anxious, overwhelmed, and poor concentration can all be signs that chronic stress is starting to have an impact.
It's common for people to notice increased fatigue and feeling down due to less exposure to sunlight during the winter months. So, it’s only natural to wonder if environmental changes during winter months play a role in the onset of depression.
“Some people experience debilitating depressive episodes during the fall and winter months with significant improvement in the spring and summer months. When depressive episodes occur in a seasonal pattern, this is consistent with the diagnosis of Seasonal Affective Disorder.”
Dr. Williams-Pitts added that it is “important to identify a range of meaningful, enjoyable activities to engage in during the winter months to help reduce the likelihood of worsening depressive symptoms.”
Rescheduling appointments with your behavioral health clinician before the holidays can be tempting. Still, keeping that appointment is helpful for those who experience stress during this season. It serves as an opportunity to review your stress management plan and identify meaningful coping mechanisms, which may help the holiday season go more smoothly.
If you are wondering where to turn if you need help during the holidays but don’t have a behavioral health clinician, scheduling an appointment with your primary care provider can be a great way to connect with a behavioral health clinician.

Wellstar Supports Developing Future Healthcare Professionals at Cobb Innovation Technology Academy
According to the American Hospital Association, “Shortages of health care workers in all roles will persist well beyond the pandemic given today’s highly competitive labor market.” To help meet this need, the Cobb County School District and Wellstar Health System are introducing high school students to healthcare careers through the healthcare pathway at the Cobb Innovation Technology Academy (CITA). CITA is an innovative Career, Technical, and Agricultural Education (CTAE) program inside the Cobb County School District (CCSD).
Wellstar Health System and Wellstar Foundation recently awarded Cobb Schools Foundation a $2 million grant to expand the Cobb Innovation and Technical Academy (CITA) over the next five years. The CITA program is a beacon of opportunity for students seeking hands-on learning experiences and career prospects in healthcare through district, post-secondary and industry partnerships.
"This program seeks to inspire, educate, and nurture the next generation of healthcare professionals,” said David Jones, Executive Vice President and Chief Human Resources Officer for Wellstar. “We’re thrilled with the opportunity to help enhance the education of our community’s students and offer them rewarding career pathways."
Cobb students will have direct access to healthcare professionals from Wellstar who will make their classroom experience more practical and prepare them for their real-world jobs. All CCSD students can apply for the opportunity to enroll in CITA. Once enrolled, the Cobb students will be able to:
"The Wellstar Healthcare Pathways Program will offer students exposure to training and potential job opportunities,” said Tiffany Barney, Director, CITA. “The Cobb Schools Foundation appreciates this investment in students who will go on to have careers in healthcare. It will further enhance the quality of education we provide our students in Cobb."

New Sarcoidosis Clinic at Wellstar MCG Health Helps Diagnose, Treat Patients Living with Little-Known Disease
It’s taken three years and several hospitalizations, but Dianne George finally knows what’s wrong with her heart, and it’s not one of the usual ailments.
She has sarcoidosis.
The condition is often missed partly because symptoms are not obvious, and partly because many physicians don’t know about it. Sarcoidosis is an inflammatory disease that causes clumps of immune cells, called granulomas, to form in tissues and organs.
“We don’t know what triggers it, and we don’t understand why certain people get it and are more susceptible to it,” said Dr. Neal Weintraub, Division Chief of Cardiology and Professor of Medicine at Augusta University’s Medical College of Georgia. “It’s most common in Black people, and it’s also very common in Scandinavia.”
It can affect almost any organ, though the lungs are most commonly involved.
For George, the granulomas form in her heart. With conditions involving the heart, the first symptom might be sudden death.
That’s one thing that makes George’s case unique: She’s here to tell her story.
“It all started in June of 2019,” she said. “I was a teacher, and I walked the neighborhood during the summer, in the morning. That summer, I started walking but I would get out of breath, dizzy and stuff.”
On her way to Edisto Beach for a trip with her husband, she joked that at least she had never passed out.
“Probably 20 minutes later, after saying that, I passed out in the car,” George said. “Harry tried to find my pulse and he couldn’t find it. I recovered fairly quickly, but I didn’t feel right.”
They went to a nearby prompt care clinic, which sent George to a local hospital because, while her blood pressure was good, her heart rate was off. She received a pacemaker and assumed that her problems were solved.
In November 2019, George started having ventricular tachycardia—her heart was beating very fast and weakly. Her cardiologist in Aiken, where she lives, sent her to Wellstar MCG Health Medical Center. She was placed on medical therapy and her pacemaker was changed to a CRT-D device, which has a defibrillator that shocks the heart to restore a regular heartbeat rhythm.
George began receiving repeated shocks from her device and was readmitted to the hospital the following month. Weintraub became involved in her care and almost immediately suspected the culprit could be sarcoidosis. He ordered several tests, including a PET scan and bronchoscopy with a biopsy, which confirmed the diagnosis.
Weintraub prescribed several medications designed to treat inflammation, as well as heart medications. George’s heart rhythm calmed down almost immediately and her heart function recovered.
Cardiac sarcoidosis can become very serious if left untreated, Weintraub said. Besides dangerous arrhythmias, patients like George could present with heart failure with no obvious cause such as blocked arteries to explain it.
“The problem is a lot of physicians are not aware of cardiac sarcoidosis at all. Even many cardiologists don’t think about it. Since they don’t think about it, they can’t make the diagnosis,” he said. “If you have cardiac sarcoidosis and proper treatment is not given, the prognosis is dismal. Most people that have untreated cardiac sarcoidosis will be dead within a few years.”
Sarcoidosis is very common in the Southeast, and that is one of the reasons Weintraub and his colleagues have established the Sarcoidosis Clinic at Wellstar MCG Health. Not only is the disease very serious with potentially life-threatening consequences and can be difficult to diagnose, but a diagnosis also typically requires advanced imaging capabilities that aren’t always available—especially in smaller communities.
“So we felt that here at Wellstar MCG Health, we were in exactly the right place and have the right people and resources to bring together to form this clinic so that we can serve the region,” Weintraub said.
When a patient comes to the clinic, they see a cardiologist, a pulmonologist and a rheumatologist who all have expertise in sarcoidosis. The cardiologist and pulmonologist investigate problems with the heart and lungs, and the rheumatologist investigates problems with the joints (another common site for the disease). The rheumatologist can also initiate medications that help suppress the immune system, which is an important part of treatment. The team will refer the patient to an ophthalmologist or dermatologist if eye or skin involvement is suspected. Each patient also receives follow-up care to ensure that the inflammation is controlled and medications are tightly monitored.
“The patient can come to one clinic and see three different physicians who all share their expertise and come up with the best plan for diagnosis, treatment and follow-up,” Weintraub said.
George credits Weintraub and the rest of her care team for her ability to continue doing the things she enjoys, although in a more limited capacity. She travels with her husband, cares for her granddaughters and stays active in her church through careful management of her symptoms.
“And I can share my story,” she said. “It’s not a death sentence, by any stretch of the imagination. You just have go to about things in a little different way.”
Wellstar MCG Health recently joined 42 other institutions as a member of the Foundation for Sarcoidosis Research Global Sarcoidosis Clinic Alliance.

Jace Dion Undergoes Multiple Surgeries at Children's Hospital of Georgia to Repair Cleft Lip and Cleft Palate
Amanda Dion had her heart set on having a girl. After three boys, she was very excited when her doctor told her, based on an early sonogram, that she would finally have one.
Another sonogram a few weeks later told a different story. Not only was she having a boy, but the image showed something concerning. He would have a cleft lip.
“My ultrasound tech was taking more time this time, measuring more,” Dion said. “I’m like, ‘What’s going on?’ She said, ‘We’ll just wait until the doctor comes in.’ About that time, I see her go across his face and you could see his cleft lip in the picture on the screen.”
That wasn’t all. Her doctor sat her down and explained that not only would her baby boy, Jace, have a cleft lip, but he might have a cleft palate. There was also an abnormality in his brain, which was eventually diagnosed as Dandy-Walker syndrome.
Dandy-Walker is a brain malformation that affects coordination. In many children, the condition causes hydrocephalus, in which fluid in the brain doesn’t drain properly. These children often have a large head size and slow motor development.
No one would know how the condition would affect Jace until he grew and began to develop, Dion said.
However, the staff at Wellstar Children’s Hospital of Georgia stepped in to not only deliver Jace early—Dion was borderline preeclamptic and had a c-section at 37 weeks—but also treat Jace and help ensure he lives a healthy, normal life.
Jace spent the first few days of his life in the hospital’s neonatal intensive care unit (NICU) on extracorporeal membrane oxygenation (ECMO). Once he was stable, he was able to go home with oxygen and a feeding tube, but the battles were just beginning. Jace developed pneumonia, needed several sets of ear tubes and had a shunt in his liver repaired. He also had heart surgery to correct a congenital heart defect.
As he grew, Jace had a difficult time eating due to a laryngeal cleft.
“It can cause aspiration, which can make it hard for babies to gain weight and stay well,” said Dr. Heather Koehn, a pediatric otolaryngologist at Wellstar Children’s and assistant professor of pediatric otolaryngology at Augusta University’s Medical College of Georgia.
Jace required a feeding tube and frequently had tubes put in his ears. Koehn explained that children with a cleft palate also tend to have frequent ear infections. Swallowing helps us pop our ears, releasing fluid and ventilating the ear.
“If your palate isn’t born with the muscles connected, then the whole mechanism doesn’t function properly,” Koehn said. “Then you’re not able to ventilate the ears through the Eustachian tubes. The ears end up accumulating thick mucus, and then that fluid is like being underwater all the time. So a child can’t hear clearly, and it puts them at risk of speech delay and other learning delays.”
Jace’s neurologists continue to monitor his Dandy-Walker symptoms, which, thankfully, are not severe. He also sees a team of speech therapists, physical therapists and occupational therapists every other week.
Now 4, Jace is an active boy who loves dinosaurs, playing with his brothers and swimming.
“It took us a long time to get him there, but he’s definitely in a good spot,” Dion said. “He’s definitely super resilient—bounces back from everything.”

KathyCare
Kathy DeJoseph delights in making and giving away thousands of soft and cheerful hats to Wellstar cancer patients through a nonprofit she founded called Happy Caps. It’s all in the name of bringing a little light and comfort to people during a hard time.
Where did the idea come from? It started with Kathy’s own lung cancer diagnosis.
A cancer survivor for more than a decade, Kathy said regular lung cancer screenings were the key to her survival. With a long history of smoking and growing up around relatives who smoked, she decided to join an early detection lung cancer study at Wellstar.
Even though she felt fine and had no symptoms, committing to the study meant having an annual low-dose CT scan every year. After several years of clean scans with no signs of lung cancer, Kathy told a nurse that she was going to quit. But the nurse persuaded her to come in for another screening.
“Thank goodness she did,” Kathy said. “I was diagnosed the very next day.”
Being a part of the study and getting screened early allowed Kathy to move immediately to Wellstar Lung Cancer STAT Clinic at Wellstar Kennestone Regional Medical Center.
STAT stands for Specialty Teams and Treatment, highlighting the collaboration of multiple cancer experts. Together, they come to a consensus on a treatment plan and meet with the patient on the same day. This puts the patients at the center of their care plan, allowing them and their families to get immediate answers to questions, make decisions and start treatment faster.
“The biggest benefit for me with the way the STAT Clinic works is that I didn’t have to worry about whether the doctors had actually talked to each other,” Kathy said. “They’d come in one after another and tell me what they thought from their expertise.”
Immediate communication and mutual agreement among medical experts mean treatment plans are established and started faster, which is proven to improve long-term survival. On average, it takes 60 to 90 days from the time of diagnosis to treatment in the U.S. With the STAT Clinic at Wellstar, patients go from diagnosis to treatment in 14 to 20 days.
Kathy’s treatment started quickly—she had a lung biopsy the day after her STAT Clinic appointment and started chemotherapy a week later.
“I wasn’t as terrified for as long as most people are because I had answers within a short period of time,” Kathy remembered.
She had surgery once she completed chemotherapy. Throughout the process, she had the support of an entire cancer team, including a medical oncologist, a lung cancer surgeon, a pulmonologist and a nurse navigator.
How research and faster time to treatment are progressing cancer care
Republished Content: Atlanta Business Chronicle
This article was originally published on Atlanta Business Chronicle on November 3, 2023.
As cancer research advances, doctors know more about the keys to reducing cancer cases and driving better outcomes, like long-term survival. Prevention, early detection and treatment—an area that has drastically improved through scientific discovery—are the big three keys today. While preventative measures reduce the risk, screening for cancer before someone has symptoms can be a lifesaver when it is identified earlier and in more treatable stages. Newer, more advanced treatments and starting treatment faster are also making a sizeable impact on survival. For a closer look at how healthcare experts apply these keys in the fight against cancer, Atlanta Business Chronicle’s Market President and Publisher David Rubinger sat down with Wellstar leaders and patients for a sponsored panel discussion on the state of cancer care.
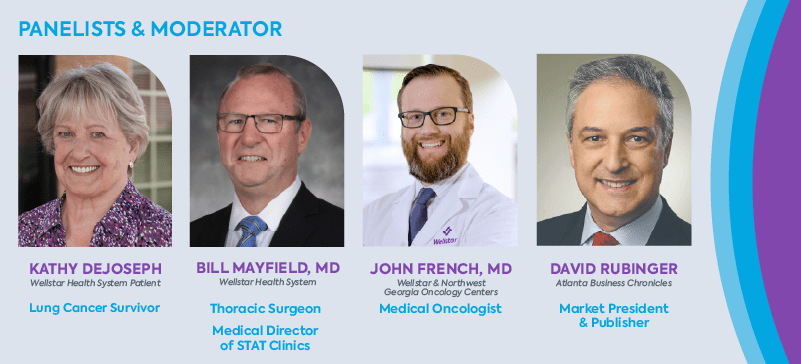
*Wellstar partners with Northwest Georgia Oncology Centers to provide world class cancer care close to home.
David Rubinger: Cancer is one of the top causes of death in the U.S., second only to heart disease, with 1.9 million new cancer diagnoses expected this year. The whole idea of trying to beat cancer is the common language of treatment now. We’ve really changed the conversation in many ways. Dr. Mayfield, what have been the keys to getting these better survival rates across all types of cancers?
Dr. Bill Mayfield: There are three basic components to improving outcomes and reducing cancer. Number one is prevention. How can you prevent cancer? Smoking cessation is a major way to reduce the risk for cancer, especially lung cancer. The second key is early detection screening for cancer such as colonoscopies, skin exams and low dose lung cancer CT scans.
Finally, we have treatment as the third key. We have dramatically improved treatments, especially in the last 10 years, with targeted therapies, immune therapies and precisely targeted radiation therapy. For some cancers, reducing the time it takes to start treatment can be as impactful as some of the newer cancer therapies. At Wellstar, we speed up time to treatment through our STAT Clinics.
Rubinger: Dr. French, from the medical oncology standpoint, what has specifically gone on in your world since you started practicing medicine that you think has improved these outcomes?
Dr. John French: There’s no bigger story than immunotherapy in the last 10 years. It was 2017 when Jim Allison out of the University of Texas MD Anderson Cancer Center and Tasuku Honjo in Japan won the Nobel Prize for cancer immunotherapy—the first time the Nobel in Medicine recognized a cancer therapy in decades. Wellstar and our patients participated in clinical trial development of immunotherapy for various cancers.
In medical oncology, there are also targeted therapies. In improving the survival and outcomes of patients, we do a lot of what we call next generation sequencing—tumor genomics and tumor DNA. The way I explain this is, “We’re not testing Kathy’s DNA. We’re testing the tumor itself. We are trying to find a lock and key mechanism, where if we can find what’s driving the cancer, maybe there’s a pill or a target that we can go after to take it out.”
Rubinger: Let’s move on to lung cancer in particular. Lung cancer has traditionally been known as a smoker’s disease—at least that’s how many people view it. It appears as though in the United States we’ve seen an improvement in terms of the number of lung cancer cases. Dr. Mayfield, where is the lung cancer discussion right now? I feel it was maybe one of these small victories that are going on in the cancer movement.
Dr. Mayfield: We do actually have some large victories. The surgeon general came out with a report in the 1960s that said smoking caused premature death and lung cancer. Men in Georgia started reducing their smoking about 35 years ago. As a result, we have 50% fewer male smokers and 35 years later, we’re now seeing a 50% reduction in primary lung cancers from tobacco.
Rubinger: As far as I understand it, early lung cancer is one of those cancers that has no outward physical markers that tell you you’ve got something going wrong. So as lung cancer specialists, what do you advise people to do when they’re getting their checkup? What is the process by which they should be screening for lung cancer?
Dr. French: The biggest thing you can do is if you’re smoking, stop smoking and get screened if you’re eligible. Dr. Mayfield discussed that already, but I’ll add some numbers and perspective.
Number two, if you were a smoker, understand the guidelines and recommendations to undergo screening. They updated the guidelines in 2021 that if your age is 50 to 80 and you have a 20 or more pack per year history of smoking, and currently smoke or quit within the past 15 years, then you’re eligible for screening.
By having a CT scan, you can reduce the risk of lung cancer death by up to 20% by identifying and treating cancer earlier.
Rubinger: Let’s talk to a lung cancer patient about this. Kathy, thank you for joining us. Take us briefly through your journey. What is your background with cancer?
Kathy DeJoseph: This year, I’m a 12-year survivor. Before I was diagnosed, I was a career person and I was on my computer one day and up popped information about this early lung cancer screening study that Wellstar was a part of. I had no symptoms. I had a long history of smoking, grew up with parents who smoked, grandparents who smoked, lived near a factory that was belching out junk into the air.
I was a workaholic and a mom and I saw this study and for whatever reason, I called and talked to the nurse navigator. I was like, “I don’t know whether I want to do this or not. You know, this sounds like I’m going to end up paranoid about it.” She encouraged me to participate.
Dr. Mayfield: Kathy was enrolled in the study and had three or four normal CT scans before she developed a mass. And sure enough, we jumped right on it through Lung Cancer STAT Clinic and got her treatment plan together quickly. That was the point of her being in the annual screening study.
Rubinger: Kathy, before we dive further into your treatment, will Dr. Mayfield help define the STAT Clinic? It’s not a simple thing to do. You all are very busy people and you all have individual schedules. To turn you all into this sort of troop, if you will, moving in sync, that’s a logistical nightmare for a bunch of doctors.
Dr. Mayfield: STAT stands for Specialty Teams and Treatments and it’s about bringing multiple cancer experts together to collaborate about a patient’s care and meet with them the same day so they can get treatment started quickly. We created STAT because we saw a need to do things better and to put the patient at the center of everything we do.
About 17 years ago, we opened a general Thoracic Surgery practice at Wellstar Kennestone Regional Medical Center. And we did everything like everybody else did. We had a navigator—someone who connects a person who has cancer with the help and support they need. We had tumor boards—a group of physicians and scientists who meet to discuss treatment options for individual cancer patients.
But when we looked carefully, we saw that by the time the patient’s case was presented in a tumor board, it was 58 days on average from the time the patient had their original CT scan. They had gone from a primary care doctor to a pulmonologist to an oncologist back to the pulmonologist, then had a biopsy, a PET scan and then maybe saw a radiation oncologist. It was 58 days by the time they got to the tumor board and were able to get a treatment plan started. That’s a problem. But that is the standard of care in the United States today—60 to 90 days in this workup period.
We said, “There’s got to be another way.” I knew of a clinic run by a pretty notable oncologist in another state, who brought the thoracic surgeons, pulmonologists and the oncologist to his clinic to see the patient at the same time. An oncologist and I drove up there, spent the day, asked a bunch of questions and said, “You know what, we need to do this.”
So we came back and getting those specialists—the thoracic surgeon, pulmonologist, medical oncologist, radiation oncologist and navigator—in the same place at the same time was hard.
What we decided to do is start with one hour on Wednesday afternoon. So we saw two patients one week, then 2 to 3 the next week and then 3 to 4 the next week. Then a primary care doctor heard about it and the pulmonologists heard about it and suddenly we were seeing 12, 15, 20 patients.
A few years ago we surpassed more than 10,000 patient visits in the Lung Cancer STAT Clinic. And during that time, we started the lung screening program and the incidental nodule program.
The culmination of our initiatives to identify lung cancer earlier and hasten the time to treatment has reduced our time from abnormal image to starting treatment to somewhere between 14 and 20 days, rather than 60 to 90 days. The early detection program has made it such that 40% of the cancers diagnosed at Wellstar are stage 1 and 2, when cancer is more treatable and patients have better outcomes. On a national average, just 15 to 20% of lung cancer diagnoses are stage 1 or 2. We’ve dramatically improved the ability of our lung cancer patients in our community to survive their disease.
Rubinger: It sounds like early detection and shorter time to start treatment make a real impact for patients. Kathy, let’s talk a little bit about what those things meant for you as a patient. Let’s start with when you were diagnosed. Did you have any symptoms? What happened next?
DeJoseph: I didn’t have any symptoms. Everything was fine, except for my history with smoking. The year I was diagnosed, I was going to quit the study but the nurse navigator took me out to lunch to convince me to come back—and thank goodness she did. I was diagnosed the very next day.
The biggest benefit for me with the way the STAT Clinic works is that I didn’t have to worry about whether the doctors had actually talked to each other. I didn’t have to worry about whether maybe they didn’t actually agree. All those things that I would have been worried about went away because I talked to all of them on the same day in the same place.
It gives you a lot of confidence. I thought, “Well, you know, they’d have to all be wrong on the same day at the same time to screw this up.” I ended up becoming a volunteer and would meet with newly diagnosed patients for several years. One of the biggest things that I would talk to new patients about is how STAT Clinic kept things from dragging out for months, going from doctor to doctor.
Rubinger: It sounds like STAT Clinic is meaningful to patients, not just medically, but emotionally. Is the STAT Clinic exclusively for people with lung cancer or are patients with other conditions benefitting from this model now?
Dr. Mayfield: That’s a good question. We added Lung Cancer STAT Clinics at Wellstar Cobb, Douglas and North Fulton Medical Centers. Outside of lung cancer, my neurosurgery buddy got curious. He’s saying, “Wait a minute. You know, we have this patient with brain cancer and they have to go see the radiation oncologist but your patient gets to meet the radiation oncologist at the same time as you. We want that.”
So the next STAT Clinic that cranked up was for neurological tumors. It was awesome to see that we could inspire other folks to do the same thing.
Dr. French: To add to that, we also have STAT clinics for breast cancer and head and neck cancer. All of these cancers require multidisciplinary care with doctors from different specialties who collaborate on patient care because otherwise, you have to go see different cancer subspecialists and that may take a longer period of time.
Dr. Mayfield: Here’s the dark secret about cancer care in the U.S. Dr. Alok Khorana at the Cleveland Clinic published a paper about three years ago. He studied 1.2 million cases in the national cancer database and 340,000 of those were lung cancer patients. He clearly showed that for every seven days’ delay in therapy in stage 1 or stage 2 disease, you lose 2% five-year survival. Delay in time to initial cancer treatment in the U.S. is an important risk factor for survival over time.
Rubinger: Kathy, let’s come back to you for a second. So you go into this STAT Clinic. Obviously, this whole process must have been terrifying on so many different fronts.
DeJoseph: I wasn’t as terrified for as long as most people are because I had answers within a short period of time.
Rubinger: How short?
DeJoseph: I had my biopsy the next morning after the first STAT Clinic appointment. About a week and a half after that, I started chemo. That was really fast. I had surgery after chemo.
In the STAT Clinic, every doctor comes in and talks to you. You learn what their role is going to be and what the timing will be with other treatments. It all happens at the same time. I took a lot of confidence in questioning everybody on the same day and knowing they had also talked together. I knew for sure that they had, where I would have really wondered about that if had I done it the normal way—visiting multiple specialists over a several-month period.
Rubinger: I’ll be the contrarian for a second. What if I walk into the STAT Clinic and say, “Well, I’d like to choose my surgeon. I’d like to choose my oncologist. I’d like to choose the radiation oncologist I want to use for my radiation treatment.” How much flexibility do I have within the STAT Clinic to select the doctor I want to work with? Or do I have to take the ones that are assigned to me regardless?
Dr. Mayfield: That is an excellent question. You can come to us for a consolidated opinion and get your care wherever you choose. You have four experts looking at you physically and reviewing all your imaging and all your tests together, coming to a consensus. For treatment, you can use any oncologist, any thoracic surgeon, anybody you want, even if it’s within our own institution.
Dr. French: Whether we’re providing the care or simply an opinion, STAT Clinic puts the patient first. We have patients from Alabama, Tennessee, North Georgia who can’t travel here for ongoing care. I’ve even had patients who live near the Carolina border. Part of the STAT Clinic is also handling the logistics where one of these patients may need treatment closer to home. For example, someone may need chemotherapy and I say, “OK, I’ll coordinate that with the medical oncologist in your area.” When we’re done seeing STAT Clinic patients, we agree, “You call the local radiation oncologist, I’ll call the local medical oncologist and let’s get them plugged in and connected with treatment recommendations.” Again, STAT Clinic expedites and coordinates all that care. Getting the foot in the door and getting that ball rolling is half the battle.
Dr. French: In talking about screening earlier, we didn’t address non-smokers. If I don’t smoke, I don’t need to be screened if I’m doing my well check-up and I’m not having a cough or chest pain. There’s really no screening for lung cancer outside of those recommendations.
That being said, the other thing that you need to understand is that in the state of Georgia, we are horrible at screening people. We rank toward the bottom quartile of the entire country in screening patients when it comes to the proportion of eligible patients. The American Lung Association data ranks Georgia 35th in the nation. We screen 5% of eligible people, so we’re not capturing 95% of people who could be screened.
We know the data to support screening is there. Kathy is a living example of this. Talk to your primary care doctor about your history with smoking and the need for screening.
Dr. Mayfield has ramped up the effort to capture more at-risk people through screening, but we still need to get the message out.
Dr. Mayfield: We started our screening program 15 years ago as part of I-ELCAP—the International Early Lung Cancer Action Project—and then we broke off of the study because the results were so positive. We decided we’re just going to do this as a standalone program in our community.
As a result, over the last 15 years, we become one of the three largest lung cancer screening programs in the U.S. We have about 15,000 people in our program currently.
The problem is, we serve a community of 1.7 million in 15 counties. Knowing that 40% of those are smokers or former smokers, we should be scanning a million people a year.
Why aren’t we screening more people? We’re a part of the Georgia Lung Cancer Roundtable and the National Lung Cancer Roundtable trying to solve that problem. I think it’s going to take a national awareness campaign.
When that happens, we need to prepare our screening centers for high volumes. That will drive us from discovering more stage 3 and 4 lung cancers when people are dying, to finding more stage 1 and 2 lung cancers. Those earlier-stage cancers are much less expensive to treat from a policy and population health level and are easier to treat, giving more patients good long-term outcomes.
Rubinger: But we wouldn’t be screening non-smokers at this point.
Dr. Mayfield: There’s not enough data yet to guide us to any other risk factor than tobacco use.
Rubinger: Let’s talk about the business community for a second.
When it comes to the employee, when you see patients who are in full-time jobs, what role do you see the employer playing when you’re caring for cancer patients? What can employers do to help them in their battles?
Dr. Mayfield: I have a pretty strong opinion on two items. One is that employers should promote age-appropriate screenings for all cancers among their employees. Give them that half a day off if they need to go somewhere for a doctor’s appointment to get that screening exam. And as callous as it may seem, that half a day off to find cancer in earlier stages is much less expensive than treating an advanced cancer years later, from extended time off to the insurance costs associated with advanced cancer.
The CEO of the corporation, the vice president, the chief medical officer, the chief operating officer—they assume that if they or any of their employees get cancer care, they’re going to get the best care available. But unfortunately, the best care available today in most places is going to take them 60 to 90 days to get through the initial doctors’ visits and tests that at the STAT Clinic, we manage in 14 days.
My challenge to the business community is to ask their insurers and their healthcare providers a very difficult question, “How long will it take to get our employee from an abnormal finding to starting treatment?” When insurers and healthcare providers have to start answering hard questions, then we’ll move the ball.
Dr. French: I would add, when a corporation buys health insurance, it needs to make sure institutions that perform research and clinical trials are covered.
I had a patient who had stage 4 prostate cancer and there is a clinical trial using novel bispecific immunotherapeutics. The guy is young; he’s eligible for the trial. The patient signed the trial consent only to find out that his insurance doesn’t cover the medical facility that’s offering it, so therefore he’s not eligible for the clinical trial. Now he’s going to have to get the standard of care, which is good. But he could have gotten something new on a trial if it was covered by his company’s health plan.
So, companies should first make sure that employees are covered for good quality healthcare and at top facilities that perform research.
Number two is, if you’re an executive, consider supporting on-site screening. I’ve seen a lot of patients in the STAT Clinic who get executive physicals, they get a day off and they do this comprehensive testing. Lo and behold it shows something. That early detection gets them to treatment at an earlier stage when the cancer is less advanced and they have a higher chance for better outcomes.
So consider offering a half-day, a health fair or on-site health screenings as part of your company’s health offerings.
I think a healthy employee, one that feels valued and respected, will be a hard worker. If I feel that my business cares about me, my health, my life and my family, that sounds like a company I’d want to work for.
Learn more about cancer care at Wellstar.

Wellstar Clinical Partners Medicare ACO Continues to Significantly Reduce Costs for Patients
The Centers for Medicare & Medicaid Services (CMS) announced the 2022 results for the Medicare Shared Savings Program (MSSP) and Wellstar Clinical Partners (WCP) Medicare Accountable Care Organization (ACO) helped CMS save over $16 million for the entire performance year.
“These latest results from CMS clearly demonstrate how Wellstar is committed to providing world-class care for every person, every time. Our teams never waiver from that commitment – even during some of the most challenging times in healthcare,” said Dr. Alan Muster, senior vice president, Specialty Division for Wellstar Medical Group. Dr. Larry Hornsby, chairman of the board for WCP added, “At Wellstar, we all work together to keep our communities healthy. We provide the highest-quality care, at an appropriate cost, and ensure each patient has an exceptional experience while maintaining a laser focus on our caregiver well-being.”
Even after CMS revised its methodology for calculating the annual Quality score, Wellstar maintained a competitive rating compared to other Georgia systems that participate in the Medicare ACO. The System also saw an increase in patient satisfaction compared to 2021. The WCP Medicare ACO performed in the top 16 percent of ACOs for 2022 based on generated savings, out of more than 480 other ACOs.
“The health and well-being of every patient remain our top priority,” said Barbara Corey, president of the Wellstar Clinical Partners Medicare ACO. “The hard work and dedication of our WCP physicians is clearly reflected in our latest accomplishments, and we are proud of the compassionate care we consistently provide for the communities we serve.”
As one of the largest and most experienced ACOs in Georgia, the WCP Medicare ACO is consistently named one of the top ACOs in the country. Additionally, the ACO is the only one in Georgia to help Medicare bend the healthcare cost curve for nine of the last ten years. Medicare Shared Savings Program (MSSP) ACOs are groups of doctors, hospitals, and other healthcare providers who come together voluntarily to provide coordinated high-quality care to their Medicare patients.
The WCP Medicare ACO leverages its internal resources, infrastructure, and partnerships with employed and affiliated physicians to deliver high quality, cost-effective healthcare to the communities it serves. Since 2012, the WCP Medicare ACO has been a consistent, high-quality, top performing ACO and it is among the top MSSP ACOs when measured by cumulative savings to Medicare of nearly $150 Million.

Wellstar Lung Cancer Screening Detects 500 Cancers Since 2008

Wellstar Offering Saturday Hours for Lung Cancer Screening November 11
Lung cancer screening can detect cancer earlier, before symptoms show up. Earlier-stage cancers are more easily treatable and more frequently cured, so if you are at increased risk of developing lung cancer, you could benefit from regular low-dose CT scans to monitor your lung health. To expand access to these vital screenings, Wellstar will offer screenings at several imaging locations on Saturday, November 11.
“Lung screening improves a person’s chances of detecting a lung cancer at an early stage and being cured of that cancer,” said Wellstar Thoracic Surgeon Dr. William Mayfield.
Wellstar is partnering with the National Lung Cancer Roundtable, established by the American Cancer Society, the American College of Radiology, the GO2 Foundation for Lung Cancer and the Radiology Healthy Equity Coalition to celebrate National Lung Cancer Screening Day on November 11. While lung scans are always available at our conveniently located imaging centers during regular business hours, offering these Saturday hours will help patients fit screenings into their schedules.
Ask your provider about whether you meet the criteria for screening, or call (470) 793-4AIR (4247) to learn more about qualifying and to make an appointment for a scan. The following Wellstar imaging locations will be open Saturday, November 11:
In addition to these special hours on November 11, low-dose CT lung scans are available at several Wellstar imaging locations. Call (470) 793-4AIR (4247) to learn more or schedule a screening.

Monitoring Your Lung Health with Cancer Screenings
Lung cancer screening can detect cancer earlier—even before symptoms show up. Earlier-stage cancers are more easily treatable. If you are at increased risk of developing lung cancer, you could benefit from regular low-dose CT scans to monitor your lung health.
“Finding lung cancer early leads to better outcomes, and screening with CT scans is recommended as the only proven way to minimize delay in diagnosis,” said Wellstar Thoracic Surgeon Dr. Daniel Fortes.
Our team has built one of the country’s largest and most comprehensive screening programs. Wellstar has been designated as a Screening Center of Excellence and Care Continuum Center of Excellence by the GO2 Foundation, an organization that supports lung cancer patients and educates about screenings and care. We’re also a designated Lung Cancer Screening Center by the American College of Radiology.
The United States Preventive Services Task Force has revised lung screening guidelines. You may qualify for screening if you are 50 to 80 years old and smoked for 20 years. If you are a former smoker, you may qualify if you quit less than 15 years ago.
“Those who are current or past smokers of cigarettes are more likely to develop lung cancer,” Dr. Fortes said. “However, while smoking is the leading risk factor for lung cancer, a large number of lung cancer patients have never smoked—1 in 5 women and 1 in 10 men diagnosed with lung cancer were never smokers.”
You may also be at increased risk of developing lung cancer if you have been exposed to radon, asbestos or other agents such as uranium or arsenic, according to the American Cancer Society. Previous radiation therapy in the lung area, such as chest radiation for breast cancer treatment, can also increase risk. Additionally, be sure to discuss your family history with your provider—siblings and children of people who have had lung cancer may have a higher risk of developing it.
Screening for lung cancer is not a one-time test, but a process that involves a periodic evaluation of your lungs over time to look for newly emerging cancer. CT scans can detect nodules that are compared over time for changes in size.
“For those who are at high risk for lung cancer, it is best to have nodules and lung health evaluated by a team of physicians specializing in lung cancer care so the appropriate decision can be made of continued observation versus the need for early intervention,” Dr. Fortes said.
Depending on the findings, some patients may have more or fewer exams. If findings are suspicious for lung cancer, your care team will contact you to discuss your screening results.
An order from your physician is required to get a screening. Contact your primary care team or a pulmonologist to talk about screening and when it may be right for you. Once an order has been obtained from your physician, call (470) 793-4AIR (4247) to schedule your appointment.
Your care team will support you at every step of the screening process. If you have any questions about your results or your screening plan, contact your provider over the phone or using the secure messaging feature in MyChart. You can also call our cancer care team at (877) 366-6032 to learn about our care options.
All lung screenings are initially interpreted by a radiologist. A team of physicians who specialize in the diagnosis and treatment of lung cancer will review findings that are suspicious for cancer. Once the physicians complete their review of your images, your results are posted within three to five days to your MyChart account. Results will be communicated with you and your physician via MyChart or mail within one week.
If a lung cancer is suspected, our team will call you to answer your questions and arrange next steps. You will then meet with a physician specializing in lung cancer treatment.
Patients whose screening shows a lung nodule may feel concerned. However, you should not be overly concerned if your report indicates you have small lung nodules. Most people who meet eligibility for screening will have some. Nodules are very common—at least 50% of people have them by the time they are 50 years old.
Learn more at wellstar.org/lungcancer.

Pediatric Patients Trick-Or-Treat at Wellstar Children’s Hospital of Georgia
Little superheroes, princesses and witches who spent their Halloween at Wellstar Children’s Hospital of Georgia did not miss out on the fun. Wearing costumes donated by the community, patients enjoyed trick-or-treating by visiting units along the halls of the children’s hospital. Wellstar MCG Health Medical Center employees dressed up as well and handed out goodies from their decorated stations.
A few members of the Child Life Specialists team who were dressed as crayons—including facility dogs Casey and Nugget—pulled wagons filled with treat bags to trick-or-treat for patients who were too ill to walk the halls themselves.
Child Life Specialists work hard to ensure that pediatric patients can still be kids, even in the hospital. But they can’t do it alone. Each community member who donated costumes and each employee who participated and provided treats made the holiday a little brighter for these patients.

Meet new Wellstar MCG Health President Ralph Turner
Ralph Turner stepped out the front door of his new apartment in North Augusta and ran into his neighbor, who had a Wellstar MCG Health Medical Center badge.
“I work there too,” he said. “Oh, what do you do there?” she asked.
He held out his badge that read “president,” and she looked up in shock.
“There are so many medical students and Wellstar employees in my complex,” he said. “The hospital is such a large part of the community.”
Turner, who has lived out of a hotel in Augusta until last week, still considers Powder Springs his permanent base. He drives to Augusta on Sunday afternoon and back to Atlanta on Thursday night to spend Friday at Wellstar Paulding Medical Center. Saturday is his rest day to enjoy with his wife of 31 years, Ann.
The new leader started his career in 1986 with the U.S. Army, giving him the chance to live around the world—Fort Bliss, Texas; Fort Cavazos, Texas (formerly Fort Hood); Fort Belvoir, Va.; Fort Johnson, La. (formerly Fort Polk); Fitzsimons Army Medical Center in Aurora, Co.; Germany; Alaska; Washington, D.C.; and Seoul, South Korea.
From the start, he knew he wanted to work in healthcare.
“It’s rewarding to help people when they are at their most vulnerable state,” he said. “To me, there is honor in that.”
After graduating from high school in Valdosta, Ga., he joined the Army and took a job repairing hospital equipment. After eight years, he became a warrant officer—a highly respected position for subject matter experts who make up less than 3% of the Army—and began managing clinical engineering departments in hospitals.
At the same time, Turner was taking classes. He earned his bachelor’s degree in 1995, going on to earn a master’s in public administration and then a master’s in healthcare administration.
“My mindset is be all you can be,” he said.
The more senior he became, the more departments he managed. His last assignment for the Army was at the Walter Reed Army Medical Center in Washington, D.C., where he ran support services departments such as property management, environmental services and clinical engineering for facilities. After more than two decades in the Army, he retired in 2008 as a Chief Warrant Officer Four (CW4) and earned an executive position with MedStar Washington Hospital Center as an assistant vice president of facilities and support services.
Turner departed Washington, D.C., for Wisconsin to work at the University of Wisconsin Hospitals and Clinics and thought he was finished with school after three degrees. But when his oldest son began to talk about going to medical school, his competitive side came out. He returned to school at the University of Wisconsin and earned his doctorate in business administration.
“I thought, ‘He’s not going to be the first one in the family to be called a doctor,'” he said in good humor.
From there, he moved his family to Cleveland, where he joined the Cleveland Clinic for two years. He then transferred to Florida for three years for his role as chief operating officer, overseeing a merger between the Cleveland Clinic and Indian River Medical Center in Vero Beach.
Turner’s journey with Wellstar began in May 2022 when he became president of Wellstar Paulding Medical Center in Hiram, Ga. He is now the first president of Wellstar MCG Health in Augusta.
We sat down with Turner last week, and he answered some questions to help the staff and community get to know him and his vision for the future of Wellstar MCG Health.
What’s your day-to-day like right now at Wellstar MCG Health?
Right now, I’m usually at the gym between 5 and 5:30 AM, and then in the office between 7 and 7:30 AM. My day usually ends between 7 and 7:30 PM. If I am not in a meeting, my door is always open. I have an open-door policy. I usually have anywhere from 80 to 100 emails at the end of the day, and I make sure to go through all of them before I leave at night.
What made you want to go into hospital management?
I have always liked helping people, and I knew going into healthcare, you’re doing just that. In high school in Valdosta, we had the South Georgia Medical Center and my plan was to end up there. My father passed when I was 4 so my mother, my grandmother and my godmother raised me. Those three women always told me to treat people the way that I wanted to be treated, and if I got caught not doing that, they always reminded me with a stick, broom or whatever they got their hands on. Needless to say, I quickly learned the Golden Rule and apply that to every area of my life—professional and personal.
What’s the biggest area of improvement you’re working on here?
First, ensuring people are paid fairly. Our Human Resources at the main campus is focused on putting together a comprehensive plan that will start to bring our caregivers to a market-compatible salary. You must make sure you do the right thing for your staff, because that’s the most important resource you have. Second, ensuring that our facility looks like it’s a place of healing. Third, ensuring physicians are supported and strengthening our medical services lines in the market. Smart and efficient growth of our physician staff and service lines lead to market domination, which leads to a stronger training center at our medical school. Fourth, community initiatives—getting out into the community and meeting community leaders to let them know we are here to support them. Fifth, ensuring a good relationship with leadership at Augusta University. And, lastly, protecting our assets. When I say our assets, this includes students in their didactic phase of learning and students in their residency or fellowship. We want to be our students’ first choice when it comes to choosing an employer. We want them to stay with Wellstar, be it here in Augusta or in the Atlanta area. We have a lot of students who come from other universities in and out of the state. My thought is, let’s feed ourselves first and go to outside resources for talent second.
Can you talk more about what improvements you’re planning in regard to facilities?
In our Wellstar Children’s Hospital of Georgia lobby, the only realistic lobby entrance we have, there are a few issues to address. There’s an old water fountain that hasn’t had water in it in 15 years; there’s furniture that was supposed to be antimicrobial and is no longer antimicrobial; there are cracks in the floors near the Chick-fil-A; windows haven’t been washed in eight years; and the bottom is coming off the reception station. It’s not that the team didn’t want to address the issues; it’s that they just didn’t have the capital. Our facility professionals managed a budget of $250,000 to take care of a 2.9-million-gross-square-foot facility. If you have one HVAC go out, there goes all of it. So it’s empowering people. People want to do their job, but they’ve been handcuffed with a budget. I told them, “Just do it.”
What’s the biggest threat to the industry?
A lack of human resources and the cost of healthcare. We have to figure out how to close the gap between the amount that healthcare organizations pay to provide care versus what we get reimbursed for providing the care because we pass a lot of that cost onto the patient.
How is the difficult labor market impacting Wellstar?
Certain hospitals are better than others. I think across our system, our vacancy rate for nurses is about 18%, but at Wellstar Paulding Medical Center, our vacancy rate is about 7.8%. At some of our other hospitals, I think they average anywhere from 18% to 24% vacancy.
What do you anticipate being the biggest challenge of Wellstar partnering with an academic medical center?
Academia focuses on the teaching mission, which may lack the urgency to maximize volumes in our ambulatory clinics, which could lead to low volumes/clinic appointments on a daily basis, in comparison to the amount of staff and available exam rooms.
I need to ensure academia understands our mission, “To enhance the health and well-being of every person we serve.” This means we must ensure we are utilizing every opportunity to maximize our ability to see patients by filling schedules and ensuring we have enough support and operational staff to facilitate safe and efficient operations of our inpatient units and ambulatory clinics. We want to earn as much revenue as possible so we can reinvest it back into our organization by providing better salaries, improving our equipment and improving our facilities.
Where is Wellstar MCG Health now and where do you want it to be?
According to U.S. News & World Report, the Medical College of Georgia ranks 79th nationally in the best medical schools for research. I want us to be ranked in the top 50 in five years, and the top 15 in 10 years. I want to make sure that we become the premier medical school not only in the state of Georgia but also in the U.S. I want us to be able to compete with medical schools like Duke and Emory. I want us to be in the top two to three schools in our region.
What are our strengths and weaknesses? I think one of our biggest strengths is our people. Our team members have true care and concern for people. This is demonstrated daily. A weakness would be the time we have to invest to become fully integrated into Wellstar. It’s a weakness because we can’t come out of the starting blocks moving at a fast speed, driving changes immediately. We are looking at three to five years before we are fully integrated into Wellstar. It takes time to implement the new IT programs and systems that will tie us into Wellstar, which will provide us the opportunity to be more nimble and agile in implementing changes.
Is there anything you want the work-family to know? We feel the most important resource we have is our human resources. I want every leader we have to engage with their staff and to understand what they need to do their job because I will ask every leader. As president, it’s my job to make sure our team members come to work in an environment that’s safe, free from coercion and free from harassment. It’s also my job to make sure they have what they need to do their job, so they don’t feel like they’re handicapped. And if anyone ever feels like they don’t have what they need to do their job or that they are being coerced, harassed or feel unsafe, please let me know directly. Remember, I have an open-door policy. Final thought: Always put the patient first. That’s what we’re here for, to take care of people who cannot take care of themselves at a specific moment in time. If our team members are making decisions with the mindset of putting the patient first, I always have their back.
Do you have a quote you live by? Just do it (Nike). Eighty percent solution is better than 100% analysis paralysis at any time. When you have 80% of the solution figured out, go ahead and start moving the needle. Just do it.

A Gift From the Heart for Patients with Breast Cancer Across the CSRA
It all started with a gift and a special note.
April Sather had just undergone surgery for her breast cancer and was struggling to sleep at night. She would spend the night tossing and turning, trying to get comfortable. “I’m a side sleeper, so that is kind of an issue,” she said when describing her sleeping troubles.
One day she received a gift from a friend: a heart-shaped pillow made with soft flannel that was light pink with beautiful clouds across it. Sather was able to tuck it under her arm and sleep comfortably throughout the night. This gift, combined with a lovely note from one of her nurses after surgery, inspired Sather to want to do the same for others.
“I thought, ‘Wouldn’t it be cool if we could make heart-shaped pillows for other breast cancer patients so that after they get out of surgery, they could feel that same love that I received?’” Sather said. “I shared the idea with a few ladies at church, and the rest is history.”
Healing Hearts Ministry at Warren Belvedere Church now meets once a month to sew, stuff, pray, write notes and package up the hearts to be delivered to patients with breast cancer across the CSRA. There is no commitment, and volunteers are welcome to take the materials with them if they prefer to work in the comfort of their own homes.
“It makes me feel like I’ve done something that’s worthy of helping someone else go through a hard time in their life,” volunteer Susan Elliot shared about each time the group finishes a pillow to be delivered to a patient.
Elliot is one of the women who answered Sather’s call for help with her idea. While she has no personal experience with breast cancer, she is a seamstress and was more than happy to use her knowledge and experience with sewing for the program.
Healing Hearts provides the sewing pattern, fabric and fluff needed to create the pillows, so all that volunteers have to bring are their hands and good spirits. Sometimes the group welcomes speakers during the meetings; in fact, they celebrated their first anniversary by inviting a Wellstar Georgia Cancer Center patient and breast team nurse navigator to come and share their story.
If you would like more information or to make a donation to assist the program, visit the church’s website, select the Belvedere campus, then make the message out to April Sather or Susan Elliot. You can also get in touch through the church’s Facebook page.

TamekaCare
Tameka Pearson experienced the best and the worst of women’s health in a decade. When she overcame her first health challenges, a new breast cancer diagnosis tested her again. As Tameka conquered cancer with the support of her family and her Wellstar cancer care team, she only grew fiercer in her dedication to self care.
Look back a decade and you’ll see Tameka, a mom of three, teaching middle school students. She started out as a special education teacher, then became an English and language arts teacher. She said, “I truly loved trying to figure out how to help the students learn the curriculum in a different way and to help them cope with their disabilities.”
She was also coping with her own issues at the same time—fibroids, heavy bleeding and pain. After five years, she had a hysterectomy and went through menopause at 36 years old. It took a year to recover, and she gained 60 pounds, high blood pressure, anxiety and depression.
“The heaviest I could lift was my clothes basket,” she remembered. “When I got clearance to exercise, I changed my eating habits, my mindset and my life for the better.”
A new focus on building strength shaped her into a new woman—inside and out. She rose at 4 AM daily, lifted weights, taught students and returned home for time with her family.
In peak physical condition at 43 years, Tameka scheduled her routine annual mammogram. She got called back for a second mammogram due to dense breast tissue.
“Getting a call back after a screening mammogram means that the doctor wants to look at something more closely,” said Diane Harris, RN, a certified oncology nurse navigator at Wellstar Douglas Medical Center. “It does not mean you have cancer, but if you do, finding it earlier could save your life.”
But for Tameka, further imaging led to more tests and finally, a needle-guided biopsy. Two days later, she got a call confirming she had triple negative breast cancer. She said, “I felt like this little bump can pretty much dictate the rest of my life. When I heard the term ‘breast cancer,’ my world stopped. I cried for about two weeks straight.”
What to Expect When You or a Loved One Are Diagnosed with Breast Cancer
Breasts play an important role when it comes to a woman’s health, yes, but often they’re an important part of a woman’s identity, sexuality and function too. With 1 in 8 American women developing breast cancer in their lifetime, the disease affects many people physically and emotionally.
In this article, a patient and a group of breast experts discuss the best ways to prevent and fight breast cancer, as well as how to support family members, friends, colleagues or neighbors who may be diagnosed.

Tameka Pearson, breast cancer survivor: When I was diagnosed, I just went to pieces. I cried for about two weeks straight. There were tears in my eyes when I’d wake up. I didn’t want to eat or go outside. I had to process the information. I was getting phone calls—updates and making appointments. But I was still a mom and a wife and had to go to work. That was a lot.
When I was a child, my mom would say, ‘Pick yourself up and dust yourself off and get moving.’ I gave myself permission to mourn for two weeks—permission to loathe, to cry, to get it out of my system. Once those two weeks were over, I was done crying—done feeling sorry for me. I picked myself up and persevered. I realized I have a lot to live for! I couldn’t give up.
Before breast cancer, I did everything for my family—cooking cleaning, washing clothes. When I was diagnosed, they immediately took over. They became more independent, especially my children. My husband became more of the provider and caretaker. My children were like, ‘Mom, we need you to sit down; we need you to rest.’
One of my coworkers from the past is also a survivor and started a group called Lean On Me. When I logged onto a Lean On Me Breast Cancer Network Zoom meeting, I loved it. They were uplifting, prayerful and gave me great information if I had questions.
Margie Apacible-Mancao, MSN, RN, CBCN, nurse navigator: After the initial shock of diagnosis, it’s not uncommon to get depressed or anxious. There can be the stress of transportation, childcare if they have young children at home or financial concerns. Sometimes patients experience anxiety for the first time, sometimes they’ve had it in the past and being diagnosed brings it to the front. We can connect them to counselors, financial counselors and social workers, or they can join a support group. Meeting with other patients and survivors helps them know they are not alone, get through treatment with hope and form great friendships. We live in a society where we’re trained to be independent, but when I meet with patients, I say, ‘Allow yourself to receive help.’
Dr. Karen Xu, MD, radiation oncologist: In general, radiation treatment for breast cancer is very well tolerated and most women go through the treatment without much difficulty. The most common side effects are fatigue and skin irritation appearing as a sunburn-like reaction from radiation treatment. We see patients at least once a week during radiation treatment and we recommend different creams depending on how severe the skin radiation reaction is. Mild physical activity usually helps with fatigue.
Dr. Sujatha Hariharan, MD, medical oncologist: One of the initial concerns patients have when they start chemotherapy is potential hair loss. This can be devastating and disheartening. We are excited to now offer cool caps as a means to reduce hair loss from chemotherapy. Cool caps work by cooling the scalp, leading to constriction of blood vessels in the scalp. This might reduce the amount of chemotherapy that reaches the hair follicles leading to reduced hair loss from the head. The success rate of the cool cap can vary from person to person.
There is a vast cancer support network available through Wellstar. Aside from the doctors, patients have support from social workers, chaplains, dietitians, nurses and nurse navigators. A whole team of people is here to help patients through the process. Patients often meet other patients during treatment where they bond and support one another. This can be such a meaningful and valuable relationship.
The main thing is you’re not going to be alone. Many people will be here to help you with all aspects of your care.

Halloween 2023: Trick-or-TREAT and Play it Safe
Halloween is right around the corner, and while many Georgians are planning to celebrate this year, many may have questions about how to do so safely.
Wellstar’s very own Dr. Branstetter recently shared his recommendations to minimize the risk from the triple-demic and to keep family and friends safe while celebrating holiday occasions such as Halloween by ensuring you are up to date with the latest vaccines that help prepare our immune systems to prevent illnesses.
"Some of my patients have already elected to get both their COVID and influenza shots. I don't think there is a perfect way that we need to go through and get these vaccines. The important thing is, if they're indicated for you and you're due for a vaccine, go ahead and get those done." - Dr. Danny Branstetter, Medical Director for Infection Prevention at Wellstar Health System in the Marietta Daily Journal
Millions of people in the U.S. and around the globe, including children of all ages, look forward to the festivities of Halloween. But–lest we forget–it's virus season, and RSV, flu, and COVID-19 are still lurking in the shadows. How can we celebrate while keeping our families, friends, and neighbors safe from the community spread of these viruses, which is essential to everyone's health and well-being? Get creative and think about safety. Think "TREAT!"
Wellstar has created these tips for a healthy Halloween celebration while keeping in mind it's a holiday full of tricks and TREATS!
Wellstar is committed to providing high-quality, tailored and compassionate care. For more information and the latest updates on COVID-19, visit wellstar.org/COVID-19.
A Candid Talk About Your Breasts
Over the years, advice about breast self-exams and breast cancer screenings has changed. So what exactly should you be doing to make sure you’re staying your healthiest? We brought together a panel of women’s health experts to discuss the best strategies to keep tabs on your breast health—and who to talk to if you’re diagnosed with breast cancer.

Dr. Paula Greaves, MD, OBGYN, Wellstar chief Women's Health officer: Unfortunately, 1 in 8 women will develop breast cancer in their lifetime, so early detection is key. We have shown over the years that the sooner we detect breast cancer, the more successfully it can be treated. Survival has increased significantly since we started finding breast cancer earlier—before there are symptoms, such as feeling a lump during a self-exam.
Mammograms are essential for early detection. It’s recommended that women start getting mammograms at age 40. However, if you have a family history of breast cancer or other risk factors, your gynecologist or primary care provider may recommend starting earlier and will help you create a personalized screening plan. There are some risk factors that women cannot change, such as genetics, but there are some ways women can lower their risk, like quitting smoking, eating a healthy diet and exercising regularly. Wellstar offers 16 mammography locations, and our patients have state-of-the-art technology on their side. We offer high-resolution breast screening, including 3D mammograms.
Women should continue not only getting annual mammograms, but also seeing their gynecologist or primary care provider for regular breast exams. Women should also be aware of physical changes within their bodies, including breast changes. Changes in the texture of the skin or a lump or pain in the breast should always be checked out by their healthcare provider.
Margie Apacible-Mancao, MSN, RN, CBCN, nurse navigator: I am so passionate about breast cancer screening—every opportunity I have I tell patients to get a screening mammogram when they’re of age. Tell someone in your circle that you’re going, then they’ll tell someone in their circle and the circle gets wider so more people will get screened.
Dr. Sujatha Hariharan, MD, medical oncologist: When a mammogram detects an abnormality, a biopsy might be indicated. Many breast biopsies will be non-cancerous such as fibroadenomas.
If cancer is found on a breast biopsy, there are several parts of the pathology result that the care team will utilize to make a treatment plan. For example, the presence of estrogen and progesterone receptor positivity allows the potential for hormone therapy as part of the treatment plan. The HER-2 gene is also tested for and if that is present and positive, it allows for medication directed at the HER-2 gene to be given along with chemotherapy.
Sequencing of the various treatments for breast cancer—surgery, chemotherapy, radiation and hormone therapy—will be determined as a collaborative effort between the breast surgeon and medical oncologist.
Margie: The anxiety of not knowing their diagnosis or what’s next is one of the hardest parts. At Wellstar, patients have access to a nurse navigator on the day they are recommended to have a biopsy. We make an appointment with the specialists as quickly as possible because just knowing that someone is helping them get to the next step and get that appointment fast dials down their stress level.
Dr. Karen Xu, MD, radiation oncologist: If you are diagnosed with breast cancer, you will need to see a breast surgeon first to discuss your surgery options—lumpectomy or mastectomy; a radiation oncologist to discuss the duration of radiation treatment and whether lymph nodes should be included in the target; and a medical oncologist about whether endocrine therapy or chemotherapy is indicated and the timing of systemic therapy. Patients who desire reconstruction after mastectomy will discuss with a plastic surgeon the type and timing of reconstruction they want.
Find a breast imaging location near you online or call (678) 581-5900.

Wellstar Health System Recognized by the American Medical Association for Promoting Well-Being of Healthcare Workers
The American Medical Association’s (AMA) Joy in Medicine™ Health System Recognition Program has recognized Wellstar Health System for its commitment to improving physician well-being and reducing burnout among healthcare clinicians. Wellstar is Georgia’s first large health system to receive this distinction.
Prior to 2020, burnout rates among U.S. physicians and other healthcare professionals were rising, but the prevalence spiked dramatically as the COVID-19 pandemic placed acute stress on care teams and exacerbated longstanding system issues. While the worst days of the pandemic have passed, the lingering impact of work-related burnout remains an obstacle to achieving national health goals.
“From our President and CEO Candice L. Saunders to our physician leaders and executive team, this recognition is a meaningful testament to the commitment that our physician and other Wellstar leaders have made to our people,” said Dr. Ryan Breshears, a clinical health psychologist, Wellstar’s chief behavioral health officer, and chair of Workforce Well-being. “The road ahead is long, and by no means does this suggest that our work is finished, but it’s encouraging that the AMA has validated that we’re trending in the right direction.”
When it comes to clinician well-being, elevating the voice of the practicing clinician is paramount. In April 2022, Wellstar’s Clinician Resiliency and Well-being team developed a cross-specialty Physician Well-being Council to identify opportunities to mitigate stress drivers and support physicians and other clinicians in prioritizing their health and well-being. Employing a multi-pronged approach aligned with best practice models, Wellstar has implemented the assessment of clinician well-being annually, developed avenues to build camaraderie, and made improvements to reduce administrative burdens on the clinical workforce. July 2023 data revealed that Wellstar’s prevalence of physician distress has declined by 29% over the past two years and that overall physician well-being is 15% better than the national average during the same timeframe. Following rigorous analysis, these changes proved statistically significant on both accounts.
“Health organizations that have earned recognition from the AMA’s Joy in Medicine Health System Recognition Program are leading a national movement that has declared the well-being of health professionals to be an essential element for providing high-quality care to patients, families, and communities,” said AMA President Jesse M. Ehrenfeld, MD, MPH. “Each recognized organization is distinguished as among the nation’s best at creating a culture of wellness that makes a difference in the lives of clinical care teams.”
"The goal of the Joy in Medicine Health System Recognition Program is to unite the healthcare community in building a nationwide culture committed to the well-being of clinical care teams by helping health organizations invest in action plans promoting professional fulfillment and meaning that clinicians find in caring for their patients,” said Christine Sinsky, MD, AMA vice president of professional satisfaction.
Since its inception in 2019, the Joy in Medicine™ Health System Recognition Program has recognized more than 100 organizations across the country. In 2023, 72 health systems nationwide earned recognition with documented efforts to reduce system-level drivers of work-related burnout and demonstrated competencies in commitment, assessment, leadership, efficiency of practice environment, teamwork, and support.
Learn more about the AMA Joy in Medicine™ Health System Recognition Program at ama-assn.org/joyinmedicine.

Six Steps to Reduce Your Cancer Risk
By Wellstar Urologist Dr. Beau Dusseault
By Wellstar Urologist Dr. Beau Dusseault
When seeking medical advice, many people turn to the internet. This wealth of information can be very helpful in uncovering the cause of common symptoms and providing general health tips. In fact, patients play an essential role on their healthcare team. However, many people fall into the online vortex of diets and vitamins while leaving the low-hanging fruit on the vine.
Here are six quick tips to reduce your risk of cancer:
Whatever is good for the immune system is bad for cancer. Lifestyle choices are the foundation for any cancer prevention program. And the internet would agree—just in case you want a second opinion.
Wellstar offers screenings and care for several types of cancer, and our urologists are experts in prostate cancer care. With a simple blood test, we can screen for prostate cancer. Learn more about prostate cancer screening.
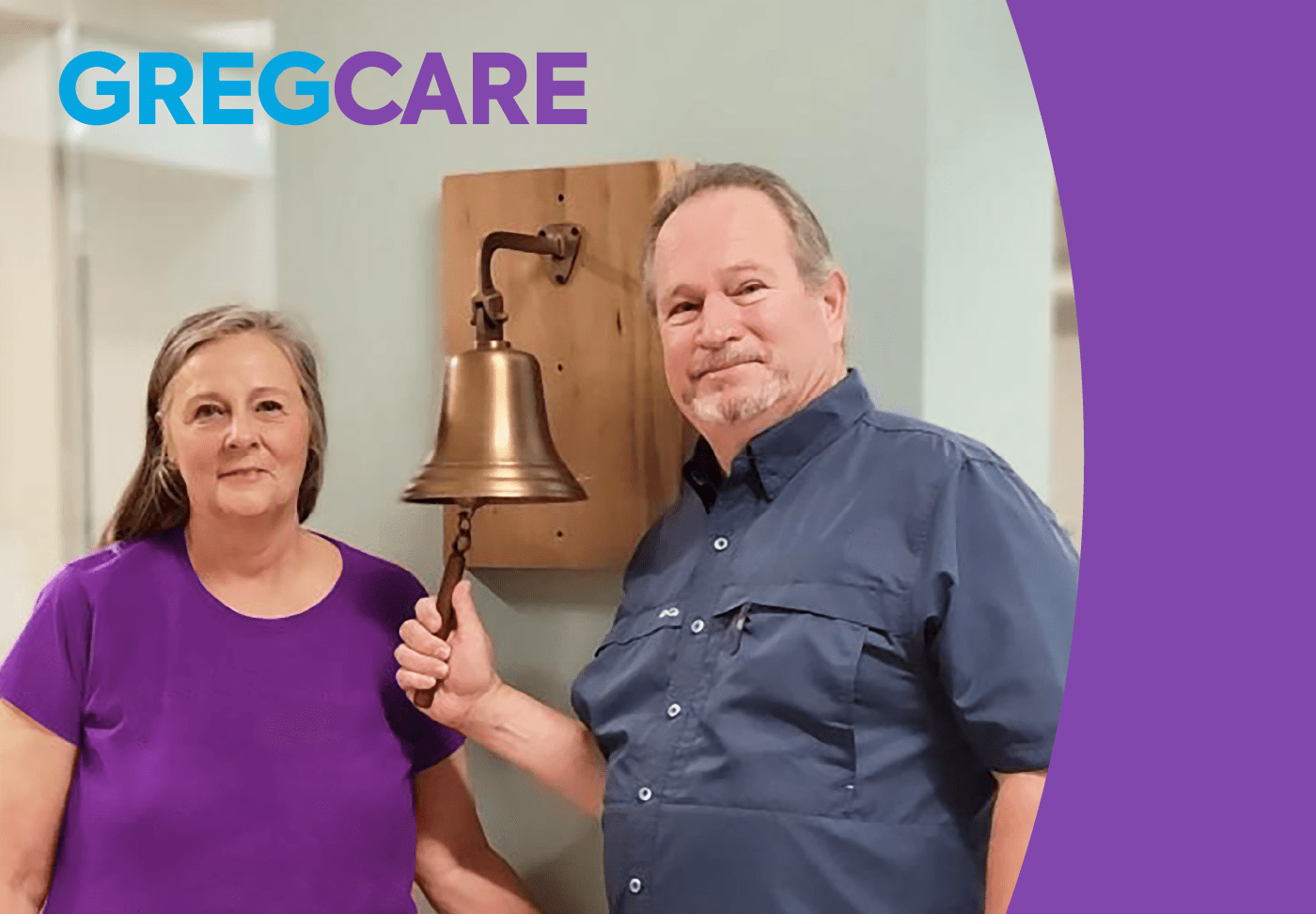
GregCare

What Women Should Know About Prostate Cancer
By Wellstar Urologist Dr. Reena Kabaria
By Wellstar Urologist Dr. Reena Kabaria
Most women don’t spend much time thinking about prostate cancer until someone they know is touched by this disease. Prostate cancer is the most common cancer in men and the second most common cause of cancer death in men. If a woman’s loved one is diagnosed with prostate cancer, here is some guidance she can use to stay informed and support them throughout their cancer care.
The prostate is an organ tucked away under a man’s bladder. The sole purpose of the prostate is to produce the fluid needed for reproduction. Although the prostate serves no other role, it is surrounded by several delicate structures responsible for urinary and other sexual functions.
Fortunately, recent advances in the treatment of prostate cancer usually allow men to keep sexual and urinary functions intact. In fact, early detection not only increases the likelihood of cure, but also minimizes the chances for side effects. At the most curable stage, prostate cancer does not usually cause any symptoms. Therefore, men aged 40 and above should ask their doctor when they should have a screening PSA blood test based on their individual needs and risks.
Many men with a new diagnosis have such a slow-growing form of prostate cancer that it can merely be observed over time. When exploring different treatment options, it's recommended that patients consult with both a urologist and a radiation oncologist.
Wellstar surrounds patients with compassionate care. Nurse navigators provide a highly personalized level of support and guidance throughout diagnosis, treatment and follow-up care. We also offer support groups if patients want to meet others who are dealing with the same diagnosis. While a cancer diagnosis is often upsetting and overwhelming for both patients and the people they love, our team stands with patients and families at every step.

Advancements in Prostate Cancer Diagnosis and Treatment Give Providers and Patients New Tools
By Wellstar Urologist Dr. Justin Watson
By Wellstar Urologist Dr. Justin Watson
Many men are reluctant to seek diagnosis and treatment of prostate cancer because they fear the effects of treatment on their urinary and sexual function. Enter modern technology. MRI scans, PET scans and molecular testing of blood and tissue samples not only help physicians know how and where to treat, but also identify those who may not need any treatment.
Having a PSA blood test is usually the first step in detecting prostate cancer. Now, modern MRI scans can help the urologist target abnormal areas for biopsy, like how a GPS pinpoints a destination. With this technique, patients can be more confident that the biopsy samples accurately represent their condition. In fact, this confidence has allowed men with slow-growing forms of prostate cancer to observe their condition rather than immediately pursue treatment. Since the formation of cancer cells all starts with changes in a cell’s genetic material, specialized testing of the biopsy sample can help further define the behavior of an individual’s prostate cancer.
When treatment for prostate cancer is needed, the latest methods bring next-level precision to protect the delicate nerves and muscles surrounding the prostate. Now in its second decade as a standard treatment for prostate cancer, robotic prostate removal continues to break barriers with new instrumentation, refined techniques and artificial intelligence. Not only do these advancements speed up recovery, but they also facilitate less traumatic access to spaces that were previously very difficult to reach. Similarly, the latest radiation therapy techniques allow delivery of a thin beam to the prostate.
For more aggressive forms of prostate cancer, the latest type of PET scan can identify the cancer in other locations. First, a radiotracer (slightly radioactive substance) is injected into a vein, and it binds to prostate cancer cells, wherever they may be hiding. Then the resulting X-ray images are superimposed onto a CT scan to highlight any areas of suspicion. We can now attach medications to this radiotracer to attack and kill remote prostate cancer cells like a guided missile.
With these recent advancements in technology, the management of prostate cancer continues to be more effective and gentler for the modern man. One can only imagine what’s on the horizon.
Learn how to support a loved one through their prostate cancer diagnosis.

CatchItEarlyCare
When it comes to diagnosing breast cancer, time is of the essence.
That’s why Wellstar uses state-of-the-art imaging technology to help identify cancer sooner, so we can treat it faster. Getting a screening mammogram can save your life, so don’t delay.
“The earlier we detect a breast cancer, the better we are able to treat it,” said Dr. Paula Greaves, Wellstar Chief of Women’s Health.
With 14 imaging centers offering mammography, it's easy to find one that's convenient to you.
If you do not have any risk factors that increase your chance of developing breast cancer, you should start annual screening mammograms at age 40.
If you’re at higher risk for breast cancer, your provider may recommend you start screenings earlier and can help you create a personalized plan.
“Being female at birth gives you a 1 in 8 chance of developing breast cancer, but there are other components that can increase that risk,” Dr. Greaves said.
You may be at higher risk of developing breast cancer if:
Wellstar offers several locations to get a mammogram. Call (678) 581-5900 to schedule yours. You can also ask your Wellstar provider to put your mammogram order in MyChart and you'll be able to schedule the test online.
A mammogram uses low dose X-rays to examine the breast for abnormalities and signs of cancer. Wellstar offers 3D mammograms, which provide a series of detailed images of the breast, allowing healthcare providers to better evaluate breast tissue layer by layer. In these images, fine details are more visible as compared to 2D mammograms and are no longer hidden by overlapping tissue.
The mammography unit is a rectangular box that houses the X-ray tubes and special accessories so that only the breasts are exposed to radiation. Attached to the unit is a device that holds and compresses the breast and positions it so images can be taken from several angles.
The technologist is with you throughout the procedure and will ensure that the necessary images have been taken before completing the exam.
Once you have completed a mammogram, you may resume your normal, everyday activities.
If your screening mammogram results are normal, your next mammogram will be the following year, unless your provider recommends more frequent screenings due to family history or other risk factors. Continue to perform breast self-exams monthly, and if you notice any changes such as a lump, sore spot or a difference in the appearance of the skin, contact your provider.
When a mammogram result is flagged for follow-up care, it can be scary and intimidating for patients and their loved ones—but at Wellstar, you won’t have to navigate your health journey alone.
As you search for answers about your breast health, the Wellstar Comprehensive Breast Health Program and its complimentary concierge services will make your experience more seamless with a tailored care plan, advocacy for your physical and emotional well-being, dedicated team members for scheduling appointments and education about your care options. Our team of experts will stay by your side through the entire diagnostic process, offering personalized counsel at every step.
For more information on our Comprehensive Breast Health Program, call (470) 610-1910 or email [email protected]. Learn more about our personalized breast care at wellstar.org/breasthealth.
In addition to yearly mammograms, conduct monthly breast self-exams to look for any changes you’ll need to discuss with your provider. Signs of breast cancer can include:
If you notice any of these symptoms, reach out to your provider and schedule an appointment to evaluate your breast health.
Your Wellstar care team will support you at every step of your breast health journey, from screening mammograms to follow-up care.

Comfortably Treating Scoliosis with 3D-Printed Braces
Did you know that Wellstar Pediatric Orthopedics offers innovative bracing options if your child has scoliosis? One of those options is 3D-printed braces, which are tailored to the patient’s body shape, size and spine curvature.
To make the custom braces, a 3D scan is made in the provider’s office, then the brace is 3D printed. The advantage of 3D printing is that due to the architectural design multiple reliefs in the brace can be made, which allows for more comfort, durability and correction.
“We have had excellent outcomes with patient compliance in curve correction using 3D bracing and are monitoring long-term results,” Wellstar Pediatric Orthopedic Surgeon Dr. Timothy Oswald said. “We have made so much progress as a whole as to how we treat scoliosis.”
Bracing for scoliosis has been around for hundreds of years, starting with an iron brace introduced by Andre Pare in the 1700s. In the 1950s, bracing became more popular for treatment of scoliosis with the introduction of the Milwaukee brace, which includes a neck ring with rests for the chin and the back of the head. Unfortunately, the results were poor, with continued progression of the curve and significant effect on the psychosocial development of the teenager. Currently, the only retrospective evidence-based braces available are the Boston brace and nighttime bending brace. These are rigid braces that are mapped according to X-ray parameters for scoliosis correction.
Using a 3D-printed brace is more comfortable for patients because they are lighter than traditional ones and offer more personalized care, with the brace customized for each patient. Since the braces feel less cumbersome, patients are more likely to wear them regularly—leading to better results in treating the spine curvature.
The 3D-mapping technology provided by Wellstar Pediatric Orthopedics can also be applied to bracing of the arms and legs. The goal is to offer more nonsurgical options and support the psychosocial development of every teenager.
To learn more or make an appointment with Wellstar Pediatric Orthopedics, visit wellstar.org/pedsortho.

Feeling Sick? Know Where to Go to Get Care in Douglas
Whether you experience an injury, minor illness or simply need a wellness exam, the most important step you can take is getting the care you need. That way, you can find trained experts for your specific medical needs, stay ahead of potential health issues or even help prevent existing conditions from worsening.
With primary, virtual, urgent and emergency care services available, as well as retail pharmacies, how do you decide which type of care is best for your medical situation? Learn the differences between each type of medical service Wellstar offers in Douglas County—so you don’t delay and get care right away.
In addition to virtual primary and specialty care appointments, we also provide virtual urgent care through WellstarON for minor medical concerns including allergies, sinus infections, strep throat or urinary tract infections.
Your WellstarON provider will offer the same personalized, tailored treatments you expect from us. That may include treatment recommendations and prescriptions to manage an immediate health issue, like an antibiotic or cough medicine.
After your WellstarON visit, all Wellstar providers, including your primary care provider or specialist, can see a record of your appointment. You will also be able to access it through MyChart. Keeping all of your trusted physicians in the know is just one way we provide you with continuity of care.
While virtual care is a convenient way to stay well, it should never be used in place of emergency care. If you are experiencing a life-threatening medical emergency, call 911 right away.
Primary care is ongoing, comprehensive care and preventative medicine that helps you live a full, healthy life.
Your primary care provider gets to know you and your health history on a deeper level. That means they have a more holistic view of your overall wellness.
Services include:
Wellstar has three primary care locations in Douglas County:
8820 Hospital Drive
Douglasville, GA 30134
(770) 947-3000
6043 Prestley Mill Road, Suite B
Douglasville, GA 30134
(770) 941-8100
6095 Professional Parkway, Suite 100
Douglasville, GA 30134
(770) 920-2255
If you’re dealing with a minor injury or illness or need care after your physician’s regular office hours, going to urgent care is often the right choice. Wellstar Urgent Care centers provide quick, convenient care for non-emergency medical conditions.
Wellstar Urgent Care provides:
Check in online to reduce your wait time at Wellstar Urgent Care in Douglasville.
In a life-threatening medical emergency, every second counts. Never put off getting the proper care when lives are on the line. Remember, driving yourself to the emergency department is dangerous and may delay care, so call 911 for the fastest access to emergency care.
When the unexpected happens, Wellstar Douglas Medical Center is always ready in a medical emergency. Our trained team provides expert emergency care 24 hours a day for people of all ages. We also have a dedicated pediatric emergency room, specifically designed to treat children.
Recognize the signs of a medical emergency:
Are You Ready to Take Charge of Your Prostate Health?
To live life to the fullest, men need to keep a pulse on their health stats, including their prostate numbers. Regular well checks and prostate cancer screenings with a primary care physician or urologist can identify prostate conditions—like prostate cancer—early, leading to better outcomes and higher long-term survival.
Partnering with a Wellstar doctor now means that if you are diagnosed later, you’ll have a team of prostate specialists in your court who are ready to support you faster.
For example, if you have prostate-related symptoms or an elevated prostate-specific antigen test, our Prostate Health Program offers patients access to the least invasive and most advanced testing and treatment options. Plus, patients who are diagnosed with prostate cancer will have a multidisciplinary team to provide treatment options. If needed, men can have non-invasive monitoring, minimally invasive robotic surgery or highly targeted radiation therapy at Wellstar—all of which minimize side effects compared to traditional treatments.
Wellstar created the Prostate Health Program to offer men a safe place to discuss sensitive health topics with less anxiety.
One benefit of seeking care at Wellstar is that the team will minimize uncomfortable testing while giving you a best-in-class evaluation that delivers clear results. And you’ll have access to advanced genetic testing. If diagnosed with prostate cancer, patients have immediate access to a team of specialists working together to create the most personalized treatment plan.
“One great benefit of the Wellstar Prostate Program is our multidisciplinary approach to prostate care,” said Wellstar Urologist Dr. Adarsh Manjunath. “We work closely with radiation and medical oncologists to provide holistic care to our patients. The collective expertise and communication between everyone involved optimizes patient well-being.”
At the first appointment, patients meet with a urologist and a nurse navigator. Navigators help bridge the gap between office visits and medical tests. They’ll facilitate scheduling any appointments that are needed, help patients prepare and arrange any follow-up care that may be needed.

Wellstar West Georgia Hospice Volunteers Sponsor their Annual Poinsettia Sale
Wellstar West Georgia Hospice in LaGrange has provided dedicated, compassionate care for patients for more than thirty years. This year, the facility hosts its 35th Annual Poinsettia Sale to share the beauty of the holiday season, while also collecting contributions that directly benefit its mission.
Once again you can continue the tradition when you purchase beautiful poinsettias through this program to share with your family, friends and business associates. The cost is $15 per plant.
Each plant is hand-delivered (free local delivery) by a hospice volunteer with a personalized card recognizing you and your recipient. Delivery dates for the flowers are Monday through Thursday, December 2 - 5, 2024, in plenty of time to enjoy their beauty all throughout the holiday season.
Please visit the Poinsettia Sale Order Form page to start your order. If you have questions, please call Sandy Melton at 706-803-7335 for assistance. Note that orders more than $75 will be acknowledged showing your tax-deductible contribution.
Funds raised will be used for patient care services for hospice patients at Wellstar West Georgia Hospice, as well as those being served in their own homes, nursing homes, and assisted living facilities. West Georgia Hospice provides services to all regardless of their ability to pay.
Thank you very much for supporting the ongoing care efforts of West Georgia Hospice in our community. And don't delay: the deadline to place your order is November 1, 2024.
Your support of Wellstar West Georgia Hospice is sincerely appreciated, thank you!
Place your Poinsettia Order here!

Navigate Your Breast Care with Concierge Services from the Wellstar Comprehensive Breast Health Program
When a screening mammogram result is flagged for follow-up care, it can be stressful and scary for patients and their loved ones. The Wellstar Comprehensive Breast Health Program supports patients with a full team of experts dedicated to navigating what can otherwise be an overwhelming process.
This concierge service helps patients who have received abnormal screening mammogram results, along with their support systems, make informed breast health decisions. Our dedicated team of schedulers, nurse navigators and breast care specialists will stay by your side through the entire diagnostic process, offering personalized counsel at every step—and it’s complimentary for anyone who has their screening mammogram performed at a Wellstar imaging center.
Our care team is invested in patients’ physical and emotional well-being and provides personalized guidance as patients follow up on their mammograms and set next steps. At Wellstar, no patient has to walk through their health journey alone.
This integrative program, available at no additional cost to patients who have received abnormal screening mammogram results, offers consultation services via secure Wellstar MyChart messaging, email and telephone calls, so you can get care anywhere.
Regular mammograms are essential to helping in the early detection of breast cancer.
“If you’re at average risk of developing breast cancer, you should start annual mammograms at age 40,” said Wellstar Chief of Women’s Health Dr. Paula Greaves. “However, if you have a family history of breast cancer or other risk factors, your provider may recommend starting earlier and will help you create a screening plan.”
When it’s time for your mammogram, Wellstar offers 16 mammography locations, and our patients have state-of-the-art technology on their side. We offer high-resolution breast screening, including 3D mammograms.
A 3D mammogram provides a series of detailed images of the breast, allowing healthcare providers to better evaluate breast tissue layer by layer, making fine details more visible and no longer hidden by overlapping tissue. A 3D mammogram is clinically proven to provide more accurate breast cancer screening and can help reduce false-positive callbacks for additional imaging.
Call (678) 581-5900 to schedule your mammogram. You can also ask your Wellstar care team to put your mammogram order in MyChart and you'll have the ability to schedule online.
If you are of average risk and your screening mammogram results are normal, your next mammogram will be the following year. In addition to yearly mammograms, your clinician may recommend that you conduct monthly breast self-exams to look for any changes you’ll need to discuss with your care team. If you notice anything such as a lump, sore spot or a difference in the appearance of the skin, schedule an appointment to have your doctor evaluate your breast health.
If your screening mammogram is abnormal and you need follow-up care, a member of the Comprehensive Breast Health Program team will contact you to schedule additional imaging, automatically including you in this complimentary concierge program. They can also answer any questions you have about the program, next steps, what to expect at your follow-up appointment and more. If your additional imaging also shows an abnormal result, your care team will remain by your side, guiding you through every needed follow-up care step, which may include additional imaging, breast biopsy or specialist referral.
In the event you are diagnosed with breast cancer, treatment transitions from the Comprehensive Breast Health Program to the Wellstar Cancer Care team. The Comprehensive Breast Health Program team will coordinate this transition, and your breast health navigator will connect you with one of our oncology nurse navigators—registered nurses who bring a highly personalized level of guidance and support to each patient. The Wellstar Cancer Care team will continue to provide compassionate care with a multidisciplinary team of experts.
An abnormal screening mammogram result can be overwhelming and upsetting for patients and their support systems. As you seek answers about your breast health, the concierge services of the Comprehensive Breast Health Program can make the process more seamless by helping with steps including:
Learn more about how our team can support you at wellstar.org/breasthealth. Contact our team by calling (470) 610-1910 or emailing [email protected].

Fueling Up for Sports this School Year
Wellstar knows that the beginning of the school year is often accompanied by getting back to extracurricular activities. With the return to the classroom and competition arenas, we know parents, coaches and teachers alike are concerned that their student athletes are fueling their bodies and brains for optimal performance.
Wellstar Pediatric Orthopedics recommends getting the correct amount of protein, carbohydrates, healthy fats, iron, calcium and vitamin D, as well as fluids. Dietary supplements are not needed for youth athletes unless recommended by a healthcare professional. It is more important to meet the body’s caloric needs.
For hydration, it’s recommended that student athletes consume up to 20 ounces of fluid one hour before an activity and 5 ounces every 15 minutes during the activity.
“Proper nutrition and hydration are critical for all students, but particularly for athletes who are more active and burning more calories,” said Dr. Lindsay Stephenson, Wellstar pediatric orthopedic surgeon and sports medicine specialist. “I recommend using the nutritional guide released by the Pediatric Orthopaedic Society of North America. This information makes it easier for students and their parents to understand the nutritional needs of the body to perform in the classroom and during competition.”
Access the recommended nutritional guide.
To learn more or make an appointment with Wellstar Pediatric Orthopedics, visit wellstar.org/pedsortho.

Wellstar and Augusta University Officially Launch Unified Health System
Wellstar Health System and Augusta University Health System (AUHS) are pleased to announce that today is our first day as a unified system. AUHS will now be known locally as Wellstar MCG Health. Together, Wellstar and Wellstar MCG Health will revolutionize healthcare and enhance the well-being of communities across Georgia. This transformative partnership is set to make a significant impact on the lives of people throughout the state.
Through this partnership, we are committed to investing in cutting-edge medical facilities and infrastructure, strengthening collaborations with rural hospitals, and providing greater access to digital health services and top-notch clinical care, such as the exceptional pediatric care offered by Wellstar and Children’s Hospital of Georgia. Most importantly, we’re focused on addressing the unique needs of each person and community we serve as effectively and compassionately as possible.
Our vision doesn’t stop there. This partnership also represents a powerful alliance between Wellstar Health System, the University System of Georgia, Wellstar MCG Health and one of the nation’s best public medical schools, Augusta University’s Medical College of Georgia (MCG), to propel medical education and research forward. By continuing to build on the rich legacy of MCG and creating new opportunities for more physicians to be trained in a modern clinical environment, we are addressing physician shortages in our local communities and contributing to solving this challenge nationwide.
The possibilities that lie ahead are extraordinary, and we can’t wait to expand our shared commitment to enhancing the health and well-being of the people we serve across our great state. We are forging a path toward a brighter, healthier future for Georgia and beyond.
This statement is issued jointly by:
Sonny Perdue, chancellor, the University System of Georgia
Candice L. Saunders, FACHE, president and chief executive officer of Wellstar Health System
Brooks A. Keel, Ph.D., acting chief executive officer of Augusta University Health System and president of Augusta University

HealthyOwlCare
Between adjusting to college life, meeting friends in the dining hall and cramming for that big exam, Kennesaw State University students have a lot on their plates.
While students maintain those busy schedules, it’s still important they keep up with their health so they can feel their best inside and outside the classroom. Wellstar provides expert student health services, keeping world-class care convenient and on campus.
Services include:
Click, call or come in—easy online booking helps students take the first step toward taking charge of their health. Visit any of our student health locations on Campus Loop Road in Kennesaw, in University Village in Kennesaw or in University Courtyard in Marietta.
While physical health is an important part of overall wellness, it’s crucial that students look out for their mental well-being too. We offer compassionate, confidential care for mental health concerns with conveniently located offices on the Kennesaw and Marietta campuses. Call (470) 578-6644 to make an appointment. Learn more or book online at ksu-health.wellstar.org.

New Clinic for Leptomeningeal Disease at Wellstar Georgia Cancer Center
When a family member receives a cancer diagnosis, you want the absolute best cancer care for them. Having multiple family members impacted by cancer and neurological conditions inspired Dr. Gerald Wallace to pursue neuro-oncology and to create the Leptomeningeal Disease Clinic at Wellstar Georgia Cancer Center. The goal of the clinic is to diagnose, treat and raise awareness of the life-threatening disease.
“Neurology and cancer have deeply impacted my life for as long as I can remember,” said Wallace, an assistant professor in the division of Hematology/Oncology at the Medical College of Georgia. “I love doing this job; everything about it is just fascinating to me.”
Leptomeningeal disease is a type of metastatic cancer. The leptomeninges are two layers of tissue within the meninges that cover the brain and spinal cord. They are the innermost layers, which line the surface of the brain, blood vessels and surround the cerebrospinal fluid. Researchers estimate that 5% to 8% of people with cancer will develop leptomeningeal disease. It is also estimated that of the nearly 54,000 Georgians diagnosed each year with invasive cancer, as many as 4,000 are at risk of developing leptomeningeal disease. While there is still much that is unknown about the disease, experts do know that it is life-threatening. Without treatment, most patients will only live another six to eight weeks. With treatment, people can live well for months and, in some cases, years.
“That six to 12 months is the next graduation, the next wedding, the next birth of a child… at the end of the day I think we are all just fighting for time to spend with our loved ones. So, we should do something. Treatment is not that bad; it is quite tolerable,” said Wallace.
Possible symptoms that are associated with leptomeningeal disease are visual changes, stiff neck, trouble walking, headache that worsens when lying down, urinary/bowel incontinence, and memory issues. Wallace is concerned when he sees a patient with neuropathies or new neurological symptoms that do not connect to a patient’s known disease. When he hears or sees these sorts of symptoms, he sends patients to get tested. He thinks leptomeningeal disease is easily missed because most patients will already have had cancer for months or years. For these patients, symptoms may be attributed to treatment rather than cancer in the leptomeningeal space.
“If you have problems with one nerve here and one nerve over there, and I cannot connect the two… that really makes me nervous. Something is going on in a more global space than would otherwise be indicated in, say, a tumor that was sitting in the visual cortex and you cannot see well,” he said.
There are treatment options for patients diagnosed with leptomeningeal disease. The first step is to confirm the diagnosis. Contrasted MRI of the brain and spinal cord is used to see if there is anything suspicious or out of the ordinary. MRI is followed by two lumbar punctures to see if there is cancer in the cerebrospinal fluid. Once the diagnosis is confirmed, the next step is radiation of the brain and possibly the spinal cord. Finally, patients meet with a neurosurgeon to discuss placement of an Ommaya reservoir. An Ommaya reservoir is a special port that allows access to the cerebrospinal fluid in the brain. It sits under the hairline on the scalp and is an easier way to give chemotherapy, evaluate spinal fluid and decrease intracranial pressure.
Wallace uses a variety of medications that are given through the Ommaya reservoir to treat leptomeningeal disease. The choice of medication depends on the type of cancer, specific mutations in the cancer and, most importantly, the ability of the patient to tolerate therapy. Patients start off going weekly for treatment for a few months. If they see good results, they can start going every other week, then monthly.
In recent years there have been major breakthroughs for drugs that may be able to treat leptomeningeal disease. Wallace is excited about their potential and is working to create clinical trials at the Wellstar Georgia Cancer Center to assess that potential. As people live longer with cancer, the likelihood of a cancer survivor being diagnosed with leptomeningeal disease also increases.
“I think there is great potential to make big strides in survival and quality of life for patients with leptomeningeal disease,” he said.
If you are concerned about leptomeningeal disease, you can schedule an appointment with Wallace and his team by calling (706) 721-2505.

Top Marks for Heart Care at Wellstar Kennestone Regional Medical Center
Wellstar Kennestone Regional Medical Center recently received two major commendations highlighting the high level of heart care continuously provided to patients—putting Wellstar Kennstone among the top hospitals in the nation. The Marietta-based heart care program received:
“This community is where we live, and when we care for our patients, we’re caring for our neighbors and friends—that’s why pursuing excellence is such a high priority,” said Steve Cermak, executive director of Wellstar Center for Cardiovascular Care & Hospital Operations at Wellstar Kennestone Regional Medical Center. “We feel it’s our duty to provide the highest level of care possible.”
Don’t forget your keys to family health—checkups, screenings and vaccinations
Republished with permission of the Atlanta Business Chronicle
This article was originally published on Atlanta Business Chronicle on July 14, 2023.
The key to avoiding health problems is prevention, and the keys to prevention are annual checkups, regular screenings and vaccinations. With the start of the next school year looming in late summer, healthcare experts in Atlanta say it’s a good time for families to get back into the routine of scheduling and keeping these important appointments—not just for children, but for parents too, especially that one parent who tends to be the primary scheduler, often the mother.
In an Atlanta Business Chronicle panel discussion in partnership with Wellstar, physicians from Wellstar and Cobb & Douglas Health District discuss why checkups are important and how families can overcome obstacles to stay on track with preventative care.
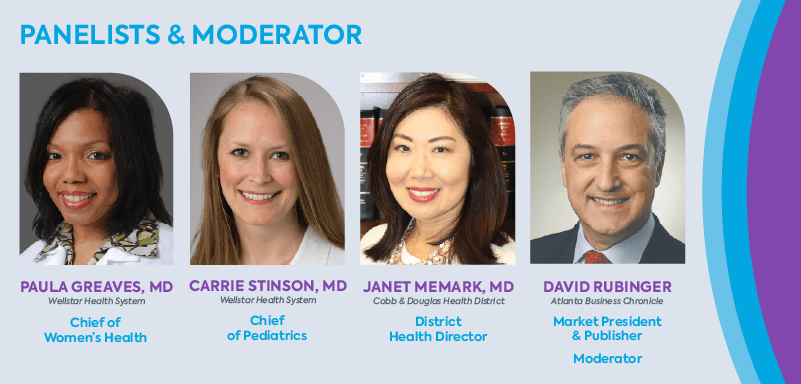
David Rubinger, Atlanta Business Chronicle market president and publisher: When we think about family wellness and how it intersects with our daily work routines, it can get very complicated, given how busy working professionals are. We’re trying to figure out a way to manage not only our children’s health, and maybe our parents’ health if we’re in the sandwich generation, but our own health. The checklist is longer and longer every day. Let’s start with the basics. We’re a few weeks away from the start of school. Dr. Stinson, what are you telling your parents of kids of school age right now?
Dr. Carrie Stinson, Chief, Pediatric Service Line, Wellstar: The summer is a great time to get caught up on all the things that fall through the cracks during the busy school year. Our lives are very hectic, and when school starts back, things get even busier.
One big thing is the annual well-child exam. Every child should have a well-child exam every single year. When you have babies and toddlers, it’s routine — you’re scheduling these frequently. When kids get older and busier, these visits may feel less important and fall off your radar.
Well visits are important every year. They focus on the comprehensive health and well-being of your child. Pediatricians focus on physical health, development, emotional, social, and even behavioral health. During these visits, the care team collects information on patient and family history, talks about developmental milestones and how your child is doing in school socially. We also assess sleep habits and nutrition. As they become adolescents, well-child exams become even more important as we ask questions about your child’s mental and sexual health.
Those are important conversations to start having and your pediatrician can be a great facilitator. Sometimes parents are uncomfortable talking about those topics with their children even at an early, pre-adolescent stage, so those well checkups are really great places to get insight on how to approach sensitive topics.
Rubinger: Dr. Stinson, since COVID, tell me what you’re seeing that’s different in terms of talking to both parents and children. I am sure the pandemic took some families off their schedules for well checkups. How has the doctor-patient pediatric conversation changed over the past couple of years?
Dr. Stinson: What we’re hearing from our pediatricians since COVID is also what we’re hearing in the news. The behavioral and mental health crisis that we’re experiencing in this country has been really impactful on children, especially teenagers. During COVID, the social isolation of being out of school for periods of time had a significant impact on adolescents. The rise in social media popularity during that time also had a negative impact on pediatric mental health.
Our pediatricians are really seeing that impact now. They’re feeling the strain our teenagers are experiencing. We’re seeing many more cases of depression and anxiety, and cases that escalate to dangerous proportions such as suicidal thoughts and actions.
We’re trying to respond to it by increasing the resources in our communities, but it’s hard to move fast enough to keep up with the demand. At Wellstar, we are developing an integrative model for behavioral health into our pediatric offices. Five of our pediatric practices will have embedded behavioral health professionals, so pediatricians can make direct referrals and patients have immediate access to behavioral health providers in their pediatric office setting.
Rubinger: Dr. Greaves, the mother might be the caretaker who takes care of the child. Most mothers would put their kid’s health ahead of their own health. Tell me what you are experiencing in terms of women’s health as it relates to those people who are the caretakers. What are the issues that they’re having to face to address their own needs?
Dr. Paula Greaves, Chief, Women’s Health Service Line, Wellstar: Women are usually considered the CEOs of their households and the drivers of healthcare in the community. Most women are the care bridge between several generations. They take care of their children, their parents, their partners and at times their communities.
Unfortunately, they sometimes forget to take care of themselves. As physicians, it is our duty to ensure that women are made aware of the warning signs their bodies may be sending them and encourage them to seek help earlier to improve health outcomes.
There are nine signs that I tell my patients to watch out for:
Rubinger: Is there ever a situation, Dr. Stinson, where you are treating a child and you see a mother whom you can tell is having health issues, even without an exam? As a pediatrician, do you ever say, “Hey, I think you need to get that checked out?”
Dr. Stinson: As pediatricians, we really focus on the whole family. While we’re seeing the child, we’re also interacting with the parents, guardians, grandparents, or whoever’s bringing the child in to see us on a routine basis.
I think we often get questions from family members about their own health because of exactly what Dr. Greaves mentioned. People think, “I am in a doctor’s office. I don’t have time to go to my own doctor. Let me just see if I can get this question answered.
While being careful not to give medical advice to a patient who is not ours or who is outside of our scope of practice as pediatricians, we are very willing to give recommendations on where that person should seek care. One benefit of our health system is we have the expertise to take care of patients from before they’re born until they need end-of-life care. We have a scope of providers within our system who can help with pretty much any problem that might come up. I would not hesitate to refer a patient to Dr. Greaves and say, “This mom is really worried about her own health. Can you please help? She’s very busy, but her symptoms sound concerning. Can you maybe work her into your schedule?
I practice in the hospital, and we have sent several parents to the emergency room in our hospital for their own health while we’re taking care of their child in the pediatric unit.
Rubinger: Dr. Memark, you get to look at this from the standpoint of two counties that are in great need of public health support. What are the trends that you’re seeing at a 30,000-foot view? What do you see within your communities that your organization tries to address?
Dr. Janet Memark, District Health Director, Cobb & Douglas Health District: From my point of view, one of the big things that we do at Cobb & Douglas Public Health is a large community health assessment. Dr. Greaves is actually a member of our board. We just finished a 2016-2020 five-year assessment. This was at the beginning of the pandemic, so keep that in mind. Our next assessment will capture 2021-2025. One of the things that was surprising to me was looking at causes of death in our communities. The assessment showed that in older people, it’s what you’d expect. For example, in Cobb County for those age 75 and older, the leading causes of death are things like vascular disease, stroke and Alzheimer’s. For ages 65 to 74, it’s heart disease and cancer. But when we started looking at the lower age groups, I was very surprised at what I saw:
After the timeframe studied in the assessment, we went through two more years of the pandemic, which affected almost everyone’s mental health in one way or another. We’ve heard on the news how pediatricians in medical school are now being trained on how to provide more extensive mental healthcare because there just aren’t enough mental health experts.
It’s wonderful to hear Dr. Stinson say they are really trying to bolster up mental health screenings for our young people during their pediatric visits. I’d also like to add that we have high rates of maternal mortality in Georgia. The state Department of Public Health did a deep dive and found that mental health is a huge component of maternal mortality. You see these same themes of mental health running through several different medical specialties.
One-Stop Treatment Clinic for Patients with Thoracic Cancer
If you had to guess which cancer took the most lives in America, what would your guess be?
“Lung cancer is the No. 1 cancer killer in the U.S. for both women and men since 1986,” said Dr. Daniel Miller. Miller is the chief of thoracic surgery and the director of the Wellstar Georgia Cancer Center lung cancer screening program.
About 80% of lung cancer cases are associated with cigarette smoking, including secondhand smoke. Unfortunately, when symptoms begin showing, the cancer has already spread, making treatment very time-sensitive. When a patient is diagnosed, their care team typically includes not just one, but four doctors: a thoracic surgeon, an interventional pulmonologist, a medical oncologist and a radiation oncologist. There are many benefits to having a large care team, but a huge drawback can be the wait time between appointments with each doctor.
“When you have cancer, you want to be seen now and be treated now,” said Miller.
The speed of treatment time for patients is what inspired the creation of the Thoracic-Oncology NOW (New Oncology Workgroup) Clinic at Wellstar Georgia Cancer Center. The multidisciplinary clinic is staffed by specialized physicians in the treatment of thoracic malignancies. The staff includes Miller and Dr. John Kuckleman as the thoracic surgeons, Dr. Rabih Bechara as the interventional pulmonologist, Dr. Girindra Raval as the medical oncologist, and Dr. William Grubb as the radiation oncologist.
The clinic has seen 50 patients since opening in October 2022 and treats not just lung cancer, but also esophageal cancer, metastatic disease to the lungs and malignant pleural effusions.
“You’re cutting back on treatment time, waiting time, travel time and, more importantly, you have a group of doctors, rather than a doctor, who are talking about your care,” said Raval.
The clinic operates on Wednesdays and acts as a one-stop shop for patients, saving their time and the time of their loved ones who join them for treatments. Patients also have access to Wellstar Georgia Cancer Center’s registered dietitians and social workers, along with a scheduler, financial personnel and medical assistants, creating one large care team ready to help them on their treatment journey.
“There is a degree of reassurance for the patient that there is a team who are all engrossed in caring for that patient,” said Raval.
To learn more about the Thoracic-Oncology NOW Clinic or make an appointment, call (706) 721-6744 for more information.

Wellstar West Georgia Medical Center Receives Primary Stroke Certification
Wellstar West Georgia Medical Center recently earned Primary Stroke Certification from The Joint Commission.
Offered in collaboration with the American Heart Association/American Stroke Association, achieving Primary Stroke Center (PSC) Certification means the hospital is making exceptional efforts to foster better outcomes. It’s a signal to the community that quality of care provided meets the unique and specialized needs of stroke patients.
Joint Commission-certified PSCs adhere to a set of standardized performance measures. Organizations collect monthly data for each measure in the set, and the data is then submitted quarterly to The Joint Commission.
“This important certification as a primary stroke center demonstrates our team’s commitment to a higher standard of clinical service,” says Coleman Foss, Wellstar West Georgia Medical Center President. “Stroke patients can be confident in the quality and safety of care, treatment and services delivered at West Georgia Medical Center.”
West Georgia Medical Center joins Wellstar's network of other stroke-certified hospitals, including Comprehensive Stroke Centers Wellstar Kennestone and Wellstar North Fulton, other Primary Stroke Centers Wellstar Cobb and Wellstar Spalding, and Remote Stroke Treatment Centers Wellstar Douglas and Wellstar Paulding.
Wellstar, Affiliated with Medical College of Georgia, Adds Bacon County Hospital and Health System to Rural Hospital Virtual Care Network
Wellstar, affiliated with Medical College of Georgia, has added Bacon County Hospital and Health System to its Rural Hospital Virtual Care Network, which comprises 16 hospitals across Georgia and allows patients in rural areas to receive Wellstar’s world-class care closer to home.
Through this network, rural health systems have access to teleconferencing equipment, software and portable point-of-care equipment like ultrasound machines and airway devices, allowing physicians and specialists at Wellstar and the Medical College of Georgia to guide local physicians through diagnostic tests and procedures. This enables patients to remain in their local hospitals while receiving the same level of specialized care they would receive in a larger hospital. Not only is this more comfortable for the patient, but it is more affordable than transferring to a hospital in a larger city.
“For Bacon County, this partnership means we can take care of local patients in our organization and have a network of specialists readily available,” said Kyle Lott, chief operating officer of Bacon County Hospital and Health System. “I’m excited for this partnership and look forward to the opportunities it brings.”
The Rural Hospital Virtual Care Network currently partners with 16 hospitals across Georgia. It has helped more than 2,000 patients be treated in their home communities and increased viability for their local hospitals. For rural hospitals this means increased revenue, which helps them provide high-quality care.
“Bacon was a great location because they are a critical access hospital that has OB/GYN services, which is very unique for a rural community hospital. What we have been trying to do is create the clinical affiliations with sites to help strengthen the relationship and provide opportunities to put residents or medical students onsite to learn in rural Georgia, to hopefully retain those students in rural Georgia,” said Lauren Hopkins, associate vice president of virtual care and community engagement at Wellstar, affiliated with Medical College of Georgia.
The Rural Hospital Virtual Care Network at Wellstar, affiliated with Medical College of Georgia, is part of its telehealth initiative, which also includes Virtual Care at Home.


Wellstar National COVID-19 Resiliency Network Partnership Reaches Over 1 Million People
After leveraging partnerships and community relationships to serve and educate patients during the COVID-19 pandemic—reaching over a million people—Wellstar Community Health and Wellstar Center for Health Equity teams continue community outreach efforts.
Since 2020, Wellstar has partnered with Morehouse School of Medicine to join the National COVID-19 Resiliency Network (NCRN)—a nationwide consortium of organizations committed to improving the reach of COVID-19 health messaging, increasing connections to healthcare and social services, decreasing disparities in COVID-19 testing and enhancing community capacity for addressing the pandemic.
Programs led by the Wellstar Center for Health Equity throughout the COVID-19 pandemic have included walk-up COVID-19 family testing and vaccination, distribution of masks and safety kits to at-risk communities, and dissemination of Spanish-language educational information. Wellstar will continue this work by educating communities about the spread of disease and distributing masks and hand sanitizer to fight illnesses such as the flu and COVID-19.
Through partnerships like the one with NCRN, the Wellstar Center for Health Equity implements multidisciplinary approaches to address social disparities and barriers to healthcare access.
Many patients skipped routine health screenings during the pandemic. Wellstar Community Health and the Wellstar Center for Health Equity focus on connecting community members with primary care providers and screenings including colorectal and prostate cancer screenings, continuing the outreach from the pandemic and meeting patients where they are.
“We recognized that people were working or had kids, and we tried to break down those barriers and get healthcare to people where they needed it,” said Nurse Manager Cindy Newman, who works with Wellstar Community Health and the Wellstar Center for Health Equity.
Wellstar Community Health and Wellstar Center for Health Equity teams collaborate with partners such as the Georgia Department of Public Health to increase access to COVID-19 testing and vaccines.
Through the Wellstar Congregational Health Network—our partnership with local faith communities—Wellstar made testing, vaccines and accurate health information more accessible to the people we serve by hosting events at places of worship and virtual town halls in collaboration with faith communities.
Collectively, NCRN has reached over 1 million people and counting through virtual and in-person events. In addition to joining NCRN, Wellstar is also part of Georgia CEAL, another initiative of Morehouse School of Medicine that addresses the disproportionate impact of COVID-19 on underserved communities.
Learn more about Wellstar Community Health and the Wellstar Center for Health Equity.

Prostate Cancer Screening in Black Men
Screening for prostate cancer is crucial for early detection and to help provide the best possible outcome. It is especially important for Black men to be vigilant about screening, as they are disproportionately impacted by this cancer.
About 1 in 6 Black men will be diagnosed with prostate cancer in their lifetime, compared to 1 in 8 white men, according to a report from the American Cancer Society. Prostate cancer is the second leading cause of cancer death in Black men.
The American Cancer Society recommends that men at an average risk of developing prostate cancer begin screening when they are 50, but Black men should start earlier—at age 45 if they have no family history of prostate cancer, and at age 40 if any of their male relatives have had prostate cancer. Wellstar takes a personalized approach to cancer screenings, with clinicians discussing benefits versus risks of screening and helping patients evaluate their risk.
“Despite many physicians being aware of this and following this practice, Black men continue to be diagnosed with and die from metastatic prostate cancer. This is a trend that desperately needs to be reversed,” said Wellstar Primary Care Physician Dr. Earl Stewart. “We have adequate screening tools that do not even require a digital rectal examination.”
The Prostate-Specific Antigen (PSA) blood test is more accurate than the digital rectal examination in helping to detect prostate cancer, according to Dr. Stewart. Patients should also discuss family history with their relatives. “Patients knowing their family history is so crucial in having those discussions with primary care physicians to determine the best age at which to start screening,” Dr. Stewart said.
Screening for prostate cancer is as simple as making a preventive appointment with your primary care physician, discussing your family history with him or her, and having a PSA blood test. This test may be performed during an annual physical or wellness visit. Shared decision making between physician and patient is important to discuss your risk, your need for testing and next steps to take if your PSA level is elevated and concerning. Knowing your risk can save your life.
“I know many personally who are near and dear to me who had the disease and who unfortunately died from complications of metastatic prostate cancer,” Dr. Stewart said. “I know many more who lived because they had the conversation and dared to move forward with appropriate screening at the appropriate age.”

Wellstar Paulding Medical Center Joins Hidden Disabilities Sunflower Network
Wellstar Paulding Medical Center is the first hospital in North America to join the Hidden Disabilities Sunflower network. Adopted by the hospital’s Diversity, Equity, Inclusion & Belonging (DEIB) Council, the initiative aims to help people who have disabilities that are not immediately obvious, such as visual or hearing impairments, autism, chronic pain, dementia or anxiety.
“We want to foster a sense of belonging and respect for every patient, family member and team member,” said Rev. Dr. Rhonda James-Jones, manager of Spiritual Health at Wellstar Paulding Medial Center & Nursing Rehabilitation Center. “Paired with education and other care initiatives, the Sunflower will enable every member of our team to provide the highest quality, most personal care for patients with invisible disabilities.
At the hospital, the official Hidden Disabilities Sunflower logo — a yellow sunflower on a green background — is placed on the door of a patient with a disability. The Sunflower symbol discreetly indicates to patient-facing team members that the wearer needs additional support or a little more time when a diagnosis or procedure is explained.
“The Sunflower will help us in our efforts to honor every voice at Wellstar,” said Tricia Everitte, a Wellstar registered respiratory therapist and Sunflower program initiative lead.
Everitt introduced the effort to the hospital because she cares for people with hidden disabilities both professionally and personally.
She added, “Several nurses and other team members have shared that they have people with hidden disabilities in their lives and are proud to work at a hospital that will go the extra mile to meet their needs.”
The Hidden Disabilities Sunflower has been adopted globally across all public sectors including major airports, supermarkets, entertainment and sports venues, government programs, public safety services and an increasing number of businesses, large and small.
“Our aim is to help make the invisible, visible,” said Paul White, CEO, The Hidden Disabilities Sunflower. “We’re thrilled to welcome Wellstar Paulding Medical Center to the global Hidden Disabilities Sunflower network. As the first hospital in North America to join the Sunflower, we champion and share their drive to support people with non-visible disabilities within the healthcare sector.”
The Sunflower is another layer of support as the team at Wellstar Paulding seeks to provide high-quality healthcare to every person, every time. Patients at Wellstar Paulding also have access to whole person-centered care provided by clinically trained chaplains and pet therapists, as well as through technology such as adaptive phones and interpretation services.

CureSearch Awards $1.2 million for Pediatric Cancer Research at Wellstar Georgia Cancer Center, Wellstar Children’s Hospital of Georgia
The national nonprofit CureSearch for Children’s Cancer presented a check Wednesday, June 14, 2023 for $1.2 million to help fund promising pediatric cancer research at the Wellstar Georgia Cancer Center and Wellstar Children’s Hospital of Georgia.
CureSearch awarded Dr. David Munn and Dr. Theodore Johnson at the Medical College of Georgia at Augusta University with this funding in conjunction with the Catapult Award, which identifies and helps propel high-potential research from the lab into the clinic and, ultimately, to the kids who need it most.
Munn and Johnson have been hard at work for several years developing anti-tumor therapies for patients with brain cancers that are actively progressing. Initially, these patients may have benefited from the groundbreaking therapy of indoximod, the first-in-class drug developed by Munn and his team in 2015 that inhibits the enzyme indoleamine 2,3-dioxygenase (IDO). However, for those children who have become resistant to such treatment, the introduction of ibrutinib may prove successful.
Currently, the focus is on malignant brain tumors—which, unfortunately, is an underserved area of pediatric cancer research and treatment, and there is seldom a pathway of treatment that can offer a cure. The CureSearch funding will help support a Phase 1 trial of ibrutinib/indoximod for patients at Wellstar Children’s. If successful, the novel treatment could improve the quality of life for patients at Wellstar Children’s and beyond.
CureSearch is a national nonprofit organization that only funds translational research projects with the strongest potential of becoming a new treatment and quickly reaching pediatric patients. CureSearch’s mission is to end childhood cancer by driving targeted and innovative research with measurable results in an accelerated time frame. To learn more visit curesearch.org.
The Rally Foundation for Childhood Cancer Research and Fisher Phillips are contributors to CureSearch and helped fund this award.

Wellstar Foundation Receives Additional Funding to Support Child Literacy and Address Social Determinants of Health Through the Small TALK Program


Wellstar CEO Candice Saunders visits Small TALK program
Wellstar Paulding Medical Center Expands Cancer Care with New Radiation Technology
New radiation therapy technology at Wellstar Paulding Medical Center doubles the hospital’s availability for radiation treatment and expanded cancer care for the region.
Wellstar Paulding added a new radiation vault, which houses a second linear accelerator. The TrueBeam technology delivers high-precision doses of radiation with flexible treatment options, including the capability to change the size and shape of beams to mimic the tumor shape and minimize exposure to surrounding tissue.
The linear accelerator can shorten the time of each treatment and for some patients, may reduce the number of treatments needed. Adding a second linear accelerator enables the cancer care team at Wellstar Paulding to double availability for radiation treatment, offering more convenient appointment times for patients.
“It gives us the versatility to address many different cancer situations in a more efficient way,” said Dr. William Thoms, the radiation oncology medical director for Wellstar Paulding. “The time of each treatment can be reduced, and the potential to accomplish the mission in fewer treatments is also there. We have the capability of targeting treatment so we can minimize injury to normal tissue.”
The linear accelerator is well-suited for treating cases where minimizing damage to normal tissue is especially important, such as in the brain, spinal cord or organs where a patient has previously received radiation treatment, according to Dr. Thoms.
As Wellstar Paulding expands its cancer care services, the new linear accelerator will also be used for stereotactic body radiation therapy (SBRT), which has not previously been offered in Paulding County. This method can treat tumors anywhere in the body with highly targeted, high-dose radiation. Because it uses multiple X-ray beams coming from different angles, as well as high treatment precision, surrounding normal tissues are spared.
Learn more about cancer care at Wellstar Paulding Medical Center.

No One Dies Alone Ensures Compassionate Care in Patients’ Final Moments
Many patients have family and friends who surround them during their final moments of life. Others—due to any number of circumstances—find themselves alone, without the support and emotional comfort needed during this difficult time.
To ensure that all patients have companionship and compassionate care at the end of their lives, the Office of Spiritual Care at Wellstar MCG Health Medical Center is launching an initiative called No One Dies Alone (NODA). The program is based on the premise that dying patients should not be left alone during their final moments.
“For patients without families, this means having a peaceful transition,” said Rev. Stephen Hughes, associate director of Spiritual Care. “Somebody is constantly with them, holding their hand, letting them know it’s OK, you’re not alone. I love you. All those things.”
At the heart of the program are caring volunteers. Hughes said the department is looking for six volunteers to begin the program. They will go through training together, form a team to support each other, and take turns sitting with patients who are alone and close to the end of life.
Potential volunteers will go through a drug screen, a background check and a rigorous screening process to ensure they truly want to provide compassionate care. Hughes said he wants to ensure that the volunteers are committed to serving and not just looking for something good to do.
Training includes learning about the dying process, how to provide the care the patient needs, how to be inclusive and how to use inclusive language.
“Training would include what to do to provide that compassionate presence—what tools are available, what to do and not to do in the room,” Hughes said.
If a family is unable to be with a loved one, it can be a comfort for them as well to know that the patient will not be alone in their final moments. Chaplains work together as a team to be with patients at the end of life, and NODA volunteers will partner with them to provide this meaningful care.
Hughes recalled a day during the pandemic when he’d been with several patients in their last moments, but one patient in particular stood out. The patient’s family couldn’t be with him because they all had COVID-19. Hughes had talked with them by phone to assist physicians in getting permission to put the patient on comfort care. The family asked Hughes to stay with the patient and told him some of the patient’s favorite songs.
“I took my phone in there with him and played some of his favorite music until he passed. The family really, really didn’t want him to be alone,” he said. “If it was my family, I would want somebody with him, just to let him know it’s going to be OK.”
For more information, or to learn how to apply to be a volunteer, call Hughes or Chaplain Linda Hamilton in the Office of Spiritual Care at (706) 721-2929.

Families Learn About Healthy Grief at Camp Tranquility
We all cope with grief differently, but its weight can impact us mentally and physically. Seeing the need for grief support among families, especially children, inspired Wellstar Hospice Care to host Camp Tranquility, a one-day community workshop for families who have experienced the loss of a loved one.
“The child campers are accompanied by their adult caregivers and through breakout sessions they learn healthy mechanisms for understanding and experiencing grief in a fun and supportive environment,” said Natalie McNeal, executive director of Wellstar Hospice Care. “This year, activities will include healthy ways to grieve through exercise, reflection, arts and crafts, and new friendships.”
This year’s Camp Tranquility, funded by donations to the Wellstar Foundation, will be held Monday, July 17 from 9 AM - 5 PM at Truist Park.
Watch the video below to see activities from last year’s Camp Tranquility, held at the Georgia Aquarium.
Wellstar Paulding Medical Center Transforms Cancer Care With Major Renovation
On May 23, Wellstar Health System hosted a ribbon cutting to celebrate the completion of a major renovation to bring advanced cancer treatments to people in Paulding County and surrounding communities. The event was hosted at Wellstar Paulding Medical Center in Hiram, Georgia, and attended by patients, physicians, healthcare leaders, team members, government officials and community partners.
“We strive to bring world-class healthcare to our neighbors every day,” said Ralph Turner, Wellstar senior vice president and president of Wellstar Paulding Medical Center. “We opened this new hospital almost 10 years ago, but that was not the finish line — just a stop on our journey. We continue to find new ways to keep pace with this community’s growth and provide the most comprehensive cancer care to this community.
The expansion enhances the patient experience by adding a new radiation vault to house a TrueBeam linear accelerator — an advanced system that delivers radiation therapy. While the capacity to treat people with cancer doubled, new technology brings more cutting-edge treatments to Paulding, alongside a modernized dressing room area offering patients more space and comfort.
“This is a dream come true after seeing the growing need for cancer treatment in this area,” said Dr. William Thoms, Radiation Oncology medical director. “The new TrueBeam allows people to stay closer to home rather than driving outside our own community for radiation therapy."
The expansion enhances the patient experience by adding a new radiation vault to house a TrueBeam linear accelerator — an advanced system that delivers radiation therapy. While the capacity to treat people with cancer doubled, new technology brings more cutting-edge treatments to Paulding, alongside a modernized dressing room area offering patients more space and comfort.
Wellstar Paulding’s new linear accelerator also brings a leading-edge cancer treatment called stereotactic body radiation therapy (SBRT) to Paulding County for the first time.
“SBRT will transform cancer care in our community,” said Dr. Rakendu Shukla, Wellstar radiation oncologist. “In the coming months, we will roll out new treatments previously unavailable in Paulding.”
SBRT is different from conventional radiation therapy because it delivers very high, precise doses of radiation directly to tumors that are traditionally difficult to treat. It is more powerful at killing tumors, and it decreases the amount of radiation that healthy tissue is exposed to, which decreases side effects. And the treatment can be delivered over a short course of time — around 1-5 days rather than weeks or months.
The renovated space is located at Wellstar Paulding Medical Center’s Outpatient Pavilion at 148 Bill Carruth Parkway in Hiram, Georgia.
Pictured l-r: Don Zarkou, VP, Oncology Service Line, Wellstar Health System; Ralph Turner, SVP, Wellstar Health System, President, Wellstar Paulding Medical Center; Dr. Michael Andrews, Chief Cancer Officer, Wellstar Health System; Dr. William Thoms, Radiation Oncology Medical Director, Wellstar Paulding Medical Center; Sandy Kaecher, Post II Paulding Commissioner; Nichole Rydahl, AVP, Operations, Wellstar Paulding Medical Center; Shawn Jackson, Manager, Radiation Oncology, Wellstar Paulding Medical Center; Dr. Rakendu Shukla, Radiation Oncologist, Wellstar Paulding Medical Center.

Physicians and team members from the Wellstar Paulding Medical Center oncology team gathered for a ribbon cutting to celebrate the completion of a major expansion to cancer services.

Wellstar Paulding Medical Center’s new TrueBeam linear accelerator helps make cancer treatment more accessible to patients and brings a leading-edge cancer treatment called stereotactic body radiation therapy (SBRT) to Paulding County for the first time.
Lown Institute Recognizes Wellstar Among Most Charitable in the Country
A report by the Lown Institute ranking the value of nonprofit hospitals’ community investment found that Wellstar Kennestone Regional Medical Center and Wellstar Cobb Medical Center are among the top 25 hospitals in the nation providing significantly more community benefit than they are receiving in tax exemption.
Wellstar Kennestone ranked No. 1 in Georgia, while Wellstar Cobb was No. 2. Wellstar is the only health system with two hospitals included on the national top 25 list.
As the top provider of charity care in the state and one of the top 10 providers nationwide, Wellstar is committed to bringing expert, compassionate health services to those who need them. Last year alone, uncompensated and charity care at Wellstar exceeded $1.2 billion, providing care for at-risk and underserved communities across Georgia.
In addition to Wellstar Kennestone and Wellstar Cobb, Wellstar Douglas Medical Center, Wellstar West Georgia Medical Center, Wellstar North Fulton Medical Center, Wellstar Paulding Medical Center and Wellstar Spalding Medical Center were recognized for spending more on financial assistance and community investment than the estimated value of their tax exemptions.

Wellstar North Fulton Medical Center Completes 250 Procedures Treating Venous Thromboembolism
The peripheral vascular care team at Wellstar North Fulton Medical Center, a leading facility in the treatment of venous thromboembolism (VTE), has completed its 250th venous thromboembolism (VTE) procedure.
According to the American Heart Association, VTE is the third most common vascular diagnosis after heart attacks and strokes, and affects between 300,000 and 600,000 Americans each year. There are two types of VTE:
VTE can be fatal and can cause lifelong disability. Early intervention is crucial. At Wellstar North Fulton, the heart care team was an early adopter of a groundbreaking treatment for VTE, which uses a catheter to remove the clot. The healthcare provider inserts the catheter through the groin and navigates it to the clot for treatment.
“This has been a game changer in the treatment of this disease,” said Wellstar Cardiologist Dr. Ahsan Achtchi. “We’re seeing a lot less long-term disability and a lot less deaths in patients who come to the hospital with a blood clot.”
Wellstar North Fulton continues to receive referrals from around the region for this procedure and is one of the highest volume hospitals for VTE care in metro Atlanta.
Previous treatment options included open chest surgery, blood thinners and clot-busting medications. These methods posed a higher risk of complications, especially for patients who have recently undergone another surgical procedure. Because a recent surgery can put a patient at higher risk for VTE, using a catheter to remove the clot is safer for many patients. This new treatment method has reduced patients’ hospital stays for VTE from an average of five to seven days to only one or two days, according to Dr. Achtchi.
“Typically with this procedure, patients feel better almost immediately, and their recovery outside the hospital is a lot more complete and brisk,” he said.
If you or someone else is showing signs of VTE, seek emergency care as soon as possible.
Symptoms of VTE include:
Risk factors for VTE include not moving for a longer period of time—such as when someone is on bed rest following surgery—as well as some medical conditions, including diabetes, high blood pressure, blood clotting disorders or kidney disease. Your Wellstar provider can help you evaluate your risk of VTE and manage your risk factors.
Learn more about cardiovascular care at Wellstar North Fulton Medical Center.
Reducing Your Risk of a Stroke
While strokes have become relatively common—more than 795,000 people in the United States have a stroke each year, according to the Centers for Disease Control and Prevention—many risk factors for stroke can be managed in partnership with your healthcare provider.
Factors that can increase your risk of experiencing a stroke include:
Hypertension, or elevated blood pressure, increases the risk of a stroke. Stay up to date on your annual physicals to know your blood pressure levels, and if you have hypertension, talk to your provider about managing it. “High blood pressure is the most modifiable risk factor, meaning it’s the one that is most treatable and has the most impact on one’s risk,” said Wellstar Neurologist Dr. Ashis Tayal. “It is vastly underdiagnosed and when it is treated, it’s often undertreated.”
Elevated cholesterol can lead to plaque buildup in the blood vessel and clotting in the blood, which can cause a stroke if the clot travels and blocks blood flow to the brain. Your primary care provider can help you monitor your cholesterol with a blood test and manage levels with medications or lifestyle changes.
People with diabetes are at increased risk of experiencing a stroke. Talk to your provider about diabetes screenings. If you are diabetic, discuss managing the condition in partnership with your provider.
“Cigarettes accelerate atherosclerosis, or clogging in the arteries, and cause inflammation in blood vessels that then increases people’s risk of stroke and heart attack,” Dr. Tayal said.
Atrial fibrillation, a heart arrhythmia, can cause clots that then travel to the brain, leading to a stroke, according to Dr. Tayal.
While many of these risk factors can be controlled through medication or lifestyle changes in partnership with a healthcare provider, other risk factors for stroke are out of a person’s control. People of any age can experience a stroke, but stroke risk increases with age.
The risk of having a first stroke is nearly twice as high for Black adults as for white adults, and Black adults and Pacific Islander adults have the highest rates of death from stroke, according to the CDC. Hypertension is more common in Black patients, Dr. Tayal noted. People in rural communities may also experience higher rates of stroke due to limited access to healthcare and nutritious foods, he added.
To help lower stroke rates in our communities, Wellstar Community Health will distribute around 100 blood pressure cuffs in 2023 and educate community members about stroke risk and blood pressure monitoring at Wellstar Mobile Markets. The blood pressure cuffs can be used to monitor blood pressure at home so patients can work with their providers to take action against hypertension.
Learn the warning signs of a stroke, and if you notice any of these in yourself or someone else, be fast and call 911 right away.
Look for a sudden loss of balance or coordination. This can also appear as a sudden, severe headache or dizziness.
Blurred vision, double vision or loss of vision can be signs of a stroke. If you think someone else may be having a stroke, ask if they are having trouble seeing out of one or both eyes.
One side of the face may be feeling numb or appear to be drooping. Ask the person to smile and see if it appears uneven.
Check for sudden arm weakness or numbness. See if the person can lift both arms without one drifting downward.
Watch out for slurred speech or difficulty speaking. Ask the person to repeat a simple sentence to find out if they are having trouble talking.
The more treatment is delayed, the more the brain is damaged. Don’t wait to seek care. If you notice any of these symptoms, call 911 immediately.
Stroke prevention and the future of stroke care
Republished with permission of the Atlanta Business Chronicle
This article was originally published on
Atlanta Business Chronicle on May 19, 2023.
Stroke is the fifth leading cause of death in the United States. The Georgia Department of Public Health reports the state had the 12th highest stroke death rate in the country. Georgia is also part of the “stroke belt,” an area of the southeastern United States with stroke death rates 30% higher than the rest of the nation.
As the leading — but preventable — cause of disability, stroke can happen at any age.
Stroke is a medical emergency, meaning the blood flow to an area of the brain is cut off, depriving brain tissue of oxygen and nutrients. When this happens, brain cells start to die and abilities controlled by that area of the brain, such as speech or muscle control, are lost.
New drugs and new advanced treatments — such as the Tigertriever and Artemis — are helping reduce the death and disability impact of stroke, as well as comprehensive care programs and innovative hospital partnerships that expand stroke services into rural areas.
Physicians from Wellstar Health System and the CEO of a hospital in northeast Georgia joined Atlanta Business Chronicle to discuss stroke prevention and the future of stroke care.
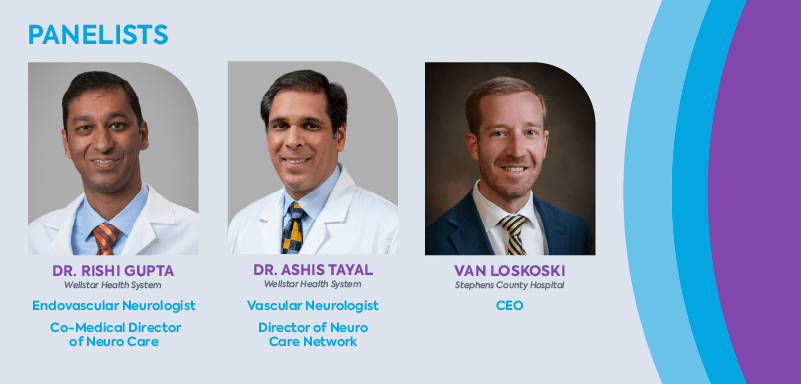
David Rubinger: Dr. Tayal, set the stage for us about the definition of stroke.
Dr. Ashis Tayal: A stroke is a sudden injury of the brain due to blockage or rupture of an artery in the brain. Injuries to the brain and disability can vary significantly.
The most common, ischemic stroke injury, is due to obstruction of an artery that causes a loss of blood flow to a critical part of the brain which damages the brain rapidly.
The other type of stroke is hemorrhagic stroke, where there’s a rupture of an artery, bleeding into the brain, or the surfaces of the brain, and that is called an intracerebral hemorrhage or a subarachnoid hemorrhage.
Rubinger: I think Americans have become a little better educated as to who’s at risk for stroke, but why don’t you walk us through that. Who would be a potential stroke candidate?
Tayal: High blood pressure, or hypertension, is the most common risk factor for both ischemic and hemorrhagic strokes. High blood pressure is an extremely common but controllable condition. Almost 80% of people have hypertension as they’re getting older.
Other risk factors include diabetes associated with elevated blood sugars causing accelerated blockage of arteries and high cholesterol, which can be related to diet and genetics.
Atrial fibrillation, a common heart arrhythmia that occurs as people get older, also places people at risk for the most severe and disabling types of strokes. And plaque buildup in specific arteries of the neck and brain also leads to an increased risk of stroke.
Smoking is another risk factor. Many adults still smoke despite a lot of progress in stroke treatment, and smoking puts people at risk for different types of stroke.
Rubinger: What about atmospheric things like stress and other areas like that? How does that play into it? Or do those things manifest themselves because of the other underlying physical conditions?
Tayal: I don’t view stress, in and of itself, as a risk factor for stroke. I think that’s more related to people’s environments and their own personalities and how they respond to stress. I do think people who are under undue stress can have poor lifestyle habits, and those poor lifestyle habits, whether poor eating habits, smoking, weight gain or lack of exercise, can lead to conditions that increase the risk for stroke.
Rubinger: So how is the healthcare system doing treating strokes? Do you believe that what’s going on at the primary care provider’s office is helping or do we have a way to go?
Tayal: In the United States, preventive care has improved the treatment of risk factors that lead to stroke, but communities must maintain routine checkups as many of the risk factors are silent.
There are improved treatments for hypertension, more aggressive treatment for diabetes, and more efforts at smoking cessation. Just the fact that we treat hypertension better than we did a generation ago has had a great impact on lowering the prevalence of stroke.
That being said, some of the most exciting work on stroke has often been done in the area of acute treatment of stroke with clot-busting drugs, catheter-based treatments and medications to protect the brain during an acute injury.
Rubinger: Has pharmacology gotten better in terms of the hypertension medicines that are out there? Have anti-cholesterol medicines improved in recent years?
Tayal: In the past, healthcare providers were often undertreating people with hyperlipidemia — high cholesterol — and not fully appreciating the benefits of significant reductions in cholesterol levels. For example, we’ve learned that driving cholesterol down into much lower ranges under 55 mg/dL can benefit our patients who have vascular disease as a cause for their stroke.
In the fight against high cholesterol, newer medications that prevent the absorption of cholesterol are now available. Recent developments have led to the discovery of a new underutilized class of drugs called PCSK-9 inhibitors that are highly effective.

Wellstar Commemorates Breast Cancer Awareness Day with Atlanta Braves
Wellstar was honored to partner with our hometown team, the Atlanta Braves, for Breast Cancer Awareness Day at Truist Park on Sunday, May 7, against the Baltimore Orioles.
Wellstar breast cancer survivors were recognized during a pre-game brunch, as well as on the field before the first pitch. Braves fans were also invited to join Wellstar for festivities to raise awareness of breast cancer with special guest, NBA Hall of Famer and Wellstar Ambassador Dominique Wilkins.
At Wellstar, we believe breast cancer takes a team approach. Our experts across all our specialties coordinate care with a patient-centric focus. We collaborate with providers specializing in primary care, women’s health, imaging, oncology and surgery to provide comprehensive, timely care.
Thank you to Braves fans for celebrating breast cancer survivors with us and encouraging those you love to schedule their annual screenings.
Early detection is crucial in breast cancer care. Screening for breast cancer at regular intervals can help catch it earlier — before symptoms appear — for better treatment outcomes. Call (678) 581-5900 to schedule your mammogram now, and visit wellstar.org/catchitearlycare to learn more.

Wellstar Kennestone Regional Medical Center Receives Highest Marks for Patient Safety
Wellstar Kennestone Regional Medical Center has been recognized with an “A” Hospital Safety Score by The Leapfrog Group, an independent national nonprofit run by employers and other large purchasers of health benefits. The Leapfrog Hospital Safety Grade is a letter grade assigned to U.S. hospitals based on data calculated using 26 measures evaluating the hospital’s overall capacity to keep patients safe from infections, injuries, and medical and medication errors.
“Patient safety is at the forefront of everything we do at Kennestone, and we are pleased to be recognized by the Leapfrog Group for earning an A grade,” said Callie Andrews, Wellstar Kennestone Senior Vice President and Chief Operating Officer. “Not only does an A grade affirm the high quality of care that we deliver to our patients every day, but this prestigious ranking also honors the critical role that our physicians, nurses and caregivers play in keeping our communities healthy and safe.”
The Hospital Safety Score was compiled under the guidance of the nation’s leading experts on patient safety. The first and only hospital safety rating to be peer-reviewed in the Journal of Patient Safety (April 2013), Hospital Safety Score is designed to give the public information they can use to protect themselves and their families.
To see how Wellstar Kennestone’s scores compare nationally and locally, visit the Hospital Safety Score website at www.hospitalsafetyscore.org, which provides information on how the public can protect themselves and loved ones during a hospital stay. Local hospitals’ scores are also available on the free mobile app, available at www.hospitalsafetyscore.org.
Wellstar Health System Partners with Georgia State University to Increase Respiratory Therapy Student Enrollment Through Wellstar Foundation Grant
Wellstar Health System and Georgia State University’s Department of Respiratory Therapy in the Byrdine F. Lewis College of Nursing and Health Professions announce a $320,000 grant to expand the pipeline of respiratory therapy (RT) professionals.
"Respiratory therapists are a vital part of the care team and are in critical demand – a trend exacerbated by the COVID-19 pandemic and felt throughout the healthcare industry," said Julie Teer, president of the Wellstar Foundation. "The Wellstar Foundation is proud to increase the workforce pipeline by collaborating with and funding Georgia State to hire an additional faculty member to lead a new clinical cohort of RT students at Wellstar Kennestone Regional Medical Center."
The faculty shortage is a major barrier to increasing program enrollment and adding this position will result in a 20 percent increase in the program’s enrollment capacity.
"Highly educated respiratory therapists will always be needed, but due to the pandemic and the burnout of healthcare practitioners, the job market is wide open for new graduates," said Dr. Doug Gardenhire, chair of the Department of Respiratory Therapy.
Over 150,000 respiratory therapists work in the United States, and 92,000 are likely to retire by 2030. In addition to faculty shortage, demand for professionals that outpaces the capacity of degree programs also contributes to the national shortage of respiratory therapists. According to the U.S. Bureau of Labor Statistics, the number of RT positions will grow by at least 19 percent through 2029 due to an aging population and increased cases of respiratory illness.
"There are more than 17,000 advertisements for needed respiratory therapy positions around the country, and the need is no different in metro Atlanta," said Gardenhire. "This partnership with Wellstar allows us to educate and graduate more baccalaureate and master’s degree prepared respiratory therapists."
Georgia State’s RT program is one of only two U.S. programs to receive the American Association for Respiratory Care Apex Award for three consecutive years. The award recognizes respiratory care in clinical care facilities and educational programs that highlight best practices with evidence-based medicine. Over the past decade, every Georgia State RT graduate has earned a 100 percent pass rate on the licensure exam.
"This grant helps strengthen our relationship with Wellstar and will bring more of our students into the Wellstar system for clinical practice and potentially for employment after graduation," said Dr. Huanbiao Mo, dean of the Lewis College. “Congratulations to RT faculty and leadership for forging this successful clinical partnership."
Explore how the Lewis College at Georgia State is producing respiratory therapists and other professionals prepared for the frontlines of healthcare at lewis.gsu.edu. See how corporate and foundation partner and individual donor dollars are making a difference at Georgia State at giving.gsu.edu. Learn how Wellstar Foundation, through philanthropy and partnership, is making a meaningful difference in the health of our communities at wellstar.org/foundation.

Wellstar Foundation Gala Raises Over $1M for Pediatric Services


Wellstar Mobile Markets Highlighted on WSB-TV Game Changers and People 2 People
Wellstar Mobile Markets were featured April 26 on WSB-TV Game Changers, a Family 2 Family Special, and on People 2 People on May 14. Wellstar Center for Health Equity and the Wellstar Community Health team are working with community partners Goodr and Wholesome Wave Georgia, along with a special volunteer, former Atlanta basketball star and Wellstar Community Ambassador Dominique Wilkins, to distribute nutritious, free food and health screening education to support the well-being of our communities. Community host sites have included partners such as C.H.O.I.C.E.S. and Roswell Organization for Community Development.
Through the mobile markets, Goodr provides fresh produce, meat, shelf-stable items, milk and other beverages. In addition, a benefit specialist from Wholesome Wave Georgia, another nonprofit increasing access to healthy foods, helps connect families with additional resources.
Learn more and find a market near you at wellstarmobilemarket.com.
Watch the WSB-TV People2People Interview.

Wellstar Celebrates Earth Day with Programs Addressing Food Waste
For Earth Day this year, Wellstar Health System is making a difference for our environment and supporting our neighbors facing food insecurity. The recently launched Organic Recycling Program at the Wellstar Corporate Office (WCO) in Marietta has already diverted almost one ton of food waste from landfills, preventing over 675 pounds of carbon dioxide emissions.

Wellstar Executives Named 2023 Black Healthcare Leaders to Know
We know what makes Wellstar special – our people. It’s evident that people outside of our organization recognize that, too. Recently, we were able to celebrate four Wellstar leaders highlighted in Becker’s 2023 Black Healthcare Leaders to Know.
When we have leaders from diverse backgrounds, we have greater insight into the lived experiences of our team members, patients and communities. We help mitigate our blind spots, grow in compassion and empathy, and build a stronger organization. This leads to more personalized care, improved patient outcomes and a more inclusive place to work.
Join us in congratulating our four recognized leaders: Le Joyce Naylor, Senior VP and Chief Diversity, Equity and Inclusion Officer, David Jones, Executive Vice President and Chief Human Resources Officer, Mary Chatman, RN, PhD, Executive Vice President of Acute Care Operations and President of Wellstar Kennestone Regional Medical Center and Wellstar Windy Hill Hospital, and Ralph Turner, Senior Vice President of Wellstar Health System and President of Wellstar Paulding Medical Center. Read their bios below.
Le Joyce Naylor: Senior Vice President and Chief Diversity, Equity and Inclusion Officer at Wellstar Health System
Le Joyce Naylor offers systemwide thought leadership, strategic thinking and program direction for Wellstar Health System's diversity, equity and inclusion initiatives. Her responsibilities include the design and implementation of programs to advance diversity efforts, achieving measurable outcomes and leading the health system's diversity and inclusion advisory council. Among her many accomplishments are the formation of 11 business resource groups, the recalibration of 11 diversity and inclusion councils and the implementation of Inclusion Cafés, an experience designed to enhance team member connection. She also leads efforts for team members to engage in inclusive virtual and in-person programming to advance cultural competence, humility, and personal development.
David A. Jones: Executive Vice President and Chief Human Resources Officer at Wellstar Health System
David A. Jones has overall responsibility for establishing, enabling, and maintaining organizational effectiveness and a positive employee and labor relations environment across Wellstar Health System. He creates and preserves positive relationships between employees and management throughout the 9-hospital system. Jones is an instrumental leader, equipping caregivers on the front lines with the resources needed to deliver world-class healthcare. Additionally, he believes that every team member should find joy in the workplace – it is his mantra. While keeping joy at the forefront of his mind, he leads critical initiatives to enhance the workplace dynamics of the more than 24,000 team members who are united around enhancing the health and well-being of every person they serve.
Mary Chatman, RN, PhD: Executive Vice President of Acute Care Operations and President of Wellstar Kennestone Regional Medical Center and Wellstar Windy Hill Hospital
Mary Chatman's leadership and collaborative work ethic can be seen throughout the health system. She is a seasoned leader with 32 years of healthcare experience. Having begun her career as a nursing assistant, Chatman is committed to providing patient-centered care and implementing effective operational strategies. She manages a team of more than 10,000, including finance, human resources, nursing, operations, and medical staff. A visionary leader, she led the charge for the 2020 opening of the Southeast’s largest emergency department at Wellstar Kennestone Regional Medical Center, which was designed to further enhance emergency and Level II trauma care for Georgians.
Ralph Turner: Senior Vice President of Wellstar Health System and President of Wellstar Paulding Medical Center
As senior vice president of Wellstar Health System and president of Wellstar Paulding Medical Center, Ralph D. Turner serves as the operating and strategic leader of a 112-bed inpatient facility, as well as its 49-bed emergency department, Level II Trauma Center, comprehensive cardiology services, oncology care, general surgery, neuro care, orthopedics, robotics and urology, as well as an inpatient rehabilitation program and comprehensive cardiac rehabilitation. Turner is responsible for leadership and management for all aspects of operations, including financial performance, clinical quality, employee, physician and community relations. He also oversees more than 1,330 team members as they pursue Wellstar’s vision of delivering world-class care to every person, every time.
Congratulations to our leaders!

Celebrate Cancer Survivors Day with Wellstar
Wellstar Health System supports people with cancer throughout their journeys, from early screening to diagnosis to treatment. However, our encouragement and dedication to delivering world-class, compassionate care doesn’t end in remission.
Across our system, Wellstar honors the bravery and strength of survivors every day, rejoicing in each milestone. This National Cancer Survivors Day, we are proud to pay tribute to people who have conquered cancer while offering hope to those still fighting. This year’s Cancer Survivors Day theme, “Cruising Toward Survivorship,” exemplifies Wellstar’s commitment to being a steadfast source of encouragement for cancer survivors and fighters across Georgia.
“Cancer Survivors Day gives us the opportunity to pause, reflect and cherish victories over cancer. It also provides an outpouring of support to people currently fighting cancer, so they know they are never alone,” said Nicole Centers, executive director of the oncology service line & nurse leader at Wellstar.
Several Wellstar facilities will host Survivors Day events — and you can be a part of the celebration.
Wellstar Cobb Medical Center
Wellstar Kennestone Regional Medical Center
Wellstar Douglas Medical Center
Wellstar West Georgia Medical Center
RSVP by contacting Sarah Hersey at (706) 845-3848 or [email protected]
Wellstar Paulding Medical Center
Wellstar North Fulton Medical Center
RSVP by contacting Pam Plasket at (770) 410-4556 or [email protected]

Wellstar Health System Partners with CLEAR to Empower Patients to Take Control of their Health Information & Enhance the Consumer Experience
Wellstar Health System, one of the largest and most integrated healthcare systems in Georgia, is collaborating with CLEAR, the secure identity company, focused on optimizing Wellstar consumers’ digital and physical healthcare experiences. Wellstar will embed secure identity verification Powered by CLEAR technology to provide patients with secure and easy access to their personal health information.
Using the Powered by CLEAR platform will provide a seamless and secure experience by eliminating the need for patients to manually re-enter biographic data with each interaction. Wellstar expects the partnership with CLEAR will save patients time, reduce help desk calls and operational costs, improve security, lower fraud risk, and drive consumer adoption and engagement across the health system’s digital ecosystem.
“This exclusive partnership will open the door to new innovations that make accessing care easier and experiences curated in the moments people need them most,” said Hank Capps, M.D., FAAFP, Wellstar’s Executive Vice President and Chief Information and Digital Officer. “As we continue to build future care models that blur digital to brick and mortar experiences, we need advanced capabilities and constant innovation. We are excited to roll-up our sleeves with CLEAR and design that future together.”
“CLEAR’s partnership with Wellstar marks another important step as we work to replace the clipboard and improve the patient experience,” said Caryn Seidman-Becker, CEO of CLEAR. ”We’re excited to power safer, easier experiences - physically and digitally - for Wellstar patients across their healthcare journey.”
Catalyst by Wellstar, a first-of-its-kind innovation company and venture firm, will support the partnership with CLEAR to accelerate innovation.
Powered by CLEAR enables frictionless confirmation of your identity and credentials to make everyday experiences safer and easier – transforming the way people live, work, and travel. Whether CLEAR’s 15 million members are networking online, visiting a doctor, checking into a hotel, renting a car, or cheering on their favorite sports team, they can frictionlessly affirm their identity with CLEAR — for free — wherever life takes them. New users can simply enroll once to verify anywhere in our Powered by CLEAR network.
In Georgia, CLEAR operates its signature expedited identity verification lane at Hartsfield–Jackson Atlanta International Airport (ATL). CLEAR also operates a free, dedicated entry lane at State Farm Arena to help fans get into games and events faster.

Wellstar Team Members Voted Best of Cobb
The care teams at Wellstar are dedicated to enhancing the health and well-being of everyone we serve, and we thank our team members for their commitment to world-class care. We also thank Cobb residents for
trusting the expertise of Wellstar to keep their families healthy and provide them with more than healthcare, PeopleCare.
Several Wellstar team members have been voted among the Best of Cobb:

Wellstar North Fulton Medical Center Opens New Comprehensive Cancer Center
Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, announced the grand opening of the Wellstar North Fulton Cancer Center on the Wellstar North Fulton Medical Center campus in Roswell, Georgia on March 27. The Center will serve as one of only two locations in metro Atlanta featuring state-of-the-art CyberKnife® technology for radiation therapy, a noninvasive treatment for cancerous and non-cancerous tumors and other conditions where radiation therapy is needed.
The Cancer Center will now offer comprehensive cancer services, including medical oncology; radiation oncology; imaging and many medical specialties from nationally recognized, expert and experienced physicians all in one convenient location.
“With this beautiful new $12 million state-of-the-art Comprehensive Cancer Center, we can offer people in our community some of the most advanced cancer treatments close to home,” said Jon-Paul Croom, president of Wellstar North Fulton Medical Center. “People will be able to come to the 12,000-square-foot Wellstar North Fulton Cancer Center for almost all aspects of diagnosis, staging and treatment, with surgery across the way at the hospital.”
Wellstar team members and the Roswell community celebrated the official opening of the Cancer Center last week with a ribbon cutting ceremony following ten months of construction. Attendees had the opportunity to tour the facility and Wellstar’s second CyberKnife system, newly housed at the Cancer Center.
Wellstar first began using the CyberKnife System at Wellstar Kennestone Regional Medical Center in 2006 to treat conditions throughout the body and can be an alternative to surgery or for patients who have inoperable or surgically complex tumors. CyberKnife can reduce radiotherapy timelines from the traditional eight weeks to as little as one to five days.
“We are committed to providing the best treatment options for our patients and are proud to bring the CyberKnife system to this community,” said Dr. Mark McLaughlin, radiation oncology medical director for Wellstar North Fulton Medical Center. “With the state-of-the-art CyberKnife technology, we can deliver high precision radiation in fewer radiotherapy sessions with the goal of making treatment easier and improving outcomes for patients. We look forward to continuing to help patients beat cancer and celebrate their futures.”
The multidisciplinary team of cancer experts onsite will offer patients a high level of knowledge and expertise, along with compassion and hope. The multi-disciplinary physician experts at Wellstar North Fulton Cancer Center include:
Learn more about Wellstar North Fulton Cancer Services.
To learn more about the CyberKnife System, please visit cyberknife.com.

CyberKnife technology

9 Things You Need to Know About Type 2 Diabetes
According to the Centers for Disease Control and Prevention (CDC), about 1 in 10 Americans have diabetes. Of that group, 90 to 95% have type 2 diabetes. Because this condition often develops in people over 45, getting screened and getting the best treatment to live your healthiest life is essential.
"Diabetes is a chronic and complex condition, and treatments are continuously changing," said Dr. Georgia Forrest, Wellstar primary care physician. "Teaming up with a primary care provider who personalizes your care plan to you and everything that makes you unique should be a top priority."
Whether you currently have type 2 diabetes, a family history of the disease or feel concerned about your overall well-being, you can take proactive steps to manage your health. Here are some key facts to help you better understand the relationship between diabetes and good health.
1. Undiagnosed diabetes costs you money & health
Not knowing you have diabetes carries high medical costs. Undiagnosed diabetes can increase your risk for death and other medical issues.
Diabetes was the eighth leading cause of death in 2021, the most recent data reported by the U.S. Preventive Services Task Force. And according to the American Diabetes Association, having diabetes doubles your risk for heart disease and stroke—heart disease is the number one killer in the U.S.
2. A diagnosis and personalized treatment can save your life
Knowing you have diabetes and then working to manage your blood sugar, blood pressure and cholesterol effectively can lower your risk of death and help you live a better quality of life.
3. Getting screened for diabetes is easy
The U.S. Preventive Services Task Force now recommends getting screened with a simple blood test at the age of 35 for people with no symptoms but who are overweight or obese. Even if you have no signs or family history of diabetes, it can lurk in your numbers. Getting screened can help you catch it early and even prevent it altogether.
Consider getting screened for diabetes if you:
4. Some people have pre-diabetes
If your screening shows that you have pre-diabetes, your blood sugar levels run higher than average but aren't within the range of type 2 diabetes. However, you have an increased risk of getting type 2 diabetes.
Identifying that diabetes is around the corner can help you stop it before it starts.
5. Diabetes treatment plans should be unique
When crafting a plan to address diabetes, the conversation must be about more than the numbers.
"Additional diseases or conditions you may be experiencing in conjunction with your diabetes should also become part of your individualized health plan," Dr. Forrest said.
A complete medical history helps your healthcare provider understand how other medications and treatments may interact with your symptoms and treatments related to type 2 diabetes.
6. Lifestyle modifications can make a big impact on diabetes
Lifestyle modifications may involve slight changes to your weight, the amount of exercise you get, your diet and even your sleeping patterns.
Changes don't have to be major. For instance, your doctor may suggest you lose around 10 pounds and exercise for 30 minutes five days a week.
Our primary care providers work with patients one-on-one but can also refer patients with pre-diabetes and diabetes to Wellstar Diabetes Services to help prevent the onset or manage the effects of diabetes.
7. S.M.A.R.T. diabetes treatment plans
According to Dr. Forrest, your overall plan should include "specific, measurable, achievable, relevant and timely (S.M.A.R.T.) goals and involve shared decision-making between you and your care provider. There should be plenty of follow-ups to keep the conversation fluid and open to modification."
8. Know your numbers — and acronyms (A1C, CGM, TIR)
Should your screening lead to a type 2 diabetes diagnosis, conversations with your health providers will focus on several acronyms and numbers.
"Know your ABCD’s of diabetes," said Dr. Forrest. "Your A1C, blood pressure, cholesterol and the medications you are taking. Knowing these facts about your health will be key to your success."
• A = Hemoglobin A1C goal is <7
• B = Blood pressure goal is <130/80
• C = Cholesterol goal is to keep bad cholesterol <100
• D = Drugs
Keeping the A1C low and within an optimal range will help prevent complications like eye damage, blindness, kidney failure and nerve damage.
A mainstay for type 2 diabetes management centers around constant glucose level monitoring. Continuous glucose monitoring (CGM) provides readings every few minutes via a sensor inserted just below your skin. Monitoring glucose is a common way to help regulate insulin in your body, giving you the readings you need to self-adjust with insulin when appropriate. Average glucose levels should be 100 mg/dl or lower though they can increase if you've just eaten.
New developments introduced the importance of tracking Time in Range (TIR). Along with monitoring your glucose levels, TIR may impact your customized plan for maintenance. According to Dr. Forrest, the goal for TIR is 70% or more.
9. Receive individualized diabetes care at Wellstar
For diabetes management, a personalized, proactive approach can make all the difference. Wellstar primary care providers are here to partner with you to help prevent or manage diabetes, heart disease and many other conditions.
"A true patient-centered approach for managing diabetes is the key to the future of this disease," Dr. Forrest said. "Get screened and speak up when it comes to your care. Opportunities for personalized and individualized medicine should be a part of your treatment plan as you move forward."
Find a primary care provider near you.

Women’s History Month Event Honors Impact of Female Leadership and Mentorship
On March 8, Wellstar’s Office of Diversity, Equity and Inclusion hosted a fireside chat with leaders, Beth Kost, Kem Mullins and Julie Teer, who also serve as Executive Sponsors to our Women’s Business Resource Group. They engaged inn an important conversation about celebrating women in the workplace. Focusing on the national theme for Women's History Month, "Celebrating Women Who Tell Our Stories," they discussed women who have positively impacted their careers, the importance of mentorship and sponsorship, and advice they would give to female leaders of the next generation.
Kost is senior vice president and chief compliance officer of Wellstar, Mullins is executive president of ambulatory and business development, and Teer is senior vice president and president of the Wellstar Foundation.
Women's History Month celebrates the contributions of women, past and present. President Jimmy Carter instituted the first National Women's History Week in March 1980. He said, "From the first settlers who came to our shores, from the first American Indian families who befriended them, men and women have worked together to build this nation. Too often, the women were unsung and sometimes their contributions went unnoticed. But the achievements, leadership, courage, strength and love of the women who built America was as vital as that of the men whose names we know so well." On March 8, we joined the world in celebrating International Women's Day and incorporate it into our month-long celebration of women's history.
Learn more about diversity, equity and inclusion at Wellstar.
Watch the virtual event below.

Black History Month Event Celebrates Excellence, Looks to Future
On Wednesday, Feb. 22, Wellstar’s Office of Diversity, Equity and Inclusion partnered with the African American/Black Business Resource Group, B.R.A.V.E., to host an engaging conversation between Dr. Khalil Gibran Muhammad, the Ford Foundation Professor of History, Race and Public Policy at the Harvard Kennedy School, and Dr. Hank Capps, Wellstar executive vice president and chief information and digital officer and B.R.A.V.E. Executive Sponsor. Focusing on “Honoring the Past, Celebrating the Present, and Inspiring the Future,” they discussed wrestling with the fundamental contradictions of our country’s past, addressing bias and holding unflinchingly to science and facts.
"Black History Month allows all individuals to reflect on the power of diversity, equity, inclusion and belonging in every facet of American culture. It is a time to understand and reflect upon Black stories of joy, pain and triumph. It is a time to come together to honor the great achievements of Black individuals, acknowledge and appreciate their many contributions to our society, both past and present, and to celebrate Black excellence," said Wellstar’s SVP and Chief Diversity, Equity and Inclusion Officer, Le Joyce Naylor.
Watch a portion of the program below.

Wellstar Partners with Goodr to Launch Mobile Grocery Store to Address Food Insecurity
Wellstar Health System is proud to announce that Goodr, a sustainable food waste management and hunger relief company, just unveiled Goodr Mobile Grocery Store on March 8 at Atlanta City Hall. Wellstar is proud to sponsor this 26-foot truck stocked with grocery items, including fresh produce, milk, eggs, and shelf-stable items – all for free. The truck aims to bring Goodr's signature free grocery shopping experience to food-insecure communities.
Fully kitted with refrigerators, freezers, and shelving, families will enjoy an experience much like shopping for goods at a local grocery store. Beyond that, every aspect of the Mobile Grocery Store is about access – from the wheelchair ramp to the resource room for private health screenings or social services consultation.
Wellstar’s Community Health Needs Assessments identified food insecurity as a key social determinant of health impacting the well-being of the communities we serve across the state in both 2019 and 2022. In late 2020, Wellstar joined the Goodr partner network and launched the Wellstar Mobile Markets, a uniquely branded variation of the pop-up grocery markets. The Mobile Markets have reached communities in metro Atlanta and beyond.
“I’m honored to represent Wellstar Health System, the Wellstar Foundation, and our generous donors who have helped make this vision, the Goodr Mobile Grocery Store, a reality,” said Julie Teer, SVP, Wellstar Health System, and president, Wellstar Foundation. “At Wellstar, we truly believe each and every person deserves to live their healthiest life, regardless of their circumstances. And, for a person to live their healthiest life, they need sustainable access to fresh, nutritious food.”
Wellstar is incredibly excited for this next chapter in our partnership with Goodr, and we are honored to be the exclusive healthcare partner and sponsor for this new and innovative way to serve communities.
To truly improve the overall health of our communities, it will take all of us working together to address the social determinants of health. The Goodr Mobile Grocery Store is a perfect example of what we can achieve when we work together.
Wellstar has been dedicated for the past 30 years to making Georgia a healthier place for everyone, and it is because of philanthropy that we are able to reinvest in the communities we serve. We appreciate the opportunity to partner with Goodr to offer these critical resources to more people through the Goodr Mobile Grocery Store, and we are excited to see how our organizations can continue to work together to further improve the health of our communities.

Finding better ways to fight heart disease and accelerate cardiac care progress
Republished Content: Atlanta Business Chronicle
This article was originally published on Atlanta Business Chronicle on February 9, 2023.
Cardiovascular disease is the leading cause of death in the United States, claiming more lives than all forms of cancer combined. Heart disease and stroke are among the forms of cardiovascular disease. In 2019, nearly 900,000 people died of cardiovascular disease in the United States, according to the American Heart Association. In Georgia, about 1 in 3 deaths are caused by cardiovascular disease, according to the Georgia Department of Public Health. Most of these deaths are premature and preventable. Atlanta Business Chronicle recently talked with a panel of experts from Wellstar Health System and the American Heart Association about ways to accelerate heart care progress through diversity and inclusion and finding better ways to fight heart disease through unconventional methods, early detection and education and through the workplace.
Moderator: David Rubinger, Market President & Publisher, Atlanta Business Chronicle
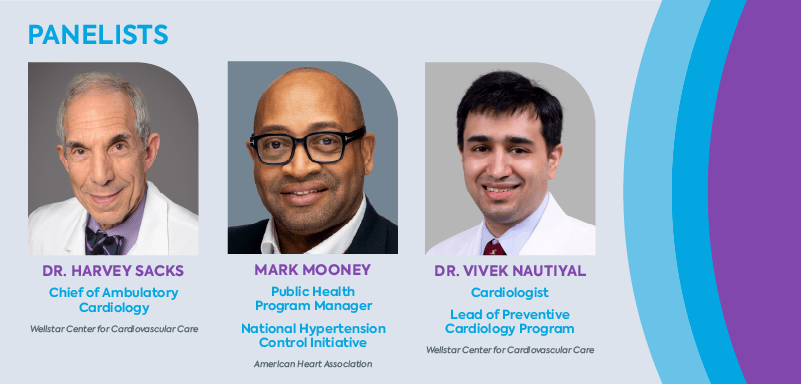
Rubinger: What is the best way to define heart disease? And what does it mean for our culture?
Dr. Vivek Nautiyal: Let me start by saying that heart disease or cardiovascular disease is a very broad term which include a wide variety of conditions affecting our heart and blood vessels. The most common type is coronary artery disease, which is usually caused by cholesterol plaque clogging the arteries, supplying blood to our heart. This is the number one cause of death in the U.S. and across the world.
Some other types of heart disease include heart failure, which affects the heart muscle pump, heart valve disease and heart rhythm disorders affecting electrical activity of the heart. Vascular disease includes aortic aneurysm, and disease affecting neck arteries going to the brain or arteries going to the legs. All of these would broadly come under heart disease.
These conditions affect the ability of the heart to function properly and can lead to serious health problems such as heart attacks or stroke.
Rubinger: How much of that would we consider to be genetics and how much would we consider to be lifestyle, leading to the disease itself?
Nautiyal: Genetics is important, but I would say the vast majority are lifestyle-related. And that is why it's killing so many people. Heart disease is often the result of lifestyle factors like poor diet, lack of exercise, mental stress.
About 4 in 10 U.S. adults currently are obese; 3 in 10 have high cholesterol; 4 in 10 have hypertension; 1 in 10 have diabetes. So, this is an epidemic. Adolescent and childhood obesity is on the rise and we in Georgia are sitting in the diabetes belt of the U.S.
Lack of awareness of these common risk factors often leads to delay in seeking preventive or medical care. You can have hypertension, high cholesterol, and diabetes for years or decades without knowing, which is why they're called silent killers. Unless you check for them, you may be blissfully unaware of your risk, until one day it leads to a major event.
Rubinger: It's very common to hear about examples where sometimes it can be genetic and other times it can be a lifestyle cause. Dr. Sacks, in your career, how have you viewed this whole conundrum of how to best approach heart disease?
Dr. Harvey Sacks: Getting back to your previous question, one form of heart disease we did not mention is congenital heart disease—malformations of the heart and blood vessels which occur at birth. As regards to lifestyle, when I started practicing cardiology, I saw patients in Paulding County. At that time, it was a rural community, but it is not so rural anymore but rather an extension of Atlanta. Many members of that community had a lifestyle consisting of poor dietary habits, lack of exercise, cigarette smoking and use of smokeless tobacco.
We began an educational process to teach people about healthy living. We socialized this into the community by giving talks to schools, churches and Rotary Club meetings.
The community bought into these new concepts, and we have made great progress. We have made significant changes as a result of this education in heart attack rates and cardiac mortality in that community.
Rubinger: Do we have any data to support that?
Sacks: We do. Since we have been seeing patients in Paulding County, data show a decrease in cardiac mortality. People understand the risk factors that contribute to the development of heart disease. And this trend is not unique to Paulding County. Similar efforts have been successful throughout the country. The American Heart Association (AHA) has helped us educate millions of people, and as a result, people are adopting healthier choices.
Rubinger: From a medical standpoint, what have you learned from research that has helped deliver better outcomes?
Nautiyal: As Dr. Sacks was mentioning, we have made huge advancements in improving cardiovasular mortality and morbidity, especially in the Medicare population. There's clear evidence of that in the last two decades. One area where we are lagging behind is in the young population. Unlike the older population, in the younger population the event rates are either flat or going up.
One of the reasons for this is that traditional risk factor calculators tend to underestimate cardiovascular risk in young people. By young people, I mean below 50. So, if you are below 50 and you have family members who had premature events or if you have very high cholesterol, or if you are a woman with certain complications during pregnancy, then be aware that traditional risk factors will underestimate your cardiac risk. Also, younger people tend to have this sense of invincibility. You don't have any symptoms. You think, “I’m doing OK,” not realizing that silently, processes are going on in your body which one day will lead to a catastrophic event.
As part of an NIH-funded four-year study, led by the Mayo Clinic, we at Wellstar are implementing a shared decision-making electronic tool called CV Prevent Choice in our primary care offices. This enables the patient and physician to have a discussion about their personal risk for heart attack over next 10 years. It shows in an easy-to-understand graphic the impact of lifestyle measures, like healthy diet and exercise and—if needed—medications, in reducing their cardiac risk. We collaborated with the Mayo team to include factors on this risk calculator, like family history, women-specific risk factors and coronary calcium score, which alerts the clinician and patient that actual risk may be higher than indicated.
Another area where we in the U.S. lag behind is utilization and adherence to easily available life-saving therapies. A recent study showed that in over 600,000 commercially insured patients with established cardiovascular disease in the U.S., the utilization of appropriate, life-saving medications, such as statins, was low, despite overwhelming evidence of the benefit and established clinical guidelines. Only 1 in 5 patients received appropriate high-strength statins, despite these being relatively inexpensive generic medicines. Younger patients and female patients were less likely to receive these therapies. Furthermore, patient adherence, as measured by prescription refill rates, was low.
To better understand some of the factors behind this and also improve our quality of care, we at the Wellstar Center for Cardiovascular Care are honored to have been chosen by the American Heart Association, to be 1 of 6 healthcare organizations across the country to participate in an integrated cardiovascular cholesterol management initiative, a learning collaborative grant. As part of this initiative, we will track patients admitted with heart attacks and follow them as they transition home. We will pilot programs to get patients to their treatment goals within a short time after discharge and improve patient outcomes.
Rubinger: Mr. Mooney, why aren’t people taking their statins? Is this part of the problem? Are people making bad decisions based on lack of education about what the risk factors are?
Mooney: There are a lot of factors that play into why patients are not adhering to taking statins or medications. Some of those barriers are health literacy, access to healthcare, and the affordability of medications. The expansion of Medicaid could address some of these factors. We at the American Heart Association are supporting the states that are advocating for Medicaid expansion.
Rubinger: What have been the major technological changes that have really made your jobs more effective or easier?
Sacks: There are different kinds of technology. One type is the evolution of the treatment of coronary heart disease. We are not only able to diagnose blockages in coronary arteries, but in a large proportion of the patients we can treat them with stents, reserving surgery for more extensive and complex heart disease. We are treating patients with valve abnormalities without having to open their chests, thus providing a much less invasive procedure.
A spot on the lung, or pulmonary nodule, is sometimes found incidentally on a CT which was ordered for another reason. We have an AI (artificial intelligence) program to follow and surveil these nodules for the possible development of lung cancer. And in addition, some of these patients have been found to have enlargement of their aorta (known as an aortic aneurysm). AI can identify these patients from a narrative report. They can then be referred to medical and surgical specialists for treatment. This helps prevent an otherwise fatal event from rupture of the aneurysm.
The other part is virtual visits. We believe that virtual visits are the future. There are so many people who for many, many reasons cannot come in to see the doctor, whether it's a transportation issue, whether it's having childcare, finances, whatever it may be. We want to bring those technologies to the person when they can't come to us. We believe that we can really influence people's lives greatly by being able to do that technologically by virtual visits.
Rubinger: And virtual medicine was something really born out of the pandemic. Is the concept of virtual medicine here to stay, Dr. Nautiyal?
Nautiyal: I believe so. The idea was there before, but the pandemic forced us into implementing it a very short time span. Now I think it's going to stay, but in a hybrid model. In-person conversation and physical exams still have meaning in spite of all the technology. An example of a hybrid model would be if someone was hospitalized recently for heart failure and now needs frequent visits for adjusting medications, they don't have to come in every time. We can do virtual visits to adjust the medications and get them to their goal.
Sacks: Psychological ill health can be as important as physical disease. Wellstar has introduced a Cardiovascular Behavioral Health program which can in part be virtual. It integrates behavioral health with physical wellbeing. We can help patients identify emotional problems which can contribute to physical maladies. Obesity is a prime example.
Obesity is often stigmatized, but it is actually a disease. And when you recognize it as a disease, you can treat it as such, similar to how we can treat other conditions. We can do a lot of this support virtually. We also have medications to curb obesity and even surgery for complex cases. If we eliminate the stigma associated with certain conditions, we can better treat them. We need to recognize emotional triggers which can lead to physical medical issues.
Rubinger: You mentioned earlier younger people who may think they’re invincible. These are the people who need to learn about early detection, earlier on in their lives. What is the recommendation you all give to the younger population to start monitoring their own heart health to know whether they need help? What are the steps younger people need to take to make sure they are addressing these issues?
Nautiyal: I would like to highlight two key groups who are at a very high personal risk of heart attacks or strokes. One is familial hypercholesterolemia. This is a genetic condition where you have high cholesterol levels since early childhood. The way to identify this is to know your cholesterol numbers and know your family history. Familial hypercholesterolemia, FH for short, is not as uncommon as we thought. One in 250 people have FH, and only about 20% of people with FH have been identified or recognized. This leaves a vast reservoir of undiagnosed and undertreated people. If you are a man with untreated FH, there is a 50% chance of having a heart attack by age 50, that is basically a coin flip. Women with untreated FH have a one in three chance of having a heart attack by age 60.
The second group is people with family history of premature heart attacks or strokes.
If you are in one of these two groups, I would strongly urge you to seek preventive cardiology consultation.
Regardless of whether or not you belong to one of these two groups, I cannot emphasize enough the importance of following a heart healthy dietary pattern, exercising regularly, not smoking, getting adequate sleep and knowing your numbers—blood pressure, cholesterol and sugar levels.
On a positive note: know that your DNA is not your destiny. If you treat FH adequately early on in life, you can have a healthy and long life without any cardiac problems. Similarly, and this has been well studied, even among people who have a cluster of genetic mutations predisposing them to heart attacks (high polygenic score), following a heart-healthy lifestyle can reduce their risk by 50%. Again, your DNA is not your destiny.
At Wellstar, we also offer a robust 'Know Your Heart' screening program for the general public to schedule an appointment. The advanced version of this includes a CT coronary calcium score. For specialized care, we have a Preventive Cardiology office, where we offer evidence-based, patient and family-centered care with a multidisciplinary team including a cardiologist, dietician, clinical pharmacist and geneticist. Our cardio-genetics program has the highest volume of patients in Georgia.
Mooney: Through programs like Kids Heart Challenge at the American Heart Association, which partners with schools to help prepare children for success by empowering them to embrace a healthy lifestyle—eat well, move more and stay tobacco free. The Kids Heart Challenge prepares elementary students for future success both physically and emotionally. Through cardio-pumping physical activities, kids learn the importance of being heart-healthy. Participating schools and/or teachers receive discounted certificates for PE equipment, direct contributions to their school and new curriculum resources for whole-child centered learning. Healthy students are better learners; teachers and schools have a major influence on students’ health, and the Kids Heart Challenge is designed to support and improve those efforts.
One other AHA program, Target BP (blood pressure), using the M.A.P. (measure accurately; act rapidly; partner with patients, communities) Framework is connecting the community to clinics. This program here at the American Heart Association is designed to work with clinicians with improving how blood pressure is measured, developing treatment algorithms to improve uncontrolled blood pressure. This program’s framework was used to train barbers and stylists in an initiative called “Do You Know Your Numbers?”
We worked in barber shops and salons, faith-based and community-based organizations to install blood-pressure monitors and train them on how to use them. In the barbershop we talk about sports, families, children, so within that conversation it was simple to bring up “do you know your numbers?” And once they asked that question, and their clients are interested in knowing their numbers, they are able to screen those clients for high blood pressure. The people who need medical care are connected with health centers or clinics.
It has worked and it has grown and it's nationwide. We sent this national hypertension project throughout so many different communities, whether rural or urban. We find that bringing in that community component helps get patients to seeing their clinicians.
Rubinger: Education about cardiovascular disease risk factors clearly plays a big part in helping people avoid making bad decisions. What programs or initiatives have had the biggest impact?
Sacks: If there is a group of people that we have significantly impacted, it is women. Mr. Mooney can speak to this too. You know, if you ask a woman what is she most likely to die from, she will probably tell you breast cancer or uterine cancer. But the truth is she is most likely to die from heart disease. The AHA has highlighted this with their Wear Red Day events and other programs. Women have come to understand their cardiac risk, and that their symptoms of heart disease may differ from those of men.
Mooney: I would agree with you on that. The information, as it relates to women dying of heart disease, is really the approach of addressing social determinants of health.
And quality improvements are really about self-management. For example, with the blood pressure project, it is a way of educating the patients, empowering the patients to take control of their blood pressure through what the doctors have shared with them. Talking to and educating these patients, as in the example Dr. Sacks gave in Paulding County, helps them know what are those factors that impact their health, such as healthy eating, access to care, also access to medication.
We're discovering in this hypertension research project that these populations would not have had access to blood pressure monitors outside of the doctor's office to get true blood pressure readings. That's self-measurement. Now these devices, when they check their blood pressure, it automatically links up into their EMR systems. It's all about time: the patient comes from that (screening) to a follow-up appointment. Doctors have a real clear big picture of what the patient’s true blood pressure readings are, and that's where it goes into better treatment plans as it relates to physical activity, diet, and so forth.
Sacks: That recent study involving stationing pharmacists in predominantly African-American owned barber shops demonstrated the power of education. They screened patrons’ blood pressure. A large number of men, with no prior medical history, were found to have significant hypertension (high blood pressure). These individuals were then placed on medication. It was an amazing study because they were able to identify, educate and treat these patients thus reducing their risk of heart attack and stroke.
Rubinger: The key here is my numbers. My primary care physician needs be looking at those numbers closely, even though I am a younger person, because they're the bridge to getting referred to take care of these conditions. Is the primary care system addressing the hard health issues in cardiac care?
Nautiyal: When we started the Preventive Cardiology Program about two years ago, we took a holistic or multi-pronged approach for this very reason. When thinking of cardiovascular risk in the population, you can imagine a pyramid. At the base of the pyramid are people with traditional risk factors like obesity, high blood pressure, high cholesterol. As you move up this pyramid, you will have more serious risk factors—for example, diabetes—and at the tip of the pyramid would be people with familial hypercholesterolemia or family history for premature heart disease, who are fewer in comparison to the base, but have highest personal risk.
We'll make the most impact by focusing on the base, because that's where the most patients are and that can be addressed adequately at the primary care level or through community-led initiatives.
And we at the Wellstar Preventive Cardiology Program are engaging with our primary care colleagues to accomplish this through the initiatives I mentioned earlier, helping them in their own preventive strategies and identifying those at the tip of the pyramid, with higher personal risk who will benefit from specialized preventive cardiology care.
Mooney: That's what the American Heart Association is all about: bringing awareness on heart disease to rural and urban communities and vulnerable populations. We are developing science based tools and resources for clinicians and providers to keep them informed with the current research and what's going on out there, as well as providing educational tools in all languages for their patient population.
We discovered that patients heard the numbers but didn't know what they meant and didn't know how they impacted their bodies. We design educational materials for these patients to really understand the consequences of high blood pressure for any literacy level. For example, in some workshops with patients and the community, we may use infographics of a home water hose connected to a street fire hydrant as an example of blood vessels to the heart and/or a boxer beating the kidney to give a visual of what high blood pressure does to the body organs. Blood pressure has impacts on your entire body. Giving the visual, just keeping it simple and straight to the point.
Rubinger: It's all about trust, right? They have to trust the medical system. There are certain communities that in the past have not trusted the medical establishment.
Mooney: Absolutely. That's why we are such a big proponent of diversity in the workplace and bringing young scholars, HBCU scholars, historical black institutions and biomedical students into this arena, connecting them with cardiologists and scientists throughout their undergrad, up into medical school and up into their careers. That's key. And that's important because getting out there in the community is key to building that trust. People trust people who are very familiar with their environment.
Rubinger: That need to build trust between the medical profession and certain communities leads me to another issue: the disparity in different groups when it comes to obtaining medical care. How can our cardiac experts help close the gap in this area?
Mooney: The AHA has put a lot of money and research and grants focused on science-based solutions to address health inequalities through, for example, our Health Equity Research Network on Prevention of Hypertension.
I'm research-focused on cardio and oncology working in underserved communities and bringing forward awareness of the connection of heart disease and cancer, as well as putting our money back into the community to support community-based organizations that are addressing social determinants of health that could assist with improving overall cardiovascular health as it relates to addressing food insecurity, vaping advocacy work that we do in school systems throughout the country and also where we are invested into people. We're working with our historically black colleges and universities, identifying those underrepresented in the medical field and enlightening them to also become representatives in the medical field to help improve overall health and communities throughout the nation. We've been committed to that, and we're very much committed to that.
As it relates to the training for our providers and clinicians through quality improvement programs such as “Get Down With Your Blood Pressure” and our cholesterol control program as well, we are providing the research and the educational tools for providers and for patients to assist health systems. We'll start on improving blood pressure with other health systems throughout the United States and particularly in the metro Atlanta area.
Sacks: If we needed a reminder about health equity, certainly the pandemic provided us with that experience. The mortality from COVID was much higher in the African-American and Latino communities. There is a saying that a parent is only as happy as their least happy child. Similarly, the medical community should only be satisfied if everyone has access to healthcare.
We must do a lot more than we are doing to ensure a better distribution of our resources. That is our obligation as healthcare providers. We need to deliver healthcare to those who are unable to come to us, but who nonetheless are in need of our services. We need to go to them.
Rubinger: How important is the employer towards helping deliver on some of these messages to their employees?
Sacks: From the business standpoint, employers need to offer more health and wellness opportunities for their employees. And why is that? Because if they do, their workers will spend more time at work and less time at home, sick. They will spend less time in the emergency room because of adopting a healthier lifestyle and medical conditions will be identified sooner. The more businesses can promote these kinds of internal programs, the more an employee realizes 'my employer really cares about me; they really want me to be healthy.' It's a win-win for everyone, so those programs need to be much more widespread and offered to more people.
Mooney: The American Heart Association has workplace programs where we work with employers throughout the nation and throughout Georgia. Also we work with organizations just in in terms of broadening or expanding the pool of applicants, or those in leadership, to be able to be a representation of the community in which they serve.

TomCare
When COVID forced everyone to spend more time at home, Tom Murphy decided he wouldn’t sit around idle. At 62, he upped his regular activity to work out with his son, daughter and daughter’s fiancé—college athletes who kept him in top shape.
Tom’s go-to workout was a long walk in a hilly East Cobb neighborhood. He and the kids also played a lot of pickleball.
About a year in, Tom noticed a physical change.
“I was playing fewer games of pickleball at a time and making it only halfway through my walks,” he said.
Tom turned to his cardiologist, who, with the help of specialized imaging offered at Wellstar Kennestone Regional Medical Center, created a personalized action plan.
Getting answers with the help of HeartFlow
During Tom’s annual appointment with Dr. George Kramer, he shared his concerns about his symptoms.
“I do sports with my kids, and I’m short of breath,” Tom said.
The physician requested a cardiac CT (CCTA), the new standard for detecting heart disease, according to the American Heart Association. It can be more accurate than treadmill stress tests and is less invasive than cardiac catheterization.
“Results of the initial CT showed two blockages,” Dr. Kramer said. “One blockage was 67%, one was 75%, and we decided to follow up with further analysis using the HeartFlow test.”
Because Wellstar was the first HeartFlow Platinum site in Georgia, the cardiology staff were able to create a personalized, 3D model of Tom’s coronary arteries to check on blood flow. HeartFlow is a fractional reserve assessment that looks at how each blockage impacts the heart. Previously, this in-depth view of the heart could only happen with a more invasive procedure.
According to Dr. Kramer, the test itself has been “a godsend” since it makes it possible for patients to avoid invasive tests while still getting important—and potentially lifesaving—information about their hearts.
HeartFlow revealed the blood flow to Tom’s heart was significantly compromised.

Tom and his 91-year-old mother stand together for heart health.

Caring for Wellstar Team Members: Wellness Rooms

2023 Team Member Giving Campaign

2023 Team Member Giving Campaign

2023 Team Member Giving Campaign
Wellstar Health System Expands Partnership with Virtual Reality Company Moth+Flame
This month Wellstar Health System announced it is extending its partnership with Moth+Flame to further utilize its virtual reality (VR) training technology throughout the enterprise.
Moth+Flame is an award-winning VR communication technology developer and premier enterprise-grade immersive learning provider offering innovative and adaptive learning programs for mastering technical and cognitive skills. Their platform includes content focused on emotional intelligence. When learners put on their headsets, they inhabit and interact with immersive simulated environments. They decide in the moment how to respond and see for themselves the impact their words and decisions have on others — and reflect on how to improve. Trainees receive an empathy rating score at the end of their session.
Last May, Catalyst by Wellstar led Wellstar’s first-ever VR-based leadership development training in collaboration with Moth+Flame. This was Moth+Flame’s first healthcare partnership, and the use of this technology continues to expand within Wellstar’s enterprise.
Following the training, 97% of participants recommended the virtual learning experience to others. They also reported that the training reduced their anxiety around difficult conversations by 57%. As a result of the successful pilot, Wellstar decided to offer VR emotional intelligence training regularly.
“We believe strongly that immersive learning is the future of learning and builds more confidence through practice,” said Kevin Cornish, CEO and founder at Moth+Flame. “Using virtual reality puts you inside of a difficult conversation and gives you a chance to learn in a safe simulated environment.”
The VR emotional intelligence training encourages Wellstar’s employees to build composure and gain practical experience in a highly realistic scenario by navigating difficult conversations and testing resiliency in an emotionally charged environment. This experience helps Wellstar’s workforce develop strategies to build situational awareness and prioritize composure, critical thinking and conscious emotional responses when engaging in triggering conversations.
By gaining conversational expertise and knowledge, Wellstar’s team will know how to respond in real scenarios with the confidence to interact appropriately and strategically.
“The realism within Moth+Flame's VR experiences, from using real-life actors, dramatically increases the emotional connection to the content and helps learners retain the information they learn. We are grateful for Moth+Flame's partnership in helping introduce VR to our leaders,” said Steven LeClercq, executive director of learning and onboarding at Wellstar Health System.
This use of innovation keeps Wellstar on the leading edge of training and team development, and the organization will continue to explore use cases for this technology within a clinical setting.

AshleyCare
In March of 2021, Ashley Martin suffered cardiac arrest, which kills about 90% of people when it happens outside of a hospital. Thankfully, she was already at Wellstar Kennestone Regional Medical Center receiving the compassionate care she’d been seeking to address a long list of symptoms.
Everything began at a hectic time in Ashley’s life. She was 30 and had just gotten engaged. Wedding planning had started with the help of her fiancé and their two young boys. The hope had been to have the wedding toward the end of 2021. But the unexpected happened.
“I was always healthy,” she said. “I grew up playing sports. I was a runner. I used to get headaches, but that was the extent of my medical history.”
Symptoms of what would ultimately be diagnosed as Guillain-Barré syndrome began in February of 2021. This rare neurological disorder causes the body’s immune system to attack the nerves.
Ashley started experiencing tingling in the tips of her hands and feet, which moved up her legs and arms as days passed. When intermittent numbness became a symptom, Ashley went to a hospital near her Peachtree City home. A clean CT and MRI meant she went home with plans to see a rheumatologist.
As she waited for her first appointment, she started feeling numbness in her feet.
“At one point, I took a step down the stairs and went tumbling down to the concrete floor,” Ashley said.
On another trip to the hospital near her home, Ashley was diagnosed with Guillain-Barré syndrome, but treatment was unsuccessful. The numbness continued, spreading to her face. She began using a walker and, soon after, a wheelchair.
“The paralysis had moved to my abdomen,” Ashley said. “I went to sleep one night and woke up abruptly gasping for air.”
Later that night, an ambulance brought Ashley to Wellstar Kennestone, where she would finally get the specialized neuro care she desperately needed. She was admitted to the Neurocritical Care unit, staffed by physicians, nurses and a medical team with specialized training in neurological conditions.
Upon arrival, she underwent respiratory failure due to paralysis spreading to her diaphragm. She was stabilized, but shortly after that, she experienced sudden cardiac arrest—the abrupt loss of heart function that stops blood flow to the body.
After a critical care nurse administered CPR, Ashley’s heart started beating again. Life support medications were given to keep her heart pumping.
“The neuro ICU nurses and doctors saved my life,” she said.
Later, her attending neurologist explained that the stress of her nervous system and immune system fighting, paired with respiratory failure, caused such high stress that she had a cardiac arrest.

Wellstar North Fulton Medical Center Receives Comprehensive Stroke Center Certification
Wellstar Health System announced today that The Joint Commission recognized Wellstar North Fulton Medical Center as a Comprehensive Stroke Center, the most demanding stroke certification recognizing hospitals that have specific abilities to receive and treat the most complex stroke cases. With two of the eight Comprehensive Stroke Centers in Georgia, Wellstar Health System now offers stroke patients greater access to the highest level of stroke and aneurysm care. Wellstar Kennestone Regional Medical Center is also Joint Commission certified as a Comprehensive Stroke Center.
“For years, we have provided world-class stroke care for each and every patient when they need it most. This designation represents how hard we have worked to provide the very best quality care for patients in North Fulton County and across Georgia. We’re proud that our work and subsequent positive patient outcomes are being recognized,” said Dr. Michael Mendoza, medical director of the Stroke Program at Wellstar North Fulton.
Wellstar North Fulton’s certification allows more Georgians to have access to the most advance diagnostics and treatments for cerebrovascular disease such as stroke. This is important because Georgia is located in the Stroke Belt, which is comprised of 11 states in the Southeast where the associated mortality rate for stroke patients is 10 percent above the national average.
At Wellstar North Fulton and Wellstar Kennestone, patients have access to advanced diagnostics and therapies to care for even the most complicated strokes faster and more effectively. These include:
“Our team of neurosurgeons, neurocritical care physicians, neuroradiologists, advanced practice practitioners and nurses work together to perform world-class thrombectomies, aneurysm treatments, carotid surgeries and cerebral bypass procedures so that patients can regain their best quality of life. Additionally, our dedicated hybrid neurovascular suite is equipped with innovative bi-plane technology. This allows neurosurgeons to view highly detailed images of brain vessels, so we as a team can customize treatments in real time,” said Dr. Arthur Grigorian, neurosurgeon, Wellstar North Fulton.
“When you have a stroke, every second counts. Getting fast, expert stroke care can mean the difference between life, death, or lasting brain damage. We are proud to receive this prestigious certification at Wellstar North Fulton, informing the surrounding community that they don’t have to go far to receive the best treatment possible. We will continue to work hard to provide an interdisciplinary, innovative, and compassionate approach to safe and quality comprehensive stroke care to all the communities we serve,” said Jon-Paul Croom, president, Wellstar North Fulton and senior vice president, Wellstar Health System.
Wellstar is a leading provider of stroke and aneurysm services in Georgia and performs one of the highest numbers of thrombectomy and aneurysm treatments in the country. The Joint Commission is a United States-based nonprofit organization that accredits more than 22,000 healthcare organizations and programs.

KevinCare
There aren’t many people out there who can say they survived cardiac arrest at 30. Kevin Miskewicz can.
According to the American Heart Association, more than 90% of people who experience an out-of-hospital cardiac arrest die. Those who survive often have permanent neurological disabilities. But Kevin’s story has an incredibly fortunate ending, thanks to the highly coordinated work of his medical experts at Wellstar.
Recovering from cardiac arrest is something Kevin will never forget. It lives forever as a piece of his health history—one that includes a dedicated healthcare team—and his wife, who was the first to save his life.

Kevin woke up on Labor Day 2017 at 5:30 AM to take the dog out. Pausing to adjust the thermostat as he came in, he fell, knocking over a lamp.
He was in cardiac arrest.
With no symptoms and no known pre-existing condition, this was unexpected, but that didn’t stop his wife, Andrea, from jumping into action.
“If it weren’t for me knocking over a lamp when I passed out,” said Kevin, “she would have never woken up and saved my life.”
In addition to calling 911 and unlocking the door for the paramedics, Andrea performed CPR for 10 minutes.
“Kevin’s wife doing good CPR was critical,” said Dr. Arthur Reitman, the interventional cardiologist who was a vital part of Kevin’s treatment team at Wellstar Kennestone Regional Medical Center. “More than five minutes of poor blood flow to the brain can result in permanent irreparable injury from which a patient is unable to recover.”
When paramedics arrived at Kevin’s home, he had no pulse and was not breathing. As the paramedics performed their lifesaving work, he technically died two times.
The ambulance took him to Wellstar North Fulton Medical Center, where he was initially assessed and treated by Dr. David Jacoboff. The interventional cardiologist implanted an intra-aortic balloon pump to stabilize him. Then, he transferred Kevin to Wellstar Kennestone for highly specialized heart care.
When Kevin arrived at Wellstar Kennestone by helicopter, his heart function wasn’t strong enough to support his body. Dr. Reitman and a team of doctors including a cardiologist, a pulmonologist and critical care doctors worked in tandem to put Kevin on an advanced life support system called veno-arterial extracorporeal membrane oxygenation. Better known as VA-ECMO, it took the heart “offline” so it could heal. The technology removed unoxygenated blood from his body, oxygenated it and pumped it back in for the next three days.
“Very few places in the state—only four or five hospitals—have the technology and specialized training to put a patient on ECMO,” Dr. Reitman explained.

Overcome Obesity with the Help of a Primary Care Provider
You’re considered obese when your body mass index (BMI) reaches 30.0 or higher. Sometimes that means you gain 15 pounds, and nobody notices you’ve gotten much bigger. Sometimes it means you have a visible weight problem.
For U.S. adults aged 20 and over, there’s a 41.9% prevalence of obesity according to the Centers for Disease Control and Prevention. That most likely makes it more common than you suspected. And, even if you don’t feel like you’re severely overweight, being obese—according to the numbers—means opening the door to a long list of potential health risks.
So, if you can’t stop gaining weight or simply aren’t seeing the pounds come off no matter what you do, it’s time to consult a primary care doctor or advanced practice professional (APP).
“Physicians previously thought obesity was only due to overeating and less exercise,” said Dr. Alicia Shelly, a Wellstar primary care provider. “The advice was always to move more and eat less, but it never guaranteed they would lose significant weight.”
In recent years, there’s been a shift in understanding weight gain, where it can stem from and how broad the range of categories really is. You can be obese because of:
The factors that impact your weight gain drastically affect your options for treatment and what lifestyle changes you need to make to see a difference.
Even with so many factors potentially causing obesity, the one constant is its negative impact on your health.
“There are more than 200 complications that accompany obesity,” Dr. Shelly said.
These include more serious issues like heart disease, liver disease, hypertension and diabetes, but also other risks like reproductive disorders, sleep apnea, joint pain and mood disorders.
“Losing only 5-10% of your current weight can prove beneficial at reducing the risk of many of these obesity-related complications,” Dr. Shelly shared.
Reducing your weight by just 2.5% percent can help lower your risk of diabetes, and losing just 5% percent of your weight can improve your overall quality of life.
Being overweight—and talking about it—can sometimes be difficult. You may feel embarrassed or that your weight gain reflects poorly on you. However, seeing that so many factors can cause weight gain that may be out of your control, there’s no reason to fear this type of conversation. What’s important though, is having a doctor or APP you trust and who supports you.
Tips for discussing weight with your doctor
Your expectations for what weight loss should look like may be different than your health provider. However, it’s sometimes necessary to put your assumptions about weight loss aside. Use the information your doctor gives you to make an educated choice as to what’s best for your overall health.
There’s no rush to lose weight. What’s important is making positive changes that you can commit to indefinitely that will take weight off and allow you to keep it off.
Many weight loss plans begin with lifestyle changes. These can include changing how you handle stress, keeping a food journal or focusing on portion control. You may even have to add or remove certain foods or beverages from your diet.
With these changes should also come a plan for staying vigilant even when life throws a curveball to your routine.
“It is common for people to get overwhelmed with the challenges during their weight loss journey and quit,” Dr. Shelly said. “This is why a piece of your weight loss plan will include addressing potential challenges and mapping out ways to overcome them.”
Appetite suppressants may also assist with an effective weight loss plan. New weight management options have come on the market in recent years. Your doctor may prescribe an FDA-approved medication, but it’s good to know that most offer an average weight loss of anywhere between 6-15%, and all carry the possibility of side effects that range from insomnia to nausea to constipation.
Work closely with your doctor before taking any medication, and only use what they prescribe.
Once you’re motivated to start losing weight, the first step on your journey is to create a road map with a qualified medical professional as your guide. Schedule an appointment with your primary care physician or search for a primary care provider near you.
Wellstar Honors the Life and Legacy of Dr. Martin Luther King Jr.
On January 12, Wellstar honored the life, legacy and many contributions of Dr. Martin Luther King Jr. with a live-streamed tribute. The program included performances from The Wellstar Singers, interfaith prayers and a keynote address featuring a conversation between Dr. Bernice A. King, youngest daughter of Martin and Coretta Scott King, and Monica Kaufman Pearson, beloved former Atlanta news anchor.
The program was themed around a 1957 quote from Dr. Martin Luther King Jr., “Life's most persistent and urgent question is, ‘What are you doing for others?’"
Throughout the program, Dr. Bernice A. King shared important life lessons instilled in her as a child, including the value of forgiveness and nonviolence. Dr. King provided insight about the state of the world, growing polarization and the need to take time to listen to those who we perceive as our enemies.
As CEO of The King Center, Dr. Bernice A. King’s mission is to spread her father’s philosophy and methodology of nonviolence. Through programs like Nonviolence365®, Beloved Community Leadership Academy and Students with the King, she is working to make perspective-altering resources available to people of all ages.
This program was pre-recorded in November at the National Center for Civil and Human Rights. The conversation was held in front of a live audience including Wellstar leaders, members of the Minority Physician Business Resource Group and our Diversity, Equity and Inclusion team.
Wellstar is honored to celebrate the life and legacy of American Civil Rights Movement leader and activist Dr. Martin Luther King Jr. and recognizes Martin Luther King Jr. Day as a paid holiday. Team members are encouraged to take the day “on” by volunteering in the community.
Wellstar is proud to be a corporate sponsor partnering with The King Center on a variety of events leading up to the holiday on Jan. 16.

Wellstar Paulding Medical Center Launches Spine Surgery Services
Wellstar Paulding Medical Center now offers spine surgery, giving patients in Paulding County and surrounding areas access to expert care for spinal conditions.
Spine surgery can help people like patient Ulysses Price find relief from chronic pain and get back to the activities they enjoy.
“Low back pain is such a common complaint among patients, and there are a limited number of specialists who are able to address these concerns,” said Wellstar Neurosurgeon Dr. Phillip Parry.
If you are experiencing neck or back pain or managing a spinal condition, Wellstar’s Neuro Care team will work with you to create a personalized care plan and decide if surgery is the most effective treatment option. Wellstar’s spine surgeons help patients with a variety of spinal conditions, including scoliosis, sciatica, arthritis, herniated disks and spinal deformities. Our spine surgeons perform cervical disk replacements and cervical fusions for cervical neck pain syndromes and offer both simple and complex spine surgical options for patients with low back pain syndromes.
Surgeons at Wellstar Paulding Medical Center also perform peripheral nerve decompression surgery for patients with carpal tunnel syndrome and other compression neuropathies.
“Wellstar offers a unique opportunity for patients to receive comprehensive, compassionate and close-to-home care for whatever disease process they may have,” Dr. Parry said. “The spine care provided here at Wellstar is world-class.”
Schedule an appointment with a neurosurgeon in Hiram by calling (770) 422-2326.

Leadership for Intense Times
Healthcare professionals are trained to work with science, data and facts. But when the pandemic hit, leaders had to grapple with working through the unknown. According to Jill Case-Wirth, senior vice president and chief nurse executive of Wellstar Health System, core tenets of leadership, such as communication, courage, and the ability to establish trust, remained constant, while other characteristics moved more clearly into focus in 2020.
“Humility rose to the forefront,” Case-Wirth said. “You had to be comfortable being able to say, ‘I don’t know, but together we’re going to figure this out … and we’re going to do the best that we can with the information we have available.’”
“We learned a lot of things during COVID about leading differently that we shouldn’t let go of now,” she said.
Case-Wirth shared that data analytics is one of those growth areas for today’s healthcare leaders. Having the ability to review data, gain consensus on the insights, and then quickly develop a plan for an actionable change management strategy is essential for future successful leaders. As a registered nurse, Case-Wirth also places an imperative on planning for the future of nursing, pioneering a career pathway program that starts as young as middle school. In addition to partnering with local universities and technical colleges, she emphasized the importance of being “thoughtful that we have these programs in diverse communities” to reach a wide student population and grow a diverse workforce for the future.
Listen to more insights on Healthcare Executive Podcast.
Case-Wirth was also featured among other healthcare leaders in the article “Leadership for Intense Times” in the November/December issue of Healthcare Executive Magazine.

Augusta University Health System, Wellstar Health System announce letter of intent for statewide health care partnership
Augusta University Health System (AUHS) has signed a letter of intent with Wellstar Health System to form an innovative new partnership that would expand Augusta University’s educational and research missions and allow Wellstar Health System to create a broader affiliation with the university’s Medical College of Georgia (MCG) as AUHS joins the Wellstar Health System.
The potential partnership is the culmination of a thoughtful and deliberate process begun in 2019 by AUHS, its governing board and Augusta University to strategically grow MCG while expanding and improving both patient care and Georgians’ access to health care services across the state.
The proposed partnership would innovate clinical care, training and research while adopting a successful model of bringing together community-based health systems and academic medical centers such as MCG and its teaching hospitals. MCG and Augusta University are part of the University System of Georgia (USG), and MCG serves as the only public medical school in the state.
“AUHS, Augusta University and the Wellstar Health System have a shared mission to solve Georgia’s health care challenges,” USG Chancellor Sonny Perdue said. “By joining forces and working together, we can leverage Wellstar’s clinical platform and leading-edge systems to support patients while providing more opportunities for students to learn, train and care for residents in local communities across Georgia.”
Pending a definitive agreement and regulatory approval, the partnership would focus on three strategic initiatives:
“By bringing Augusta University Health System together with Wellstar Health System and leveraging our respective strengths, we would improve the health of the community, address social determinants of health and expand access to quality care for all Georgians,” said Candice L. Saunders, FACHE, president and chief executive officer of Wellstar Health System.
While there are aspects of the proposed partnership yet to be determined, the partnership would likely result in significant investments to improve existing healthcare facilities and to expand access to care across the state, including a new hospital and medical office buildings in Columbia County.
“Providing health care has never been as dynamic and complex as it is today, and this partnership with the Georgia-based, not-for-profit Wellstar Health System would enable us to extend our mission of improving health through excellence in patient care, education and research for the benefit of Georgians,” said Brooks A. Keel, PhD, acting chief executive officer of Augusta University Health System and president of Augusta University.
Through an expanded affiliation with the university’s Medical College of Georgia, the partnership would address the need to train more physicians and address a growing statewide shortage. With 60 percent of MCG graduates entering a primary care residency, training more physicians in these disciplines would support increased access to frontline care provided by specialists such as family medicine physicians and general pediatricians, especially in underserved areas of the state.
A new teaching campus in Atlanta at Wellstar Kennestone Hospital could also be established under the proposed partnership. As a result, MCG, which already has the ninth-largest freshman medical school class in the nation, would grow to become one of the largest public medical schools in the country.
“With our entire nation facing a physician shortage and our state typically ranking about 40th in the number of physicians per capita, educating the next generation of physicians is more critical than ever,” said David Hess, MD, dean of the Medical College of Georgia and executive vice president of medical affairs and integration at Augusta University. “I’m excited about the partnership with Wellstar, since it will enable our students and residents to continue to learn from some of the most highly qualified physicians and other health care professionals in the state while allowing MCG to expand its contributions to improving public health in Georgia especially in more rural regions.”

A1 Test
Augusta University Health System (AUHS) has signed a letter of intent with Wellstar Health System to form an innovative new partnership that would expand Augusta University’s educational and research missions and allow Wellstar Health System to create a broader affiliation with the university’s Medical College of Georgia (MCG) as AUHS joins the Wellstar Health System.
The potential partnership is the culmination of a thoughtful and deliberate process begun in 2019 by AUHS, its governing board and Augusta University to strategically grow MCG while expanding and improving both patient care and Georgians’ access to health care services across the state.
The proposed partnership would innovate clinical care, training and research while adopting a successful model of bringing together community-based health systems and academic medical centers such as MCG and its teaching hospitals. MCG and Augusta University are part of the University System of Georgia (USG), and MCG serves as the only public medical school in the state.
“AUHS, Augusta University and the Wellstar Health System have a shared mission to solve Georgia’s health care challenges,” USG Chancellor Sonny Perdue said. “By joining forces and working together, we can leverage Wellstar’s clinical platform and leading-edge systems to support patients while providing more opportunities for students to learn, train and care for residents in local communities across Georgia.”
Pending a definitive agreement and regulatory approval, the partnership would focus on three strategic initiatives:
“By bringing Augusta University Health System together with Wellstar Health System and leveraging our respective strengths, we would improve the health of the community, address social determinants of health and expand access to quality care for all Georgians,” said Candice L. Saunders, FACHE, president and chief executive officer of Wellstar Health System.
While there are aspects of the proposed partnership yet to be determined, the partnership would likely result in significant investments to improve existing healthcare facilities and to expand access to care across the state, including a new hospital and medical office buildings in Columbia County.
“Providing health care has never been as dynamic and complex as it is today, and this partnership with the Georgia-based, not-for-profit Wellstar Health System would enable us to extend our mission of improving health through excellence in patient care, education and research for the benefit of Georgians,” said Brooks A. Keel, PhD, acting chief executive officer of Augusta University Health System and president of Augusta University.
Through an expanded affiliation with the university’s Medical College of Georgia, the partnership would address the need to train more physicians and address a growing statewide shortage. With 60 percent of MCG graduates entering a primary care residency, training more physicians in these disciplines would support increased access to frontline care provided by specialists such as family medicine physicians and general pediatricians, especially in underserved areas of the state.
A new teaching campus in Atlanta at Wellstar Kennestone Hospital could also be established under the proposed partnership. As a result, MCG, which already has the ninth-largest freshman medical school class in the nation, would grow to become one of the largest public medical schools in the country.
“With our entire nation facing a physician shortage and our state typically ranking about 40th in the number of physicians per capita, educating the next generation of physicians is more critical than ever,” said David Hess, MD, dean of the Medical College of Georgia and executive vice president of medical affairs and integration at Augusta University. “I’m excited about the partnership with Wellstar, since it will enable our students and residents to continue to learn from some of the most highly qualified physicians and other health care professionals in the state while allowing MCG to expand its contributions to improving public health in Georgia especially in more rural regions.”

Wellstar North Fulton Medical Center Reverified a Level II Trauma Center
Wellstar Health System, which has one of the largest trauma networks in the state, is proud to announce that Wellstar North Fulton Medical Center was again verified as a Level II Trauma Center by the Georgia Department of Public Health (DPH) and American College of Surgeons (ACS). Wellstar North Fulton has been a Level II Trauma Center since 1987 and was the first in Georgia to be verified by the American College of Surgeons in 2015. This marks the third time the hospital has been designated a Level II Trauma Center, demonstrating its commitment to patients in their time of need.
The option to be verified by the ACS is voluntary and is in addition to the State of Georgia designations. Only a handful of trauma centers are verified by the ACS in Georgia, even though they have state designations.
“This designation represents a unique distinction for a community hospital because it demonstrates we are managing trauma cases according to the highest national standards,” said Mark Gravlee, MD, trauma medical director, Wellstar North Fulton Medical Center. “We are reevaluated by the ACS every three years and continue to meet their rigorous standards, so patients in North Fulton and surrounding communities can rest assured they’ll be cared for expertly and with excellence now and well into the future.”
Wellstar North Fulton’s highly skilled trauma team is ready 24/7 to save lives. Level II Trauma Centers provide 24-hour immediate coverage by general surgeons, as well as coverage by the specialties of orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology and critical care. They also offer trauma prevention and continuing education programs for staff, and a comprehensive quality assessment program. Wellstar North Fulton has board-certified trauma surgeons standing by to offer a heightened level of care.
“We are proud to receive this designation again, and more importantly, to be able to offer the advanced care our patients in Northeast Atlanta suffering from accidents, incidents and injuries need,” said Jon-Paul Croom, president, Wellstar North Fulton Medical Center and senior vice president, Wellstar Health System. “This designation is a shining example of our commitment to deliver world-class care to every patient, every time.”
Other trauma centers across the System include Wellstar Kennestone Regional Medical Center (Level II), Wellstar Cobb Medical Center (Level III), Wellstar West Georgia Medical Center (Level IV), and Wellstar Paulding Medical Center (Level IV). Wellstar’s Trauma Network serves patients across the state of Georgia, and the health system is proud to play a critical role in Georgia’s trauma network, collaborating with peers across the state to ensure patients receive the care they need.

Mary Chatman, Executive Vice President of Wellstar Health System and President of Wellstar Kennestone Regional Medical Center and Wellstar Windy Hill Hospital, Named Chair-Elect of the Georgia Hospital Association Board of Trustees
Mary Chatman, PhD, RN, executive vice president (EVP) of Wellstar Health System and president of Wellstar Kennestone Regional Medical Center and Wellstar Windy Hill Hospital, was named chair-elect of the Board of Trustees of the Georgia Hospital Association (GHA) on Nov. 10. Chatman, who has served on the GHA Board since February 2020, will lead the Board in developing strategies for GHA hospital members, advocating for the highest quality care for patients and supporting adequate reimbursement for hospitals.
“Mary Chatman is a visionary leader whose vast leadership skills have benefited Wellstar hospitals and the communities they serve,” said GHA President and CEO Earl Rogers. “She is a strong patient advocate and we look forward to her expertise and leadership of our Board.”
In addition to serving as a Wellstar EVP and president of two of the system’s hospitals, Chatman oversees the operations of the seven other Wellstar hospitals. In 2020, she led the opening of Wellstar Kennestone’s new emergency department, the largest in the Southeast.
Prior to serving in her current role, Chatman was the chief operating officer and chief nursing officer at Memorial Health University Medical Center in Savannah, where she was responsible for managing the 654-bed hospital and its nursing operations. She also served as interim chief information officer for Memorial and completed the electronic health record conversion to EPIC.
This year, Gov. Brian Kemp appointed Chatman to the state’s Healthcare Workforce Commission, where she has helped address challenges in the hiring and retention of healthcare workers.
Chatman has been recognized locally and nationally as a prominent leader and strong patient advocate in health care. Atlanta Daily World recognized her among the 2018 Women of Excellence. Diversity MBA Magazine named her among the 2018 Top 100 Under 50 Executive & Emerging Leaders and 2020 Top 100 Women of Influence. Profiles in Diversity Journal named her a 2020 Women Worth Watching® in STEM award winner. Chatman was recognized by Atlanta Magazine among the 2021 Women Making A Mark honorees and by Becker’s as one of the 75 Black Healthcare Leaders to Know 2022. She was also named the 2020 West Cobb Citizen of the Year for serving on the frontlines for Cobb County, fighting COVID-19 and collaborating with local leaders.
Chatman is deeply involved in the community, serving as board member for United Community Bank and active in the fight to find a cure for type 1 diabetes. She is a member of the American Nurses Association and the American College of Healthcare Executives. She earned her Bachelor of Science, Master of Science and Doctor of Philosophy degrees from East Carolina University in Greenville, North Carolina.

Wellstar Midwives Support Women's Best Health
From welcoming a child to well woman’s exams and health education, women have a partner and advocate in Wellstar’s certified nurse midwives.
Midwives are registered nurses who have received additional education and training in comprehensive care for women. While they may be associated with childbirth — and do support patients through every aspect of labor and delivery — they also offer personalized care for women through every phase of life.
“Midwives do everything spanning from well women’s health, like annual exams, birth control, IUDs and Nexplanon insertions, to all of the prenatal care, so taking care of women from the time of conception throughout delivery and postpartum,” said Emily Goolsby, a certified nurse midwife at Wellstar.
Midwives collaborate with other members of a patient’s care team, including nurses and OB/GYNs, to provide comprehensive care during birth. Whether the patient has a natural childbirth or a medically-assisted birth, midwives provide personalized, expert care and advocate for the patient.
“We support all aspects of birth. We are there for the patients who are laboring naturally and want to be on the birthing ball or moving around, but sometimes the patient says their goal is to feel as little pain as possible,” Goolsby said. “Then, my goal is to advocate for those interventions as soon as possible. It’s all about making the birth experience what our patients want and supporting our patients in that environment.”
Numerous studies have shown the highest quality comprehensive birth experiences come from a multidisciplinary treatment team of midwives and OB/GYNs supporting and caring for a mom together.
“We’re championing for patients’ best outcomes and their babies, and it tends to decrease interventions overall that are unnecessary,” Goolsby said.
After the patient gives birth, midwives support patients through education on parenting topics such as breastfeeding and newborn care.
Midwives care for patients at these Wellstar locations — Wellstar Cobb, Douglas, Kennestone, North Fulton, West Georgia and Spalding medical centers. If you already have a Wellstar OB/GYN, ask your provider about working with a midwife. If you need a new provider, find a Wellstar OB/GYN location near you.

Dr. Hank Capps Awarded 2022 Georgia CIO of the Year® ORBIE® Award in Healthcare
This month Dr. Hank Capps, Wellstar Health System’s executive vice president, chief information and digital officer, and founder and president of Catalyst by Wellstar, was honored by GeorgiaCIO with the 2022 CIO of the Year® ORBIE® Award in the healthcare category.
The CIO ORBIE Awards is the premier technology executive recognition program of its kind that recognizes CIOs in Georgia who have shown excellence in technology leadership. Since its inception in 1998, over 500 CIO winners have received the prestigious ORBIE Award. The ORBIE signifies exceptional leadership, innovation, and vision, representing the characteristics and qualities that inspire others to achieve their potential. GeorgiaCIO is led by an advisory board of CIOs from prominent organizations in Georgia who set the direction for events, membership, and annual Awards program.
“Every organization is technology-dependent, but strong leadership is the X-factor that can turn mundane IT into a remarkable strategic differentiator,” said Brandon Van Orden, GeorgiaCIO Chair. “The ORBIE Awards are meaningful because they are judged by peers – CIOs who understand the challenges of technology leadership.”
Within one year of joining Wellstar, Dr. Capps led the creation and launch of Catalyst by Wellstar, a first-of-its-kind global digital health and innovation center designed to disrupt the future of healthcare. Dr. Capps has also led the transformation of the core technology functions of the organization, including reorganizing around customer needs, launching the Wellstar Data and Insights Institute, and accelerating implementations of ERP, Device Integration, core infrastructure modernization, and data governance initiatives with the main goal to make work easier for clinicians and team members.
“PeopleCare is at the forefront of every project let by the Wellstar team. For myself and the dedicated team at Wellstar, the greatest reward is caring for patients each day,” said Dr. Hank Capps.
Dr. Capps and his team of experts are committed to changing the model from sick care to PeopleCare, by harnessing new technologies and always-connected networks to make care more personalized and focused on well-being through prevention. Some specifics include:
This recognition is a testament to the nearly 1,000 digital, technology, data, and innovation team members who help deliver on Wellstar’s mission of improving the health and well-being of every person served.
Wellstar Paulding Medical Center Breaks Ground on New Radiation Technology
Wellstar Health System announced a multimillion-dollar investment to bring cutting-edge radiation therapy to Wellstar Paulding Medical Center in Hiram, Georgia on November 2, 2022.
“Our motto is ‘Neighbors Caring for Neighbors’ and these new technologies will enhance access to medical care for every neighbor in Paulding County,” said Ralph Turner, Wellstar senior vice president and president of Wellstar Paulding Medical Center. “Our team is focused on providing a patient-centric experience. Having a short drive and the comforts of home and family nearby helps the healing process.”
The expansion will enhance the patient experience by adding a new radiation vault to house a second linear accelerator — the technology that delivers radiation therapy — and is slated for completion in early 2023.
In the last year, patients received nearly 8,000 radiation treatments. The radiation oncology team often extended hours from 7 a.m. until 7 or 8 p.m. to accommodate patients.
During a recent press conference, a group of patients, physicians, healthcare leaders, team members, government leaders and community partners ceremonially broke ground on the major expansion of Wellstar Radiation Oncology. The facility is located on the ground floor of Wellstar Paulding Medical Center’s Outpatient Pavilion at 148 Bill Carruth Parkway in Hiram, Georgia.
The new machine will also bring a leading-edge cancer treatment called stereotactic body radiation therapy (SBRT) to Paulding County for the first time. This radiation technology uses multiple X-ray beams to treat tumors with highly precise, high-dose radiation to any location in the body, preserving surrounding tissue, organs and nerves. The technology allows patients to have significantly fewer treatment sessions.
“This is a huge step forward for cancer care for the people of Paulding County,” said Dr. William Thoms, who has served as the radiation oncology medical director for Wellstar Paulding Medical Center since 2017. “This expansion will allow people to stay in our community for more advanced treatments with shorter wait times.”
The renovation will also modernize the dressing rooms and add more space to increase patient comfort.




CEO Statement About AMC Closure
Candice L. Saunders, FACHE and O. Scott Swayze, MD
Atlanta Medical Center (AMC) has proudly served the community with compassionate healthcare for more than 100 years. It’s a legacy of service and success spanning its years as Tabernacle Baptist Infirmary, Georgia Baptist Hospital and AMC, and at Wellstar, we are honored to have been part of this story.
We understand and share the community’s disappointment that the hospital has closed as of November 1. While the decision may have felt abrupt, it came after an exhaustive search where a national consulting firm identified a number of potential partners. However, after learning more about AMC’s infrastructure and finances, none were willing to move forward. Discussions with state, local and community officials also offered no alternate paths forward.
Throughout the transition, we have remained focused on supporting our AMC patients and team members. Because our top priority is ensuring patient safety, we worked to thoughtfully wind down services in advance of the closure, including safely transferring the few remaining patients to other appropriate Wellstar hospitals and connecting with partners to ensure people receive the care they need.
We are deeply grateful to the hundreds of AMC team members and clinicians who have worked hard to ensure a successful transition and for their many years of service at AMC. We are honored that nearly 75% of our more than 1,780 offers to AMC team members for new positions have been accepted, and we are grateful they will continue in their shared pursuit of Wellstar’s mission and vision. Now that the hospital has been safely closed, Wellstar will continue to secure and maintain the facility and begin a thoughtful process to determine what is next for the site.
The challenges we faced at AMC were multi-faceted and included the age of AMC’s buildings, patients using less than half of the bed capacity, lack of public support while caring for communities most in need of whole-person wellness offerings such as primary and preventive care. Compounding these issues were the intense financial pressures facing hospital systems across the country. Like many of our peers, we felt the pain of the end of government pandemic aid and the skyrocketing costs of supplies and labor. The needed investment to address these challenges was simply too great for Wellstar alone.
As we look ahead, Wellstar will continue to build lasting partnerships that will provide people with increased access to the care they need. As the largest provider of uncompensated care in Georgia, we are proud to serve 1 in 6 Georgians in diverse communities across the region. We will continue to be there for those who need us for primary and specialized care and through our critical role in the statewide collaborative trauma network.
Through our recently announced partnership with Southside Medical Center, Wellstar will invest $5 million in Southside’s East Point clinic to expand their size and capacity and provide greater access to much-needed primary and preventive care, among other services. This is the latest example of our long-standing commitment to partner with others to provide ongoing care to the AMC community.
Our vision for the future requires collaboration with mission-aligned partners and with our friends and neighbors in our communities. That includes partners within and beyond the healthcare industry who can bring unique ideas and perspectives to support the health of the whole person, address the social determinants of health and expand access to world-class care when, where and how people need it. Together, we can transform healthcare to support the people we serve throughout their health and wellness journeys — not just when they are sick or injured. We can build the bold future of care Georgians need and deserve.
Candice L. Saunders, FACHE, is the president and CEO of Wellstar Health System, one of the largest and most integrated health systems in Georgia. A former critical care nurse, she leads nearly 25,000 team members and physicians overseeing the health and well-being of communities throughout the state.

O. Scott Swayze, MD, is the chair of the Board of Trustees for Wellstar Health System. He is an accomplished orthopaedic surgeon, practicing at Pinnacle Orthopaedics and belonging to local, state and national orthopaedic associations.


Wellstar Health System Earns Level 9 Ranking for Digital Health Most Wired Recognition
College of Healthcare Information Management Executives (CHIME), has released their coveted Digital Health Most Wired Survey results for the 2022 data collection period. Wellstar Health System is proud to announce our Level 9 recognition in both acute and ambulatory categories survey selection. This is the eighth time Wellstar has been recognized with this award. Wellstar is one of only two organizations in Georgia to receive the Level 9 rating.
The annual survey is designed to recognize healthcare organizations that exemplify best practices through their adoption, implementation and use of information technology.
Among the more than 38,000 organizations surveyed by CHIME, Wellstar Health System ranked above peers in categories like analytics and data management, population health, infrastructure and patient engagement. The survey assessed the impact of technologies in healthcare organizations at all stages of development, from early development to industry leading.
“We are proud to honor your team’s exceptional dedication to excellence in digital health,” said CHIME President and CEO Russell P. Branzell. “Your pioneering performance in the industry inspires other organizations by example. Patients in communities around the world receive better care when you drive change through digital transformation, as you have proven through your success in this rigorous program.”
The Digital Health Most Wired survey and recognition program serves as a comprehensive “Digital Health Check-up” for healthcare organizations across the world. As success in digital health increasingly determines the quality of patient care, the scope of the CHIME Digital Health Most Wired survey reflects the progress of leading healthcare providers as they reinvent healthcare for a new century.
“Patients in our communities can receive better care when we drive change through digital transformation, as we have proven through our success in this rigorous program,” said Dr. Pranav Jain, VP and chief medical information, Wellstar Health System. “These recognitions help Wellstar’s patients understand the high level of care they can receive, and that we strive to better the lives of every patient we serve.”

Southside Medical Center and Wellstar Partner to Enhance the Health of Atlanta Communities
Wellstar Health System and Southside Medical Center are announcing a new partnership to improve primary and preventive care throughout Atlanta communities. Together, the organizations will focus on expanding access to preventive, whole-person care and chronic disease support, rather than treating patients episodically when they are acutely sick or injured without guaranteed follow up.
As the first step in this collaboration, Wellstar will invest nearly $5 million toward expanding primary care services for thousands of East Point residents at Southside Medical Center’s East Point clinic located at 1100 Cleveland Ave. Through Wellstar’s investment, the Southside Medical Center clinic in East Point will expand its size, capacity and hours.
“This important partnership will create a much-needed medical home that will meet the primary and preventive care needs of the South Fulton County community,” said David M. Williams, MD, President and CEO of Southside Medical Center. “Wellstar and Southside share a vision to promote a culture of health and well-being. Building upon the initial expansion in East Point, our plan is to promote change in health status, lifestyles and health outcomes in the patients we serve through a new model of care throughout Metro Atlanta.”
The Southside Medical Center clinic is adjacent to Wellstar’s East Point Health Center (EPHC), which offers urgent care, care coordination and behavioral health services. Through this partnership, care coordinators at EPHC will support urgent care patients in developing a relationship with primary care clinicians at Southside Medical Center to support their long-term health and well-being.
“At Wellstar, we know from our experience, and we have heard from our patients and consumers that our communities have a critical need for preventive primary care health services, especially those focused on chronic illnesses,” said Candice L. Saunders, President and CEO of Wellstar Health System. “We are proud to partner with Southside Medical Center to grow access to the kind of care that matches the needs of the community and promotes the long-term health and well-being of the people we serve. This partnership represents Wellstar’s broader vision for the future of healthcare, which is focused on transformative care models that support overall community health and wellness through personalized preventive care.”
In April 2022, Wellstar transitioned the Atlanta Medical Center South hospital campus to an urgent care clinic to better match the care needs of the community. The partnership with Southside Medical Center represents the next step on this journey to create a sustainable care solution that will best serve the South Fulton County community long-term.
By expanding and enhancing the care offered through Southside Medical Center, patients will have access to family medicine, general dentistry, behavioral health services and substance abuse disorders management. Patients will also have access to Southside’s Behavioral Lifestyle Enrichment Center, which provides mental health and addiction treatment through their comprehensive Lifestyle Enrichment Treatment program to address addiction, depression, anxiety and other disorders.
Southside Medical Center is a Federally Qualified Health Center (FQHC) that has provided care to East Point and Atlanta communities for over 55 years. As an FQHC, Southside Medical Center provides primary care access to all patients of the communities it serves, especially
underserved communities. Southside Medical Center has strong ties to the community, and expanding their clinic is the right next step toward a sustainable care solution for a population that needs access to primary care, preventive and mental health services. As an FQHC, Southside Medical Center intends to provide greater access to primary and preventive health care services in addition to addressing the chronic care needs of the community through the patient-centered medical home model, which is designed to address both the clinical and social determinants of health issues which impact the healthcare and well-being of our community.
An important member of the East Point and Atlanta communities, Southside Medical Center has been nationally recognized by the National Association of Community Health Centers for having one of the best primary care delivery systems for the medically underserved.
“I look forward to the incredible impact this clinic will have on the lives of the patients and families we serve,” Dr. Williams said. “The expansion in East Point is just the beginning of an impactful partnership with Wellstar that I’m confident will meaningfully improve the health of our friends and neighbors throughout our region.”
As these groups move forward with this exciting partnership, Wellstar and Southside Medical Center will continue to work in collaboration with East Point Mayor Deana Ingraham, and we look forward to sharing more about this exciting next step.
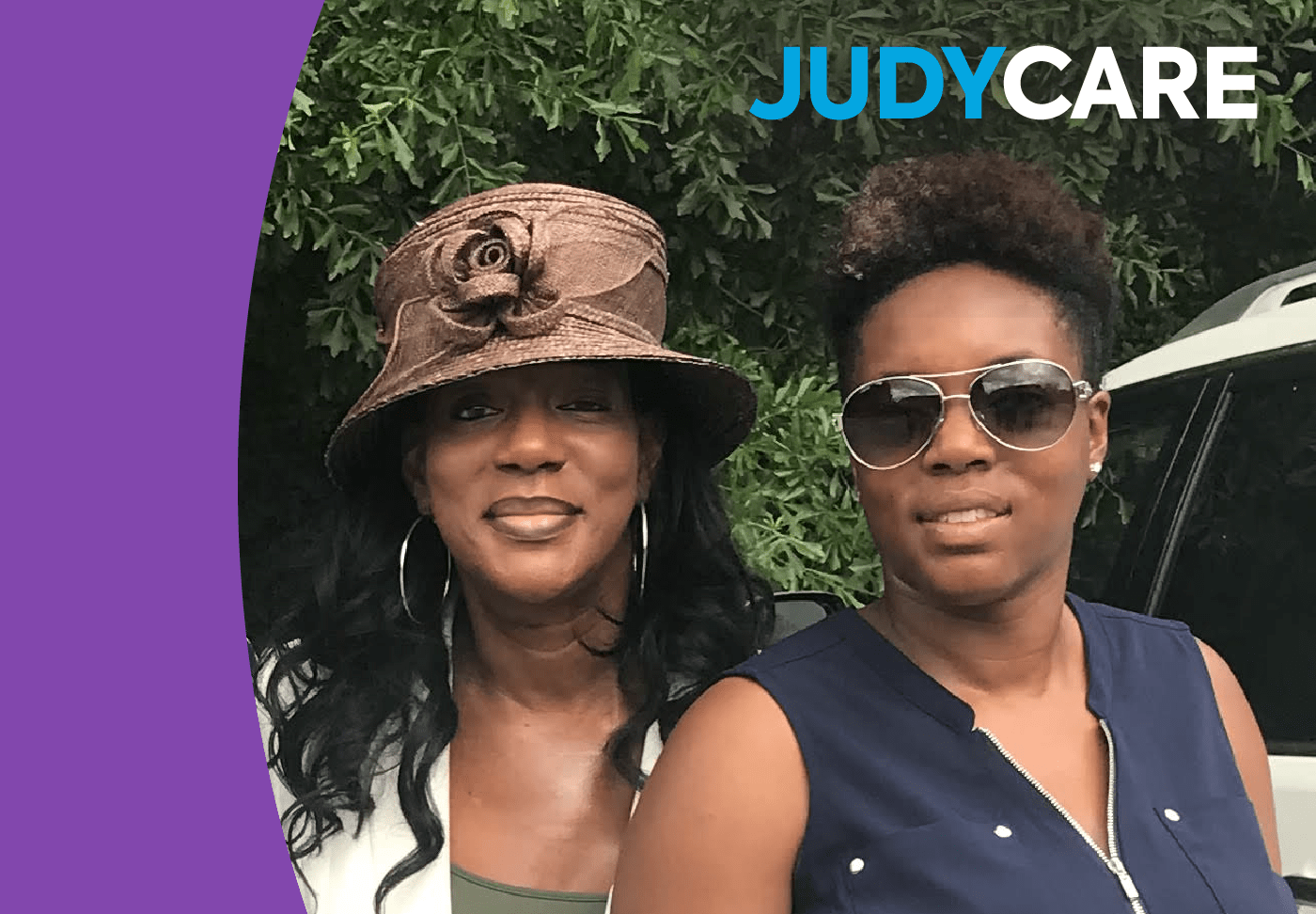
JudyCare
Judy Robinson finished her fifth tour as a civilian assisting the military in January of 2018. She prioritized visiting her mother, her three adult daughters and five grandchildren when she returned to Douglasville. Second on the list was scheduling her routine health checks, as required every year by the military, including having a mammogram.
A mammogram is a routine X-ray that takes a picture of the breast to identify early signs of breast cancer. Mammograms can catch cancer before it can be felt, sometimes up to three years earlier. When breast cancer is detected earlier, the outcomes can be better for patients.
At Wellstar Douglas Medical Center, Judy’s mammogram identified a lump in the breast. A biopsy confirmed it was cancer. This was the third time Robinson was diagnosed with breast cancer in 20 years.
“The most aggressive breast cancer I had was the very first time,” she said, explaining that when her breast cancer was treated in 1998, she had a lumpectomy (a breast-preserving procedure that only removes the abnormal tissue from the breast), radiation and chemotherapy.
Her daughters were school-aged children at the time, and Robinson’s mother helped with their care as Robinson underwent aggressive treatment.
“I went to work one day, and I thought to myself, ‘I can’t do this. This is too much,’” she remembered. “I saw their picture on my desk, and I thought, ‘You know what, Lord, I’ve got to hang in here for them.’ My whole attitude changed. It wasn’t about me or how I was feeling. It was about providing for them.”
She fought breast cancer and won, eating healthily, exercising and loving her family for nearly 10 years before it returned.
“I was on Tamoxifen (a hormonal therapy used to treat hormone-receptor-positive breast cancer), and it was so strong it threw me into menopause,” she said. “I was having hot flashes so bad, so I stopped taking it. If I would have stayed on it, it may not have come back.”
When cancer returned to her left breast, Robinson chose to have a mastectomy — complete breast removal and reconstructive surgery.
“My attitude for treatment was better the second time,” she said, smiling. “I would skip in there and bring that positive sunshine personality to rub off on everybody else!”
In 2018, she was diagnosed for the third time — this time, the breast cancer was in her right breast. She had a mastectomy at Wellstar Cobb Medical Center and breast reconstruction surgery in September 2020.
“Breasts don’t make or break us,” Judy said. “We are who we are as humans. It’s all about what’s in the heart. I’ve learned that. And, reconstructive surgery has its perks!”
Her oncologist recommended a long-term oral medication to help decrease the chance of the cancer returning. Throughout her treatment, Robinson found comfort by participating in a breast cancer support group at Wellstar Douglas Medical Center.
“I didn’t have any hair — I was wearing a wig,” she remembered. “I met a lady who had ovarian cancer, and it was amazing. I always find comfort in talking to others there.”
Robinson has had her share of health challenges, including living with multiple sclerosis, diagnosed around the same time as her third breast cancer diagnosis. But she has an incredibly positive outlook.
Robinson owns two service-oriented businesses and runs them with her sister and two of her daughters.
Nell's Place is a transitional home serving civilians and veterans with disabilities such as bipolar disorder and schizophrenia. Robinson goes above and beyond the call of duty, often playing the role of a family member in addition to that of a daily caregiver. She often takes groups of residents out to dinner to celebrate a resident’s birthday when their family is not involved.
Judy and her family also operate In Loving Hands Adult Day & Health, caring for seniors with Alzheimer’s Disease and dementia and children and adults with developmental disabilities.
“I look at my purpose for still being here as God’s purpose,” she said. “I don’t take anything for granted. He’s allowing me to be a good steward — to see about others, even in my condition. I’m still able to give, and I’m still able to love.”
Screening can help catch breast cancer early and may improve outcomes after treatment. Learn more about mammograms and schedule one at a location near you.
IN THE PHOTO:
Judy Robinson overcame breast cancer three times to run service-oriented businesses with her sister, Wendy Favors (not pictured), and her daughters. Pictured from left to right: Tamara Robinson, Somer Robinson, Judy Robinson and Brittia Childs.

Wellstar Celebrates MyChart Milestone
Wellstar Health System has recently hit 1 million active users on MyChart. When we deployed this electronic medical record patient portal in 2015, we were the first Georgia-based health system to offer the service to patients.
Since then, MyChart has transformed the way patients interact with their healthcare information and clinical team by giving them 24/7 access at their fingertips. Patients became active participants in their care, both during their hospital stay and at home. Research shows that empowering patients to take control of their health leads to lower costs and better clinical outcomes.
MyChart’s "Open Notes" feature also allows patients to go to appointments and ask questions without having to worry about writing down information. Our physicians type up all notes and attach them to the records, allowing patients to review everything once they get home. If additional questions come to mind, patients can also ask them directly on the portal.
"I love MyChart and that I keep everything organized. What medications I'm taking, I can order them easily. I can text the doctors and Sharon at Ryan Cantwell's office, the nurse there," said Frank Ryan, who has used Wellstar to navigate through his health journey for several years.
"At Wellstar, we work as a team to take care of our patients," Wellstar Family Medicine Physician Dr. Ryan Cantwell said. "I enjoy being my patients’ quarterback and coordinating their care with other physicians. Through our electronic health records system, the referral process and communication with other specialists is easy and accurate."
That’s why Wellstar continues working on how we connect digitally with our patients to improve their experience and keep them in control of their health.
In 2018, we set the goal of reaching Epic’s top quartile for MyChart activation, which was 50 percent. At that time, the activation rate at Wellstar was 28 percent, with 420,000 patients signed up for MyChart. As of July 2022, the MyChart activation rate at Wellstar hit 65 percent.
Looking to the future, Wellstar is focusing on increasing and optimizing MyChart digital experiences, particularly around patient self-scheduling, e-Check, and MyChart bedside utilization for in-patient encounters. This high level of MyChart engagement ultimately gets Wellstar closer to our mission of providing world-class healthcare to every person we serve.
Click here to sign up for MyChart today and start taking advantage of all its benefits.

HometownCare
Before Atlanta Braves shortstop Dansby Swanson was a world champ, he was a little league player at Adams Park in Kennesaw. He honed his skills on the field at Marietta High School. And while you can now see him playing in front of 40,000 fans at Truist Park, he hasn’t forgotten his metro Atlanta roots.
Now he’s teamed up with Wellstar, another hometown institution, to stay at the top of his game — continuing a tradition that started the day he was born at Wellstar Kennestone Regional Medical Center.
“For my family, sports are a tradition,” Dansby said. “We have another family tradition too — looking to Wellstar for high-quality healthcare. Generations of our family came into this world at Wellstar Kennestone, including me and my siblings and my sister’s kids too.”
With convenient access to comprehensive care, Wellstar is there to cheer on Georgians like Dansby and help our communities thrive. Whether you’re running the bases or running your weekly errands, we all want to feel our best and stay ahead of health issues — and that starts with being proactive about our health.
“To live like an all-star, you’ve got to touch base with your primary care team regularly, at least once a year,” Dansby said. “Staying on top of our health means fewer surprises from left field.”
Your primary care provider will partner with you to create a personalized game plan to help you reach your health goals. Just like you may track Dansby’s home runs and batting average if you’re a Braves fan, you should keep up with your own health stats by staying up-to-date on screenings.
A few of your own stats you should know include:
Men are less likely than women to see their primary care provider regularly, but it’s still crucial they get regular screenings to stay healthy for themselves and the people they love.
“Men aren't always the best at making health a priority, but you need to know your numbers to keep you in the game and out of a slump,” Dansby said.
Men who are 50 or older should get checked for prostate cancer by their primary care provider. You may need to start screening even sooner, depending on your risk factors and family history. Ask your provider about setting up a screenings plan, so you can be proactive against prostate cancer.
With locations around metro Atlanta and West Georgia — and virtual care options available — Wellstar supports Braves fans all over Georgia. Find a location near you.
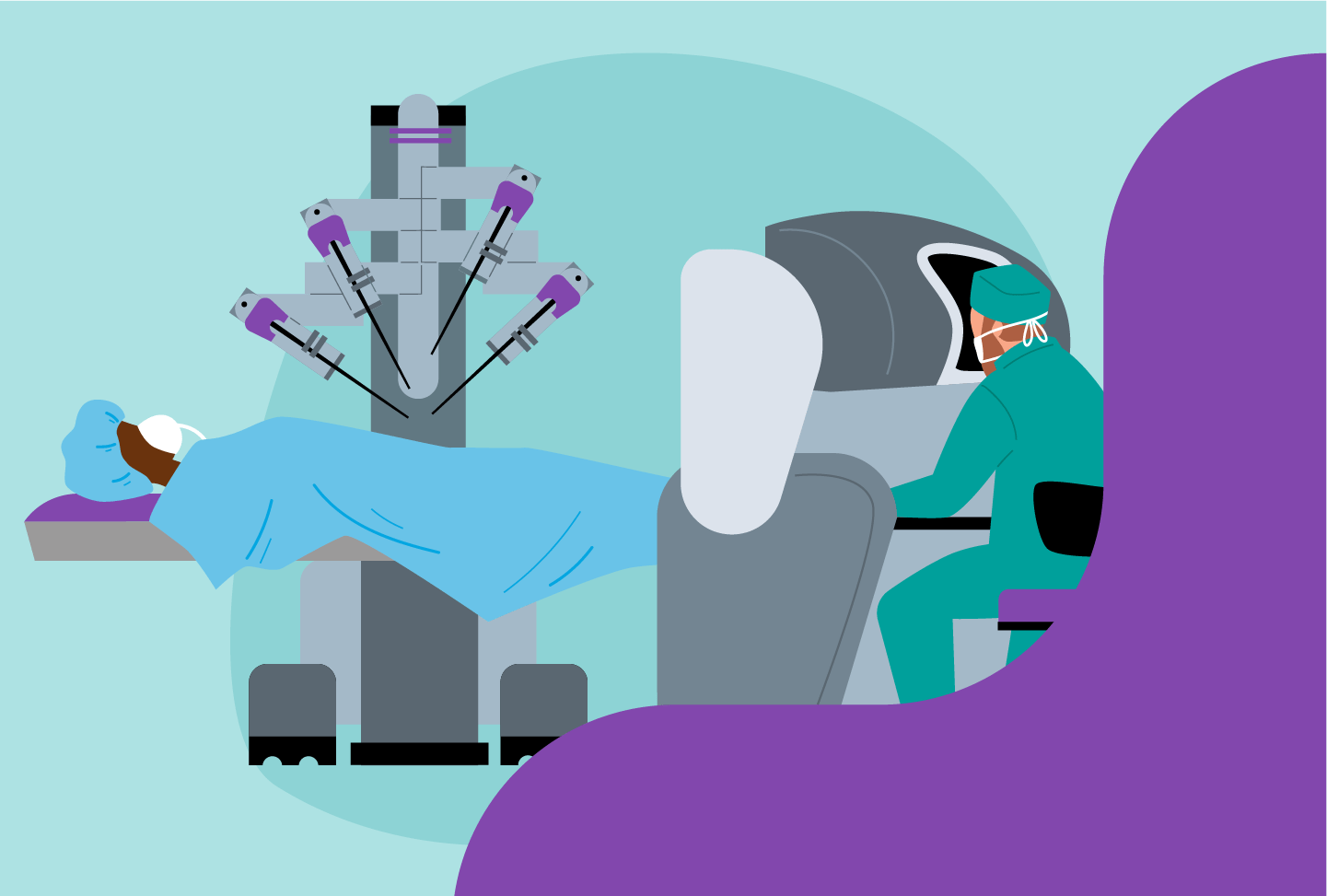
Wellstar Brings Robotic Surgery to the Paulding Community
For the first time, people in Paulding County and nearby communities have access to leading-edge robotic surgery close to home. Wellstar Health System launched a new robotic surgery program at Wellstar Paulding Medical Center.
“We’re thrilled to offer access to game-changing da Vinci robotic surgery at Wellstar Paulding Medical Center for the first time in history,” said Ralph Turner, Wellstar senior vice president and president of Wellstar Paulding Medical Center.
Robotic technology enables surgeons to make highly precise incisions smaller than the human hand can make — as tiny as a keyhole. As a result, people who have robotic surgery typically experience less blood loss, recovery pain and scarring.
“Robotic surgeries are minimally-invasive, which typically means shorter hospital stays and faster recoveries,” said Dr. Beau Dusseault, a urologist who leads the robotics program at Wellstar Paulding Medical Center.
He performed the first robotic surgery at the hospital, assisted by the $1.8 million da Vinci Xi Surgical System, on August 22. Dr. Dusseault has performed more than 440 robotic surgeries for prostate cancer and urinary tract conditions.
Experienced urologists and general surgeons are the first to offer robotic surgery at Wellstar Paulding Medical Center, primarily treating:
The surgical team named the robot “Rosie,” a reference to the robotic maid from the 1960s sitcom “The Jetsons.” It is one of 14 robotic systems patients can benefit from at nine Wellstar locations.
“While our robotic surgery program is new to Paulding, we have high-volume robotic experience that we are bringing from the other Wellstar hospitals,” Dr. Dusseault added.

Wellstar Health System Ranked #9 by Great Place to Work® and Fortune Magazine
Wellstar Health System, one of Georgia’s largest and most integrated health systems, has been ranked in the top 10 Best Workplaces in Health Care™ by Fortune Magazine in the “Large Company” category.
The Great Place to Work® Trust Index™ Survey results show that 81 percent of employees at Wellstar Health System say it is a great place to work, compared to an average of 57 percent for other U.S.-based companies. Additionally, 88 percent of Wellstar team members feel a sense of pride in accomplishments made at Wellstar.
To determine the Best Workplaces in Health Care list, Great Place to Work analyzed the survey responses of over 161,000 employees from Great Place to Work-Certified™ companies in the healthcare industry. The survey enables employees to share confidential quantitative and qualitative feedback about their organization’s culture by responding to 60 statements on a five-point scale and answering two open-ended questions. Collectively, these statements describe Wellstar’s positive employee experience, defined by high levels of trust, respect, credibility, fairness, pride, and camaraderie.
Learn more about working for Wellstar at careers.wellstar.org.

Wellstar Patient Thanks Her Care Team with Original Artwork
In 2001, Kathy Knopp had been suffering from terrible headaches. It all came to a head when Christmas Eve came and she could barely move her leg without physically dragging it. That’s when she knew it was time to go to the emergency room.
Spending Christmas Eve in a hospital waiting room was already not how Kathy thought her day would go, but when the doctor told her she needed emergency brain surgery and that she also had a collapsed lung, she knew what was about to unfold would be one of the most challenging times of her life.
Kathy spent the next three weeks in the hospital and though that would be difficult on anyone, Kathy shares the care she was given was the best and made a huge difference in her stay.
“I could not have asked for a finer hospital to care for me and am very thankful for all that the nurses and doctors did to aid in my recovery,” Kathy said.
After spending three weeks in the hospital, she went straight into rehabilitation for a month, and recovery was not easy.
Several years later when COVID hit and she had finally recovered, Kathy wanted to do something to give back to the nurses and doctors who did everything to make her long stay in the hospital more comfortable. This inspired Kathy to make something that they could look at every day and find hope. It’s what drove her to donate an original painting titled “The Land of Hope” created by Kathy and her fellow artist friends, Alison Keogler and Katie Kohu.
Kathy teamed up with the Wellstar Foundation to find the perfect location for her beautiful piece of art, which is now hanging in one of the Family Consultation Rooms at the Wellstar Kennestone Regional Medical Center Emergency Department, where she hopes it will bring peace and comfort to families and hospital staff during stressful times.
We are grateful for Kathy's perseverance and generosity. Learn more about the Wellstar Foundation at wellstar.org/foundation.

Did You Know Prostate Cancer Screening Has Changed? Find Out Why It’s Better Now.
Quick history lesson: In the 1990s, U.S. doctors adopted the prostate-specific antigen test—or PSA—to identify prostate cancer early, when it’s more treatable. While the PSA helped more men get diagnosed, concern was raised over the risks versus benefits of biopsies, procedures and treatment. In response, the U.S. Preventive Services Task Force gave a controversial recommendation against routine screening with PSA in 2012.
But with new evidence from a variety of credible studies, they changed their recommendation in 2017. The current Task Force recommendation focuses on men having a conversation with their doctors about their risk for prostate cancer and the risks and benefits of screening.
Prostate cancer is the most common cancer diagnosed in males after skin cancer. According to projections by the American Cancer Society, there will be twice as many new prostate cancer cases diagnosed as lung cancer this year.
“The prevalence of the disease cannot be ignored,” said Wellstar Health System Chief of Primary Care and Medicine Service Line Dr. Jeffrey Tharp, a primary care physician. “Early-stage prostate cancer has higher survivability than prostate cancer diagnosed in later stages.”
Dr. Tharp pointed out that while guidelines have changed, so have the way doctors diagnose and treat prostate cancer. An elevated PSA does not automatically mean a cancer diagnosis. And when cancer is diagnosed, some care options have no side effects.
Read on to learn:

Wellstar Health System Earns Recognition as a Healthiest Employer from Atlanta Business Chronicle
Wellstar Health System, one of Georgia’s largest and most integrated health systems, announces it has been named a “Healthiest Employer” by the Atlanta Business Chronicle in the “Extra Large Company” category, recognizing innovative organizations that have created robust and healthy workplace programs.
“Wellstar is dedicated to putting people first in everything we do, and that starts with our team members,” says David A. Jones, EVP and chief human resources officer at Wellstar Health System. “Prioritizing a culture of wellness is essential as we strive to deliver world-class healthcare to every person, every time. Wellstar is proud to be recognized by Atlanta Business Chronicle for our work in looking out for our team members' health and well-being. When we take care of ourselves, we can better care for our communities.”
The Atlanta Business Chronicle’s Healthiest Employer award is based on the analysis of over 60 scored questions with more than 600 data points for scoring and benchmarking. Wellstar was included in this prestigious list as an organization that takes proactive measures to “better the lives of employees through innovative programs and leadership commitment.” In 2022, wellness rooms were established across the system for team members to have a place to reflect, refuel and recharge during their shifts. Team members also have access to state-of-the-art fitness centers and onsite mental health resources.

Wellstar Comprehensive Aortic Program Provides Complete Care for Aortic Conditions
A new multidisciplinary program at Wellstar cares for people with aortic conditions, providing both emergency and non-emergent treatment.
The Wellstar Comprehensive Aortic Program brings together a highly-skilled team of experts, including cardiovascular surgeons and vascular surgeons, cardiologists, anesthesiologists, nurse practitioners and physician assistants. These providers share the common goal of diagnosing, treating and preventing aortic diseases and emergencies—making care more comprehensive and improving outcomes for patients.
“Traditionally, aortic diseases have been managed by multiple physicians spread throughout multiple specialties, which can lead to confusion, delays in treatment and competing treatment plans,” said Wellstar Cardiothoracic Surgeon Dr. James Ryan Burke. “Wellstar has created a single, multidisciplinary program to bring together aortic-specific disease expertise and leverage advanced technology.”
The aorta is the major artery that carries blood away from the heart to the rest of the body. If the aorta is ruptured, then blood does not flow to other areas like the legs, feet and brain, which can lead to lasting brain damage or death.
An aortic aneurysm is an abnormal bulge in the wall of the aorta. Aneurysms are often asymptomatic until they become large, rupture or dissect. However, an aortic dissection, when a tear develops on the inner wall of the aorta, is one for concern. Depending on the aneurysm location, the most common symptom could be one of severe chest pain, back pain, or abdominal pain. When an aneurysm ruptures or tears, it can lead to death within minutes or hours.
The aortic program takes a proactive approach to prevent aneurysms by monitoring and treating aortic conditions.
“Identifying aortic pathology early leads to better patient outcomes,” said Wellstar Cardiovascular Disease Specialist Dr. Jennifer Giuseffi.
The program’s team partners with patients to reduce their risk of an aortic emergency. Risk factors include tobacco use, being older than 65, obesity, high blood pressure, high cholesterol, history of coronary artery disease or peripheral vascular disease, family history of aneurysms, certain connective tissue disorders, and certain genetic conditions. Men are also at higher risk than women.
The team of aortic care specialists gets to know each patient and collaborates with them to create a personalized care plan to keep their aorta healthy.
“Every patient is different. Every aorta is different. The risk factors and complications with every aorta are different,” Dr. Giuseffi said. “Within our group, we’ll be able to address all of our patients’ issues individually.”
Our approach to aortic care brings together experts from multiple specialties, allowing patients to have all their questions answered and get multiple perspectives.
“All patients with aortic diseases being cared for at Wellstar will benefit long-term through the program’s unique collaboration of healthcare practitioners from cardiology, cardiac surgery and vascular surgery all working together to ensure the best possible care and outcomes for patients with these complex heart conditions,” said Vascular Surgeon Dr. Michael Corey.
While the program includes an outpatient component to help patients manage aortic conditions or recover from aneurysms or dissections, the systemwide team is also prepared to save lives and step into action during emergencies.
The program offers treatments including aortic root and aortic valve surgery, thoracic aortic surgery and thoracoabdominal aortic surgery.
If you experience any of these symptoms of aortic disease, call 911:
While the team performs procedures at Wellstar Kennestone Regional Medical Center, care teams at all Wellstar hospitals are trained in how to address aortic emergencies and transfer patients if needed. Wellstar Kennestone was the first hospital in Georgia and only fourth in the country to receive the highest certification in cardiovascular care—the Comprehensive Cardiac Care Center Certification—by The Joint Commission and American Heart Association.
To see a provider in the aortic program, patients can either be referred by their physician or call the office to make an appointment. The team will help patients determine which provider they should see first, depending on their health history or aortic condition. Call (770) 590-4180 to make an appointment or learn more about the program.
Accelerating the Progress of Cancer Care:
Republished Content: Atlanta Business Chronicle
This article was originally published on Atlanta Business Chronicle on August 19, 2022.
Cancer is the second-leading cause of death in the United States, with more than 600,000 people dying of cancer in the country in 2021. While the U.S. death rate, or the percentage of people dying from cancer, is decreasing — partly due to fewer people smoking — the number of cancer deaths is going up due to our aging population. All these statistics are behind the call to decrease cancer deaths by 50% in the next 25 years. Atlanta Business Chronicle recently talked with a panel of experts from Wellstar Health System and the American Cancer Society, headquartered in Atlanta, about ways to accelerate cancer care progress through scientific research, patient care, partnerships, early detection, diversity and inclusion, and local care.* (Remarks edited for clarity and brevity.)
Moderated by David Rubinger, market president and publisher, Atlanta Business Chronicle.

*Wellstar partners with Northwest Georgia Oncology Centers to provide world class cancer care close to home.
David Rubinger: Where are we today in the world of scientific research? Are we in a good place in terms of research dollars?
Kimberly Jackson: I think we’re in a good place, but we can always be doing better and that’s a fact. There’s no other nongovernmental, nonprofit organization in the United States that’s focused on finding the cause and cures for cancer like the American Cancer Society. We’re committed to continuously funding the best new and ongoing projects at institutions across the country. For instance, right now in Georgia, we are currently funding eight research multi-year grants that are totaling more than $6.3 million. In addition to funding and conducting research, we are mobilizing our grassroot network advocates to increase the funding for cancer research. We’re primarily supporting those investigators that are early in their career, who are doing the most innovative cancer discovery research.
Rubinger: While the aging population is causing the cancer deaths to increase, the average death rate for the population has actually decreased. What do you attribute recent successes to and how will we continue to fight cancer deaths in the future?
Dr. Steve McCune: The mission of the Wellstar and Northwest Georgia Oncology Centers partnership is to help cancer patients live longer by providing innovative therapies in their local communities. What we have seen in the last 10 years has revolutionized the treatment of certain cancers, particularly lung cancer and melanoma, with immunotherapy and targeted therapies, oral drugs that address a gene mutation. What may be a good way to think of that is it’s the Achilles heel for certain cancers: they have one gene that drives their growth. And there are, because of the research that has occurred, typically one or more drugs that may specifically treat that mutation and block it so that it no longer encourages the growth of cancer cells.
Next-generation sequencing makes it very easy and fast to sequence 400 to 500 genes in a tumor from an individual patient, so that you know exactly any gene mutations in that particular tumor. It’s the most individualized medicine you could have. That’s the reality and that’s very accessible for many patients.
Rubinger: Nicole, from the nursing standpoint on the front line with patients, how has immunotherapy changed the relationship between the patient and the healthcare provider psychologically?
Nicole Centers: From the patient care perspective, it’s very clear that patients are more involved in their care. They want to have more say in their care. When we can educate patients appropriately up front about all of their different options and their care along with their providers, they feel like they have more control. We know when patients feel more in control of their care, they’re more compliant to the plan of care. When it comes to immunotherapy and monoclonal antibodies that are given, they’re generally tolerated far better than chemotherapies of the past. That doesn’t mean everything can be treated with an immunotherapy or monoclonal antibody. However, when we have more options to give patients that they can tolerate better, then it kind of alleviates all of those nightmares of, “This is a horrific journey,” and, “It’s not going to work for me.” Overall, we have medicines that work with your body to fight the cancer in ways that we just haven’t had before.
Rubinger: The cancer “moonshot" is a term that excited everyone. Have you seen the concept of patient care change from when you first got into the field to where it is today?
McCune: I think it’s dramatically different. In some ways the moon shot has already happened and I'll explain what I mean by that.
Immunotherapy revolutionized the treatment of cancer. If you have a chemotherapy that kills 99% of cancer cells, well that means eventually that 1% keeps coming back. Immunotherapy can work for years, even after the actual immunotherapy has stopped. It’s not a vaccine, but it works in much the same way that a person’s own immune system actually can control or eliminate the cancer. I think that, in a sense, was the biggest game changer for the way that people were treated.
I started doing this about 20 years ago. And so most things that we treated were chemotherapy, very few things that were actually what we would have called targeted therapy or intelligently designed targeted therapy. The first drug was really coming out at that time called Gleevec, which treated CML (chronic myeloid leukemia.) I treated patients before that era who had to have a bone marrow transplant or they were basically going to die of CML. And now we think of CML as a condition that’s almost 100% survivable. We have eight different medicines that are commercially available for treating CML. It’s totally changed the future for some patients who would have had very poor outcomes otherwise.
Melanoma used to be very difficult to treat. Chemotherapy didn't work well. A treatment called Interleukin-2 worked for about 8% of patients and no one really knew why. It basically is an early immunotherapy but with a lot of toxicity. Now you have drugs like Opdivo, Yervoy, Keytruda, which are really the standard of care. Chemotherapy is rarely, if ever, used for melanoma.
There are antibody drug conjugates — something that basically has a payload on the monoclonal antibody, so it homes in on certain proteins on the outside of different cancer cells. That’s a way of delivering a toxin directly to the cancer cells with less impact on normal tissues.
There are companies all over the United States, from large to small, that are really driving the innovation in targeted therapies, antibody drug conjugates, so it’s an exciting time in oncology.
Wellstar has participated in trials for 15 years. In just the last three years, we have participated in cancer trials resulting in over 20 FDA approvals for either new medicines or new combinations of medicines. Usually, it is four to five years before something is FDA-approved. Now not everything’s approved, not everything works better, but it gives people hope and it gives them the chance to have cutting-edge therapies in their local communities.
Rubinger: Nicole, how have advances like these changed the psychology of talking with a patient with a cancer diagnosis?
Centers: I think it has changed. When I started in this field 20 years ago, we would say “the breast cancer down the hall" or “this is the breast cancer treatment.” Now we say, “the patient with breast cancer,” “the patient with lung cancer,” and we treat it as an illness that is part of the whole person, versus the whole person being the illness. That’s a different way that we think about things and that’s how we approach our patients differently when it comes to nursing.
There’s a very unique field inside of nursing called navigation. And one of the things that moonshot really promoted was something that we've been out here doing for a pretty good while, but it brought it to the center stage for all Americans to hear this word called a navigator. It meant someone that was going to guide you on your cancer journey. Several years ago, there was just one kind of navigator and they tried to do the whole care path, but we at Wellstar recognize that there’s lots of pieces to people who could have cancer, people who are being tested for cancer, and those patients that actually have cancer. So we have screening navigators, we have diagnostic navigators, and we have actual care trajectory navigators, which are oncology nurse navigators. We have over 15 of those in our system and some of those specialize by tumor type and some of those are more generalized.
What they do is they actually bring the whole person into view during their care. It means if you have childcare or if you have your parents, that you're taking care of first, or that transportation is an issue, these navigators work with you and your provider as well as your payers, whether it’s insurance or if you don't have insurance, we try and get you on insurance — to be sure that those things that would affect your compliance to the plan of care, they're helping you resolve.
It’s great if you can come in for your treatment. But if your dog has to be walked at two o'clock every single day and your treatment starts at noon, then we need to help you get a dog walker. We need to help you link to resources. For years there have been resources out there that patients didn't even know to utilize. And so organizations have this money that’s sitting there trying to help patients, but no one to link them to it. Navigators link patients to community resources, to national resources. The American Cancer Society has this really great program that will offer patients free rides to go get their cancer care, and most patients don't even know about that. But you talk to the navigator and they're like, “Wait, I have them on speed dial” because they get to know what those resources are, and they can help patients keep their appointments and keep a total life balance.
When we look at that, what that does is it makes their care more effective because they're more compliant to the plan of care.
The other thing navigators do is to help timeliness of care. So if two providers talk and say “we're both going to go see Sally Sue,” or whoever your patient is, and they turn to the front desk and say, “be sure we get this patient on the schedule.” However, the front office staff may not be aware the appointment doesn't meet the latest benchmark for timely care. So what a nurse navigator does is say, “Wait, we have some timeliness to care parameters that we know are best practice.” And they work with that provider or that office to help expedite those appointments.
The best part of navigation is it really brought care back into the patient’s community. Patients didn't understand what was available to them in their community. They thought you had to go to an academic center in a large city that cost them lots of money because they had to stay in hotels or take a flight or go get a car, because there’s so many patients in the states that don't have valid transportation that can take them two hours away. Navigators help patients understand what’s available in their community and the care that they can receive. They can also link them to clinical trials, arrange for assisted lodging and help patients get the best care out there to survive their cancer.
We've also seen an uptick in clinical trials because the navigators say, “Do you remember when your doctor talked to you about clinical trials? Do we want to circle back on that? And do you want to go talk to your doctor again?" They're reinforcing that education.
Rubinger: Let’s move to another topic: the second opinion. The second opinion might be local, but if you have the resources, it might be at Sloan Kettering, MD Anderson or Mayo. Is there less of that going on today because local providers are able to provide that level of confidence in what the care is going to be? Twenty years ago you would have maybe run to Houston.
McCune: I think people still do, but maybe for a different reason. I think they have more information and more knowledge and they're not just running to Houston, they're running to a specialist in Houston or New York or Atlanta. I say, “Hey, you're not stepping on my toes. I want you to get a second opinion. I can help you get that, more than just a cold phone call. Let me try to get you to the right person.”
At Wellstar, we do have Mayo Clinic Care Network e-consults available. That’s a pretty easy way to get a quick question answered if we need a specific answer or a second opinion without someone having to travel somewhere.
In addition to second opinions, we believe in collaborative care. We have groups of cancer experts who diagnose and plan treatments together in tumor boards so patients have the best outcomes. In Specialty Teams & Treatments (STAT) Clinics, multiple cancer specialists meet with the patients and their families in one place on one day to help them get questions answered. This helps them start treatment faster so they have better outcomes.
Centers: At Wellstar, 300 cancer specialists in our network can collaborate with each other. When they do request second opinion e-consults from the Mayo Clinic, it is free to patients which is a really nice thing because they usually have to pay for second opinions.
Rubinger: Kimberly, when I think of the Cancer Society, I think of the research dollars going to help cure cancer. But as we were talking earlier about how it helps with driving patients to treatment, the society’s partnerships with a Wellstar or other healthcare systems may be less well known. Can you address that?
Jackson: Collaboration is absolutely critical. So many cancer patients and their families are facing barriers and challenges that are too complex for just one organization to address on its own. To help overcome those barriers, we unite organizations in partnership to improve the lives of people facing cancer.
One example, we have Hope Lodges all over the country where individuals and a family member are able to stay for free and they're wonderful. It’s a great resource for our patients and their families.
Another example is we partner with Wellstar and other health systems in Georgia to provide those transportation grants that Nicole talked about and service to people who need it the most.
For some people with cancer, transportation is a challenge and it creates that barrier to receiving the treatment that they need. Many of them need daily or weekly treatment and often over the course of several months and the need was particularly pronounced during the pandemic. We were able to provide funding to 251 health systems across the country to alleviate that financial burden of transportation.
Another way we mobilize the cancer community on both the national and the local level is through our mission-critical roundtables. We're providing organizational leadership and expert support to multi-organizational roundtables focused on breast, cervical, colorectal and lung cancer, HPV vaccination and patient navigation. Each roundtable has a shared vision to support people to prevent and support and survive cancer. It’s a proven model close to home. Wellstar Health System was a key partner in launching our Georgia Lung Cancer Roundtable, whose primary goal is to improve screening rates and lung cancer outcomes.
Rubinger: Our society has come a long way in terms of reducing smoking. What are the trends in lung cancer that you're seeing? Does it primarily impact your older patients or is it across the age spectrum?
McCune: It can be any age and certainly there are people who are non-smokers who are much more likely to have a lung cancer that is driven by a single gene mutation and those are usually treatable with targeted therapy, which is typically an oral drug. So, in one sense, lung cancer is a disease of people who have smoked for a long time, 30 or 40 years. But it’s also a disease of nonsmokers. I do think people are generally smoking less. I remember people used to smoke in the pediatrician’s office when I was little. Things have changed dramatically.
There is a very active lung cancer screening program at Wellstar through the thoracic surgeons and the pulmonary physicians. It looks at people who have had some smoking history, who are typically at more risk for developing lung cancer. They'll have a low-dose screening CT scan, and we do see a number of lung cancers get discovered earlier. That’s a worthwhile initiative when something is surgically curable, as opposed to it’s gotten so advanced that people are having symptoms.
Rubinger: During the pandemic, I didn't see my doctors as often. None of us did. It was harder to access healthcare the way we did before. What has that done?
Centers: The pandemic did change us. A lot of screening procedures at the beginning of the pandemic were paused, but we were still able to quickly to return to those services. But the temporary delay made some patients think that screening wasn't as important as it once was. We really worked hard to get the message out there about the importance of early detection.
We use a lot of automated tools like our lung nodule software to help us identify nodules in patients who come into our system for other reasons and have those incidental findings. We also work with our church network here at Wellstar. We work with BLKHLTH in Atlanta, and there’s lots of healthcare organizations that are reaching out to their communities to get people back to screening.
We at Wellstar have made a very concerted effort to go back out and say, “We have kit testing that you don't have to come into the hospital to have done. You can do that at home. Let us help you get the kits.” We reopened our screening mammography centers with all the safety protocols in place. And then we called the patients and said, “Hey, you missed your cancer screening.”
We did see an initial dip because if you're not screening, you're not finding it, as cancer usually doesn't hurt. So most people don't know that there’s something in there growing. Now we're seeing patients come in with later stages, or more advanced tumors than we traditionally would have seen. That’s because of the lag in screening.
Rubinger: Kimberly, is this consistent with what you've been seeing?
Jackson: Yes it is. Early during the pandemic, cancer screening rates decreased dramatically and an estimated 35% of Americans missed routine cancer screening due to Covid-19-related fears and care disruptions when many facilities reduced or suspended services. Screening rates remain below historical averages. In addition to the coronavirus, top barriers to screening are that individuals have no symptoms, procrastination, lack of recommendation, cost, and no insurance. During the pandemic we worked with healthcare systems to address the issue as part of the “Get Screened” initiative. Through donor support, we were able to provide $2.2 million in grant funding to 77 health partners to implement quality improvement strategies to rapidly increase cancer screening rates and reduce the barriers that have been exacerbated through the pandemic. Wellstar was one of our partnering health systems in the Get Screened initiative. They were able to increase their breast cancer screening rate by 6.8 percentage points, which resulted in over 44,000 people in Georgia being up to date with their breast cancer screenings.
Rubinger: One of the crises in our society is the ability that people have to access care. When you think about those things from the DE&I perspective, where do we see the biggest challenges and where are the biggest opportunities?
Jackson: While the pandemic is shining a light on the issue, the reality is if we were focusing on having more diverse physicians, nurses, etcetera, if we were focused more on removing the barriers and investing more, we would have fewer people who are getting diagnosed at later stages, or, you know, unfortunately losing their lives to cancer. That’s a fact. There’s an opportunity right now that we cannot shy away from. The evidence is there to show the tie between the impact on an entire community by ensuring equitable health for all by focusing on the ones that need the most is actually equalizing and improving the health of the community itself.
Rubinger: I'm curious what role can the employer play?
Jackson: The employer, they have team members and staff that make up the community that we're seeking to serve. So what they can do immediately is educate the employees on the resources that are available on the prevention side. They can also make prevention a priority and establish norms of only offering healthy snacks, for example.
As well, they can encourage employees to go to their doctors, and also for the top leaders to serve on these boards and these councils of the hospitals and organizations like the American Cancer Society, to be aware and to stay ahead of the issues and to be informed and proactive about helping the community.
Centers: There’s really three ways to look at equitable care, and it’s not a one-path journey. First off, there’s a screening environment and the diagnostic environment, getting people to the services where they are and getting them access to care.
The second part is a mistrust of the healthcare system, which is ingrained in many of our societies across the U.S., so educating them to the safety parameters we have in place to ensure that all patients have equal access to care.
The third component is to teach our healthcare providers, be they nurses, medical assistants, physicians, about diversity and the things that happen to patients who maybe don't look like you, that walk through the door. What we know is, especially among our patients of color, that when they come in, sometimes their complaints aren't taken as seriously as others. We see that in the national studies.
What we have to do is educate our providers and our healthcare workers, but also educate our patients to say “you are your own best advocate.” If you go to a doctor and you're not getting the care that you think that you need or you deserve, then you can go to another place or else you can reach out to your patient advocates at the facility that you're going to. At Wellstar, we have invested a lot of time and energy into educating all staff so that all patients who walk through the door regardless of their social standing, regardless of what they look like, regardless of their history, are all treated equitably, and we do our best.
Rubinger: Dr. McCune, anything to add on that topic?
McCune: Yes. We have a diverse group of research coordinators, both African-American and native Spanish-speaking, so I do think there are opportunities to narrow some of those health gaps. I will say the pandemic across the board affected clinical trial enrollment, because there are typically more procedures like more CT scans that a person has to go through to go on a clinical trial, than just receive what we would call standard of care therapy. So across the board, that is something that has reduced clinical trial participation and that is starting to come back.
But I do think you have to meet people where they are. We obviously have a health system that covers some urban to rural areas in Georgia. One of the things that we're able to do is take clinical trials to people who are as far west as Carrollton, as far north as Cartersville, or closer to the Atlanta area in Marietta, Austell and Douglasville. We're expanding that research network as well.
Not everybody can drive two hours. Not everybody has a family member who can drive them when they're too sick. Access to care is a huge list of things that don't sound like much but a ride to the doctor’s office, a ride to a CT scan is the difference between someone getting care or not getting care. It’s things that seem little but are really not.
When you were talking about what can corporations do, I'll just say, it seems like most people’s experience is very dependent on whether the human resources person is nice to them. From the patient’s point of view, either “they're working with me and I can show up,” or “if I have a bad day, I can just stay home,” or “they fired me yesterday.” So maybe just a little bit of grace there. People have their federally mandated leave but they need more than that. They need a little attitude of caring or just going the extra mile, to help somebody get through their cancer treatment. They'll probably be a better employee and grateful if you treat them nicely.

Wellstar Recognized for Expert Patient Care
Wellstar is dedicated to serving our communities with high-quality care that’s conveniently located and accessible when it is needed most.
Several Wellstar facilities have been recognized in the U.S. News & World Report Best Hospitals rankings for providing world-class care in a variety of specialties, including cardiology, neurology and cancer care. Hospitals ranked as high-performing in an area of care are in the top 10 percent in the country.
Our team is grateful to be recognized for our care and looks forward to continuing our mission to enhance the health and well-being of every person we serve. To learn more about care at Wellstar, call (770) 956-STAR (7827).
Wellstar Cobb Medical Center was recognized as high-performing in treating:
Wellstar Douglas Medical Center was named high-performing in treating:
Wellstar Kennestone Regional Medical Center was ranked 32nd in the nation for rehabilitation services and the hospital ranked ninth in the state overall. It was also named a Best Regional Hospital and was recognized as high-performing in the following procedures and treatments:
Wellstar North Fulton Medical Center was recognized as high-performing in treating:
Wellstar Paulding Medical Center was named high-performing in care for:
Wellstar Spalding Medical Center was recognized as high-performing in treating:
Wellstar West Georgia Medical Center was named high-performing in treating:

STAT Clinic for Head & Neck Cancer Care Comes to North Fulton
Wellstar now offers advanced care for people with head and neck cancer—a complex disease that is often aggressive and requires coordination amongst multiple cancer experts. The new STAT Clinic for Head & Neck Cancer opened on the campus of Wellstar North Fulton Medical Center on August 11, 2022.
People with all types and stages of head and neck cancer have access to expert care and advanced treatments that are typically only available at academic centers. Treatments available in North Fulton include complex excision and reconstruction with microvascular free tissue transfers as well as CyberKnife radiation treatments.
In Wellstar’s STAT Clinics—short for Specialty Teams and Treatments—patients can see multiple cancer subspecialists to be diagnosed, have questions answered and finalize a treatment plan in a single day. This reduces the need to drive to different locations and helps the patient start treatment faster.
“The concept of multidisciplinary care is tried and true and shown to be effective for cancer patients,” said Dr. Fiyin Sokoya, the head and neck cancer surgeon who co-founded the North Fulton STAT Clinic for Head & Neck Cancer. “This model decreases the time to proceed and receive care.”
First, a group of medical specialists including a head and neck cancer surgeon and facial plastic surgeon, a radiation oncologist, a medical oncologist, a pathologist and a neuroradiologist review the patient’s pathology and imaging as a group to diagnose, stage and create a personalized treatment plan.
Next, the patient and their family meet one-on-one with the head and neck cancer surgeon, radiation oncologist and medical oncologist. This is an opportunity for the patient to learn about the recommended treatments and ask questions.
“Traditionally, patients must drive to several different appointments to learn the stage of their cancer, meet with different specialists and make decisions,” said Dr. Nagender Mankan, the dedicated medical oncologist in the new STAT Clinic. “At that point, four to five weeks have gone by. In STAT Clinic, we are expediting the complicated decision-making process.”
The patient also meets with a nurse navigator. This specialized nurse helps coordinate many aspects of care for the patient including scheduling appointments and connecting patients with support team members, such as a registered dietitian, a speech therapist or a dentist who may help relieve irritation in the mouth and throat.
When a STAT Clinic patient needs surgery, Dr. Sokoya is one of only a few surgeons in the region to perform complex excision and reconstruction with microvascular free tissue transfers.
“North Fulton has now become a destination center for head and neck cancer treatment because of our ability to offer advanced surgical care,” he explained. “The launch of this STAT Clinic is exciting, and it’s going to bring very advanced, high-level care to this area.”
Hundreds of patients travel to Roswell each year to seek Dr. Sokoya’s expertise from Georgia, Florida and Alabama.
Patients from all over the Wellstar system are seeing Dr. Sokoya for complex head and neck cancer management,” said Dr. Mark McLaughlin, a Wellstar radiation oncologist who co-founded the STAT Clinic.
Adding the new clinic allows us to invite those patients to come to North Fulton for evaluation and discussion of treatment options. Then we can work with their hometown doctors.”
Patients of the STAT Clinic who are candidates for radiation therapy have access to the latest CyberKnife technology at Wellstar North Fulton Cancer Center. The CyberKnife radiation suite is one of just two in the entire metro Atlanta area.
People with complex head and neck cancer such as large or recurrent tumors often benefit from CyberKnife radiation therapy. The technology minimizes radiation exposure to healthy tissue and limits side effects while shortening treatment courses. Normally patients receive five to eight weeks of radiation therapy. In many situations, they can complete their radiation course in as few as one to five treatments with CyberKnife.
“This highly advanced technology treats advanced head and neck cancers,” Dr. McLaughlin said. “You don’t have to go all the way into Atlanta.”
STAT Clinic for Head & Neck Cancer at Wellstar North Fulton Medical Center is located at 4500 Hospital Blvd, Suite 120 in Roswell, Georgia. For more information or to schedule an appointment, call the nurse navigator at (770) 751-2556.

BacktoCampusCare: What to Know About Anxiety
Whether it’s your first time on campus or you’re a seasoned college student, the start of a new school semester can be exciting, stressful and a little scary all at the same time.
Between finding classes on campus and fitting in with new friends, you may be feeling anxious about the upcoming semester. Keep in mind, new-school-year nerves are normal and there are resources to help you—including a check-up with your Wellstar primary care physician as well as on-campus counselors.
“Anxiety often goes unrecognized and undiagnosed,” said Wellstar Physician Dr. Andrew Doyle. “It’s not always recognized or talked about because people think it’s a normal part of life. But when anxiety interferes with completing homework, socializing or working at your job, it’s not necessarily normal. It’s helpful to have someone check it out.”
Signs of anxiety can also include difficulty sleeping, abdominal pain, headaches, significant changes in appetite or an explosive temper.
“There are effective treatments that make a difference for students including lifestyle changes, medication and therapy,” Dr. Doyle said.
Getting enough sleep, exercise and healthy food are highly important, and Dr. Doyle also recommends planning downtime from social media and life responsibilities.
“Therapy and role-playing can help you recognize your stressors and think through how to handle them ahead of time so you can face those situations,” he said. “For example, on exam day, start with positive self-talk. You can say, ‘I’m feeling nervous. I have a headache and an upset stomach. I know that’s because I’m anxious. I’ve taken many tests before and I can do this so I don’t need to worry about it.’ Breathing exercises before the test can help you stay calm. You can also plan ahead of the test to do something enjoyable afterward and to focus on that instead of the stressor.”
To help you start the semester off feeling mentally strong and physically healthy, here are some wellness tips to get you off to your best school year yet.
From medical appointments to personal safety, follow our tips to prepare for college and prioritize your health.
Heading to college can be a big transition, and you may feel anxiety about the upcoming changes, especially during a pandemic. But don’t be afraid to ask for help if you need help getting ready or adjusting.
Talking to your Wellstar is a great place to start, whether your concerns are about physical, emotional or mental health. Our health partners are here to support you and can connect you with specialists to keep you feeling well.
Book your annual physical today and be sure to bring up any questions or concerns you have with your doctor.

Wellstar Enhances Interpretation Services to Serve Diverse Patient Population
Wellstar's interpreting team partners with clinicians to ensure that culturally and linguistically diverse patients, including those who are deaf or hard-of-hearing, have access to communication and information in all aspects of their healthcare.
Effective communication, which includes verbal, nonverbal and written, is an essential component of quality care, successful treatment plans and patient safety. Communication errors can have negative and even life-threatening consequences. We integrate literacy, culture and language access to improve healthcare quality for diverse populations.
In addition to staff interpreters, Wellstar has partnered with Martti to provide remote interpreting services both on video and telephone. Martti offers many benefits, including access to 250 languages, an average of 30 seconds to connect with an interpreter, and top-of-the-line equipment in hospitals and outpatient practices, with user-friendly technology. Wellstar is also making network upgrades to optimize the connection on calls with interpreters, which will be especially beneficial for deaf or hard-of-hearing patients who use video calls to communicate with their interpreters.
Our team is comprised of professional interpreters and experienced translators. Wellstar is the only health system in the state that has nationally certified American Sign Language interpreters on staff. An interpreter must understand cultural nuances, be proficient in at least two languages and follow professional interpreting ethics and best practices.
Being bilingual alone does not qualify someone to be a professional interpreter. At Wellstar, for a bilingual team member to interpret in their department, they must complete medical interpreter training and pass the same proficiency assessment we require of our full-time interpreters. Like interpreters, the translator's skills are assessed for written language proficiency. Proof of competency for our team includes training in the following areas:
If you are within the Wellstar Health System, your care team can assist in finding an interpreter for you. If you are in the community or at home, you can call Wellstar’s Direct Access to an Interpreter line at (470) 944-7300. This line is staffed by interpreters, in multiple languages, who can assist patients to communicate with their provider’s office or the appropriate Wellstar department. You simply provide the interpreter with the Wellstar phone number you would like to reach.
For more information or questions about these or other language access services, please contact [email protected].

Wellstar Mejora Los Servicios de Interpretación Para Atender a Una Población Diversa de Pacientes
El equipo de interpretación de Wellstar trabaja en asociación con los médicos para garantizar que los pacientes cultural y lingüísticamente diversos, incluidos los sordos o con pérdida de la audición; tengan acceso a la comunicación y estén informados en todos los aspectos de su atención médica.
La comunicación efectiva, que incluye verbal, no verbal y escrita, es un componente esencial de la atención de calidad, los planes de tratamiento exitosos y la seguridad del paciente. Los errores de comunicación pueden tener consecuencias negativas e incluso mortales. En WellStar integramos el acceso a la alfabetización, la cultura y el idioma para mejorar la calidad de la atención médica para diversas poblaciones.
Además de los intérpretes de planta, Wellstar se ha asociado con Martti para brindar servicios de interpretación remota tanto por video como por teléfono. Martti ofrece muchos beneficios, incluido el acceso a 250 idiomas, un promedio de 30 segundos para conectarse con un intérprete y equipos de primera línea en hospitales y consultorios ambulatorios, con tecnología fácil de usar. Wellstar también está realizando actualizaciones de red para optimizar la conexión en las llamadas con intérpretes, lo que será especialmente beneficioso para los pacientes sordos o con pérdida de la audición que usan videollamadas para comunicarse con sus intérpretes.
Nuestro equipo está compuesto por intérpretes profesionales y traductores con experiencia. Wellstar es el único sistema de salud en el estado que cuenta con intérpretes de lenguaje de señas americano certificados a nivel nacional. Un intérprete debe comprender los matices culturales, dominar al menos dos idiomas y seguir la ética y las mejores prácticas de interpretación profesional.
Ser bilingüe por sí solo no califica a alguien para ser un intérprete profesional. En Wellstar, para que un miembro bilingüe del equipo esté habilitado para servir como interprete en su departamento, debe tomar el curso de entrenamiento como intérprete médico y aprobar la evaluación de aptitudes que exigimos a nuestros intérpretes de tiempo completo. Al igual que los intérpretes, las habilidades del traductor se evalúan para el dominio del idioma por escrito. La prueba de aptitudes de nuestro equipo incluye capacitación en las siguientes áreas:
Terminología médica, especialidades, anatomía y fisiología, afecciones médicas, patología, síntomas y tratamiento, pruebas médicas y procedimientos de diagnóstico, abreviaturas y acrónimos médicos
Si se encuentra dentro del Sistema de Salud WellStar, su equipo de atención puede ayudarlo a encontrar un intérprete para usted. Si se encuentra en la comunidad o en su hogar, puede llamar a un intérprete a la línea de acceso directo de Wellstar al (470) 944-7300. Esta línea cuenta con intérpretes, en varios idiomas, que pueden ayudar a los pacientes a comunicarse con el consultorio de su proveedor de salud o el departamento de Wellstar correspondiente. Simplemente proporcione al intérprete el número de teléfono de Wellstar con el que desea comunicarse.
Para obtener más información o preguntas sobre estos u otros servicios de acceso de idioma, comuníquese con [email protected].

Donor Spotlight: Imogene Walraven Waldrop - A Legacy of Giving
As a longtime resident of Paulding County, Imogene Walraven Waldrop has a passion for giving back to the community that she called home for years – the place where she made so many memories with her brother, Bobby, and sister, Doris, and where she and her husband spent the early years of their marriage together. Unfortunately, illness has taken the lives of many of Ms. Waldrop's loved ones, which is why she is so dedicated to uplifting the well-being of her community by bolstering healthcare services and enhancing access to care.
In the fall of 2021, Wellstar Paulding Hospital was designated a Level IV Trauma Center by the Georgia Department of Public Health. Level IV Trauma Centers demonstrate the ability to provide advanced trauma life support prior to transfer of patients to a higher-level trauma center when necessary. This added community resource was made possible by gifts to the Wellstar Foundation from generous members of the community like Ms. Waldrop. In 2018, she also made a substantial contribution to the hospital’s new infusion center, aptly named the Imogene Walraven Waldrop & Charles W. Waldrop Infusion Center. The 2,860-square-foot facility provides patients undergoing cancer and other medical treatments with world-class care conveniently located within their community.
“After witnessing both my brother and sister having to travel long distances to receive cancer care, I realized how critical it was to have these resources in Paulding,” Ms. Waldrop said. “Through the Infusion Center and now the Trauma Center, Wellstar is making leading-edge healthcare available to people when and where they need it most – that’s something I’m happy to be a part of.”
Ms. Waldrop’s donations to the Foundation were made through planned gifts, which allow donors the flexibility of contributing to the causes most meaningful to them while supporting their financial goals and creating a long-lasting legacy.
“I have enjoyed working with the Foundation and take pride in knowing that 100 percent of my gift will stay right here in Paulding,” said Ms. Waldrop. “I’m thankful for the opportunity to make a difference in my community that will benefit people now and the generations to come.”
The Wellstar Foundation is grateful to Ms. Waldrop for her dedicated partnership and philanthropic support. Through the generosity of corporations, organizations and individuals like Ms. Waldrop, the Foundation is addressing Georgia’s most pressing challenges through a strategic focus on health equity, behavioral health, innovation and workforce development. To learn more about the Foundation’s strategic initiatives or to discuss whether a planned gift may be right for you and your family, visit wellstar.org/foundation or email [email protected].

BackToSchoolCare: Helping Your Child With Stress & Anxiety
The new school year comes with a lot of change for children—a different classroom, teacher, peers, learning material and routine. These changes can cause stress and anxiety in some children and teens, especially if they struggle in school and dread going back.
Kids and teens of all ages can feel stress at times, and that’s normal. It’s essentially a signal to get ready for what’s coming. With typical back-to-school stress, a parent or caretaker can help adolescents start the school year with confidence—and gain important coping skills—with the following tips.
Stress can be good for kids. But on the other hand, chronic stress and anxiety that lasts for more than a few weeks aren’t healthy. In recent years, Dr. Doyle has noticed a growing number of adolescents, especially females, have anxiety.
“It’s normal to have stress; it’s not normal to have anxiety,” said Wellstar Pediatrician Dr. Andrew Doyle. “Understandably you get nervous with new situations that make you uncomfortable, but you’re still able to do it and have fun. Significant anxiety starts to interfere with a child or teen’s ability to do what they need to do—homework, school, social situations. That’s when it’s helpful to get it checked out.”
In addition to having difficulty participating in and completing activities, signs of anxiety in children and adolescents can include difficulty sleeping, abdominal pain, headaches, significant changes in appetite or an explosive temper.
Effective treatments include lifestyle changes, medication and therapy. For example, lifestyle changes can include getting enough sleep, exercising, eating a healthy diet and planning downtime from social media and life responsibilities.
“Therapy and role-playing can help you recognize your stressors and think through how to handle them ahead of time so you can face those situations,” he said. “For example, on exam day, start with positive self-talk. You can say, ‘I’m feeling nervous. I have a headache and an upset stomach. I know that’s because I’m anxious. I’ve taken many tests before and I can do this, so I don’t need to worry about it.’ Breathing exercises before the test can help you stay calm.”
Another way to begin the school year right is to check in on your child’s emotional and physical health. Wellstar pediatricians will get to know your child and help them live their healthiest.
“I try to do whatever I can to help our patients and families so that when they leave my office, I've given them something to hold onto that is going to make life better for them,” Dr. Doyle said.
Find a pediatrician near you and book your child’s back to school exam so they can start the year strong.

Wellstar Douglas Hospital Earns Advanced Certification
Wellstar Douglas Hospital recently attained advanced certification as a Primary Heart Attack Center (PHAC) by The Joint Commission and The American Heart Association. This means the hospital offers patients the next generation of cardiac care.
“Our cardiac experts in Douglas County are dedicated to doing what is best for the patient,” said Dr. Joshua M. Willis, Medical Director of Cardiac Catheterization Lab at Wellstar Douglas Hospital. “The Joint Commission certification shows that our cardiac program is designed to help people having heart attacks receive the fastest, most evidence-based care.”
Wellstar Douglas Hospital has 24-hour-a-day coverage to treat heart attacks. The hospital’s team communicates with first responders, so patients can get diagnosed and treated as fast as possible upon arrival at the hospital by ambulance.
“Everything we do is centered around giving each person the best chance for positive outcomes,” Dr. Willis said.
The hospital’s team aims to get patients diagnosed fast by performing cardiac tests within 10 minutes of arrival at the hospital. For patients who need surgical intervention, Wellstar Douglas Hospital’s interventional cardiologists perform percutaneous coronary intervention (PCI) — a minimally-invasive procedure that restores blood flow to the heart — within a 90-minute-window.
According to Gene Morris, Director of Cardiac and Vascular Services, the cardiac team has performed 2,500 PCIs since the program launched in 2012.
Wellstar Douglas Hospital is also designated as an Emergency Cardiac Care Center (ECCC) Level II by the Georgia Department of Public Health.
To learn more about Wellstar Douglas Hospital, please visit the hospital webpage.

Wellstar Appoints Chief Experience Officer to Drive People Centered Care
Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, has hired Susan Grant as executive vice president and chief experience officer. Grant will begin her role on July 1 and will be focused on creating holistic, curated experiences that power the continued development and growth of Wellstar’s system of care. She will work closely with Dr. Hank Capps, Wellstar’s Chief Information and Digital Officer, as well as operations leaders across the system to advance digital experience and integration to enhance care model innovation.
"Wellstar Health System has made significant drives to remain on the cutting edge of medical service through our care and dedication to patient experience. Initiatives and programs that define our care often involve addressing the unique needs of each patient and community to be both as effective and compassionate as possible," said Candice L. Saunders, president and CEO of Wellstar Health System. "The more advances we make in the field of medical technology, the more effort we must give to unify these innovations into a holistic experience that benefits not only our patients, but our doctors, nurses, and practitioners as well. Grant’s highly knowledgeable background will help us define and develop that experience across our system."
Grant has operated in healthcare for over 30 years. Her wealth of experience in various roles such as Executive Vice President and Chief Nursing Officer at Beaumont Health in Detroit, Michigan, has led to incredible achievements, including leading the nursing practice of over 10,000 nurses across all care settings and overseeing successful Magnet redesignation of two hospitals. In addition, she helped secure the initial designation of four of eight hospitals in the system at that time.
Grant received her Doctor of Nursing Practice from Vanderbilt University, a Masters in Psychiatric/Community Mental Health Nursing from the University of South Carolina and her Bachelor of Science in Nursing from the Medical College of Georgia. She is currently the chair-elect of the Building Health Systems Excellence expert panel with the American Academy of Nursing, is a member of the Nurse Executive Council for The Beryl Institute and serves on the Board of Directors for the Daisy Foundation Board.
Existing Wellstar Health System programs such as Catalyst by Wellstar, the Wellstar Clinical Partners Program, and the Hospital Quality & Efficiency Program are key components of Wellstar’s dedication to Patient Experience. By increasing the systems, programs, and access to critical care needs, world class technology and care, and highly skilled staff and care practitioners, Wellstar continues to grow its ability to provide both meaningful care outcomes as well as world class care that matters – PeopleCare.
These programs and partnerships have revolutionized the way our patients and our staff engage with medical treatment, from enhanced training techniques, to employee wellness centers dedicated to mental health, to additional family support for hard-working professionals within the system.

BackToSchoolCare: Checking in on Your Child’s Health
As you prepare for the new school year, give your child a positive start by completing your own homework assignment—checking in on their health.
Before heading back to the classroom, prioritize your child’s physical and emotional well-being with a visit to your family’s Wellstar pediatrician. Our compassionate pediatricians share your goal of keeping children healthy as they grow.
“In pediatrics, it’s always a relationship with the entire family, and it’s working in partnership with the parents,” said Wellstar Pediatrician Dr. Andrew Doyle. “We’re here to help them take care of their children.”
Preventative check-ups and screenings help children stay ahead of health issues, and our pediatricians will ensure your child is up to date on their vaccines and discuss which immunizations are needed to prevent disease.
“Our job is to make sure our children are growing up healthy and poised to be successful in life, and the best way to do that is to set them up well from the beginning,” Dr. Doyle said.
Your family’s pediatrician can also help you navigate health requirements at your child’s school.
“Pediatricians are knowledgeable about what forms schools require, and we can help parents with that process and ensure children are up to date on immunizations,” Dr. Doyle said.
Teach your child healthy habits so they can feel their best throughout the school year.
Show children how to wash their hands properly and remind them to do it frequently. Don’t send your children to school if they’re sick.
Children should have about 30 to 60 minutes of moderate activity every day. “Sometimes that's as simple as going outside to play or going for a walk and, especially for older kids, staying off screens and getting up to move,” Dr. Doyle said.
Teach children about good nutrition by encouraging them to eat plenty of fruits and vegetables and limiting sugary drinks.
Children aged 3 to 5 should get about 10 to 13 hours of sleep a day. Children 6 to 12 years old should get nine to 12 hours, and teenagers need about eight to 10 hours. “Children need more sleep than adults do, and unfortunately, just like adults, children are chronically sleep deprived,” Dr. Doyle said.
While the end of summer is often a busy time, planning ahead now will help ensure the whole family has a healthy, successful year.
Find a Wellstar pediatrician near you or locate an Augusta area provider to book your child’s wellness exam today.

Wellstar Health System and UnitedHealthcare Renew Relationship
UnitedHealthcare and Wellstar Health System have reached a multi-year agreement that restores network access to Wellstar’s clinicians, hospitals, health parks and clinics for people enrolled in UnitedHealthcare employer-sponsored, individual and Medicare Advantage plans, effective July 1, 2022. The agreement also expands access to Wellstar Clinical Partners, skilled nursing facilities, home health and hospice care.
UnitedHealthcare members can begin scheduling appointments with Wellstar today through MyChart or by calling their clinician’s office. For more information, call 770-956-STAR (7827).
“We know how important it is for patients to have local access to high-quality care from the doctors and hospitals they know and trust,” said Candice L. Saunders, President and CEO of Wellstar Health System. “This agreement will offer expanded access and more convenient options for patients with UnitedHealthcare insurance.”
“The care that Wellstar provides to our members is important and personal to them,” said Junior Harewood, CEO of UnitedHealthcare Georgia. “Our top priority throughout this negotiation has been ensuring the people and employers we’re honored to serve in Georgia have access to quality, more affordable health care, and this new agreement helps accomplish that goal.”
Wellstar’s mission is to enhance the health and well-being of every person they serve and provides access to compassionate, high-quality care to 1 in 6 Georgians through 10 hospitals, 300+ medical office locations, 9 cancer centers, 74 rehabilitation centers, 3 hospice facilities, 1 retirement village, 34 imaging centers, 18 urgent care locations and 5 health parks.
In Georgia, UnitedHealthcare serves nearly 1.2 million people through a network of more than 150 hospitals and nearly 35,000 physicians and other care providers.

Wellstar Kennestone Regional Medical Center Celebrates 72 Years of Service to the Community as it Prepares to Expand Care
Callie B. Andrews, FACHE, MBA, MSHA, Senior Vice President & Chief Operating Officer, Wellstar Kennestone Regional Medical Center and Wellstar Windy Hill
As Wellstar Kennestone Regional Medical Center celebrates our 72nd birthday, we are grateful for the opportunity to serve our growing community. We also are very grateful for the ongoing partnership and support our community affords us as we continue to evolve and grow to meet the changing healthcare needs of patients and families. This year has been a true testament of excellence in the quality of care we provide at Kennestone. Even through the challenges that the past several years imposed upon us, we have led by taking care of each other, our patients and our communities.
We are honored to continue to be recognized alongside Wellstar and its network of award-winning hospitals as we worked hard, together, to exceed the national standards of care. Among the awards and distinctions bestowed to Kennestone were the National Accreditation Program for Rectal Cancer, a first for Wellstar; Stroke Gold Plus award from the American Heart and American Stroke Associations; the very coveted Georgia Oglethorpe award; and several disease specific re-designations through The Joint Commission.
This year also brought a meaningful opportunity to continue to support our commitment to growth by preparing for the enabling work of a new, state-of-the-art bed tower. This new tower replaces the Baird building on campus and allows us to expand our patient care capabilities. The new tower is expected to be complete by late 2025 and open in 2026. In the meantime, we are engaging with our front line team members, providers, patients and a neighborhood advisory council and listening to their specific needs and desires as we consider this building’s amenities. Among such sought-after features will be private patient rooms.
Additionally, the tower will offer:
All of this will be enabled by technology to ensure the expertise housed within the tower is accessible to everyone. Sustainability is also a key factor as we finalize the tower’s design and materials.
Technology continues to be a priority area for innovation in the healthcare industry and at Kennestone Medical Center. For example, in 2021, we opened a new Hybrid CVOR which enables us to offer advanced cardiovascular operations and procedures with the most up-to-date technology available. Additionally, we have a Neuro Robot in the Vascular Institute and a a Cardiac Robot in the Cath Lab. These robots offer more precise tools for delicate procedures and assist surgeons with life-saving techniques, while also offering additional safety to physicians by reducing their exposure to radiation. This very exciting robotic technology also presents a tremendous opportunity for impact in the future. Robotics will enable our world-class physicians to leverage their expertise and expand our care to rural areas by assisting with operations remotely.
As we advance our mission through deploying a refreshed strategic plan, we look forward to innovating new care models to serve our patients, leveraging digital innovation and heavily investing in ambulatory spaces in order to increase our primary care footprint for easy access to care.
We learned a tremendous amount about disease crises as we watched how this hospital and the entire U.S. healthcare system pivoted to the dedicated care of Covid. In spite of the profound toll the pandemic had on employees everywhere, we remarked at the resiliency of our workers and clinical excellence of our providers and caregivers. We cannot thank you enough for the overwhelming show of support you gave our teams during that time. You nourished their minds and hearts and helped them thrive through incredibly challenging times.
Kennestone’s birthday and our new fiscal year represents a renewed hope in our journey, together, as our country continues to heal, grow and move past the devastating effects of Covid. It is more important than ever to stand in support of one another and continue to invest in resources for our staff. As the health and wellness of our teams continues to be of utmost importance, we continue to work with our staff to implement new and expanded employee programs, including wellness rooms and relief perks as a way to renew and refresh. Health equity also remains a priority. Our Diversity, Equity and Inclusion Team is dedicated to providing each team member with resources including book study groups, dialogue forums, videos and other tools which optimize technology resources for learning aimed at honoring every voice and ensuring equitable care to our patients and their families. This is a theme we carry through our community involvement, as well.
We remain excited to welcome new hires to Kennestone and Wellstar, especially new graduates who have chosen our medical center as their first clinical site. You are the reason we do what we do. We pledge to never stop striving to improve your health and wellness and remain committed to advancing care. Thank you for the trust you place in us to serve you and your loved ones. We are grateful to be your care provider of choice.
Wellstar Continues to Enhance Team Member Experience with Digital Tools
Wellstar Health System, one of the largest and most integrated health systems in Georgia, has selected Workday as their technology partner for finance, human resources and supply chain. Workday’s online platform will expand Wellstar’s ability to efficiently engage team members through improving how they gather information, distribute information throughout the system and improve existing operations. Wellstar’s continued investment in advanced tools is a part of its broader enterprise strategy that will power our transformation to a more digitally empowered workforce.
“As we look toward our health system's future, how we invest in our people is going to become more important than ever. With the integration of Workday, we will enable our staff to work more efficiently so that they can focus on what matters most – their patients,” says David A. Jones, executive vice president and chief human resources officer at Wellstar. “Our people are at the center of everything we do. We must care for them so that the best people choose to work and stay here.”
Nationally recognized for quality care and as a top employer of choice, Wellstar is committed to continuing to improve patient outcomes and the caregiver experience led them to evaluate new solutions for core administrative functions. Wellstar strives to make the workplace better for everyone who serves, and in doing so they continue to build upon the momentum of their digital transformation, helping to secure recent recognitions such as being honored with the Healthcare Information and Management Systems Society's (HIMSS) Stage 7 validation for its continuous efforts to improve patient outcomes through technological advancements. Stage 7 is the highest ranking an organization can receive, with less than 10% of hospitals nationwide recognized at this level. Wellstar is the only health system in Georgia to achieve this systemwide designation. This expanded capability will increase the communication and performance of team members as the organization continues its digital transformation across all facets of care. By designing the system with best practices and the caregiver in mind, Wellstar will continue to evolve to meet the changing needs of employees and patients.
“We are thrilled Wellstar has joined our growing Workday healthcare customer community. We look forward to helping Wellstar achieve their goals, learning from their extraordinary team and welcoming them into our customer forums as we partner together to help advance the future of healthcare," said Deana Kraft, Global Head, Healthcare at Workday.
With over 25,000 team members, 10 hospitals and more than 300 medical practice offices, Wellstar serves more than 1.7 million patients annually. Workday will provide Wellstar team members with an enhanced experience through greater accessibility and self-service capabilities ultimately reducing team member administration time so the team can focus on what matters – patient care.

Wellstar Health System Partners with Moth+Flame to Test Virtual Reality Leadership Training
Wellstar Health System is shaping the future of leadership training and development through an initial training program with Moth+Flame, an award-winning virtual reality (VR) provider and technology studio.
On May 18-19, 2022, Catalyst by Wellstar, the health system's global digital health and innovation center, along with Wellstar Leadership Development and Moth+Flame hosted the health system's first-ever VR-based leadership development training, focused on emotional intelligence. Across the two days, more than 100 Wellstar leaders participated in an immersive, VR-powered learning experience to prepare them to lead their teams through ongoing change in the healthcare industry.
"Partnering with Moth+Flame is an opportunity for us to gain a deeper understanding of how virtual reality can impact the way we care for and engage with our patients, consumers and each other," said Hank Capps, M.D., FAAFP, Wellstar's executive vice president and chief information and digital officer. "Our team members are essential in creating curated healthcare experiences, and we hope this initial training will showcase how VR technology can help our team be even more effective, compassionate and culturally competent leaders."
Studies show virtual reality learners learn four times faster than traditional methods and are 275 percent more confident to act on their training. This initial training aims to validate these numbers with a select group of Wellstar's clinical and leadership teams to elevate the organization's leadership development programming. At the end of the two-day training, Wellstar measured an increase in levels of confidence in the material learned and 97 percent of participants reported they would recommend this training.
"We've seen that investment in high quality training can improve retention across all industries," said Kevin Cornish, Founder and CEO of Moth+Flame. "By training in a simulated life-like environment, our product offers employees immersive training that helps them feel more confident. The metrics in Wellstar's launch show a continued trend that virtual reality is proving to be one of the most effective tools for professional development."
"Virtual reality and other technologies can open the door for us to take our leadership and team development to the next level," said Laura Dannels, Wellstar's chief talent officer. "These outcomes show us what's possible when we think outside of the box and embrace solutions from across industries. Our goal is to support our leaders as they guide their teams in creating exceptional consumer and team member experiences."
Unlike most typical VR experiences, Moth+Flame leverages real people instead of virtual avatars, which helps provide a more profound, meaningful experience for the end users. During the session, Wellstar leaders used headsets and iPads to immerse themselves in scenarios designed to prepare them to guide their teams through moments of change. This video describes more about the training.
"This 30-minute VR training on emotional intelligence was more effective and comprehensible than two full days of in-person training," said Michael Collins, Wellstar team member and participant.
Catalyst by Wellstar and Moth+Flame were connected through Engage, a first-of-its-kind collaborative innovation and corporate venture platform. Engage brings together industry-leading corporations, enterprise startups and universities with the shared mission of elevating Atlanta and the Southeast as a leading technology and innovation hub. Wellstar is proud to be the only healthcare organization to partner with Engage as the health system works to create new solutions to transform health and well-being.

Wellstar North Fulton Medical Center to Open Comprehensive Cancer Center
Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, announced yesterday it will open the Wellstar North Fulton Cancer Center in early 2023 on the Wellstar North Fulton Medical Center campus in Roswell, Georgia. The Center will also serve as one of only two locations in metro Atlanta featuring state-of-the-art CyberKnife® technology for radiation therapy.
Located at 4500 Hospital Blvd., the Cancer Center will offer comprehensive cancer services, including nationally-recognized, expert and experienced physicians; medical oncology; radiation oncology; imaging and many medical specialties all in one convenient location. Oncology surgery will continue to be performed at Wellstar North Fulton Medical Center, on the same campus.
“Wellstar North Fulton has been delivering expert, compassionate cancer care and support to North Metro Atlanta residents for many years,” said Jon-Paul Croom, president of Wellstar North Fulton Medical Center. “Our expansion of cancer services enables patients to receive the most advanced and robust offering of treatments available to beat cancer – close to home.”

Wellstar Celebrates National Cancer Survivors Day, Offering Hope to the Community
Wellstar Health System supports people with cancer throughout their journeys, from early screening to diagnosis to treatment. However, our encouragement and dedication to delivering world-class, compassionate care doesn’t end in remission.
Across our system, Wellstar honors the bravery and strength of survivors every day, rejoicing in each milestone. This National Cancer Survivors Day, we are proud to pay tribute to people who have conquered cancer while offering hope to those still fighting.
This year’s Cancer Survivors Day theme, “There’s No Place Like Hope,” exemplifies Wellstar’s commitment to being a steadfast source of encouragement for cancer survivors and fighters across Georgia.
“Cancer Survivors Day is a true celebration of life, healing and hope for the future. The special moment allows us to pause, reflect and cherish victories over cancer. It also gives an outpouring of support to people currently diagnosed with the disease — that way, they know they are never fighting alone,” shared Nicole Centers, executive director of the oncology service line & nurse leader at Wellstar Health System.
Several Wellstar facilities will host Survivors Day events — and you can be a part of the celebration.
Learn more about how Wellstar is fighting cancer in Georgia.
Wellstar Supports Child Literacy Through Community Collaboration
The Wellstar Foundation has joined the Literacy and Justice for All initiative, a coalition of leading organizations such as the Joseph B. Whitehead Foundation, United Way, Atlanta Speech School Rollins Center and Marietta City Schools — all committed to ensuring youth have the literacy skills needed to succeed in life. The goal of the program is ensuring that every child can read by third grade and has a foundation for growth in literacy.
Georgia ranks 41 out of 50 states for literacy*. According to the COX Campus, literacy is strongly correlated to zip code, race and ethnicity. The disruption in education due to the COVID-19 pandemic has further heightened the need for childhood literacy programs to ensure no child is left behind.
“We are honored to join this effort in creating a connected ecosystem with schools and early childhood educators to enhance literacy and create a national model that can be expanded to serve and support our country’s youth,” said Julie Teer, senior vice president of Wellstar and president of the Wellstar Foundation.
Through a grant from the Joseph B. Whitehead Foundation, Wellstar Kennestone Hospital and its affiliated OB/GYN and pediatrics offices will implement the Talk With Me Baby program and be part of a literacy ecosystem dedicated to healthy brain development for children.
The team at Kennestone will collaborate with families of babies born there to teach about the importance of building language from an early age. Families will be prepared with the resources needed to improve their child’s “language nutrition.”
According to the Talk With Me Baby program, families can teach their child basic language skills by using loving words, eye contact and facial expressions, as well as repeating words and phrases. Families can partner with their child’s Wellstar care team to learn more about how to engage with their children, and Wellstar clinical and nursing teams will be trained as Talk With Me Baby coaches.
This support will continue at pediatric patient visits as Wellstar partners with families of children from birth through the age of five to promote literacy. Talking, reading, playing and singing together help even the youngest children establish these skills.
Through philanthropy and community partnerships, the Wellstar Foundation fuels innovation and action to address the vital needs of diverse communities in Georgia. Philanthropic contributions are transforming healthcare and improving access for all within four focus areas: health equity, behavioral health, innovation and workforce. The Foundation’s participation in the Literacy and Justice for All initiative combines innovative techniques for early childhood development with health equity endeavors to ensure all parents are equipped with the knowledge to raise thriving children and improve their quality of life.
Teer says, “As a not-for-profit health system, our passion for people extends beyond the walls of our care sites and into the diverse communities we serve. Through collaboration with our partners, we are creating pathways for success to improve the health and well-being of all Georgians with the aim of creating a healthier state for everyone now and in the future.”
To learn more or make a tax-deductible donation, visit wellstar.org/give. If you’re preparing for the arrival of a new family member, learn more about prenatal care at wellstar.org/womenshealth. To find a pediatrician to keep your child healthy, visit wellstar.org/kidcare.
Wellstar Foundation Gala Raises Nearly $1 Million for Behavioral Health Services
The Wellstar Foundation raised more than $900,000 toward combating the behavioral health crisis facing Georgia during its 23rd annual Starlight Grand Gala on April 23 at The St. Regis Atlanta.
Sponsored by ApolloMD and Bank of America, the black-tie event was emceed by Condace Pressley, Director of Community and Public Affairs at WSB-TV, and included a cameo video from Atlanta Braves shortstop Dansby Swanson, both of whom were born at Wellstar’s flagship hospital in Marietta, Georgia, Wellstar Kennestone Regional Medical Center.
Atlanta Hawks Hall of Famer Dominique Wilkins also energized the sold-out crowd by hopping on stage to add two tickets to the auction for NBA playoff game four between the Miami Heat and Atlanta Hawks. Wilkins, who partners with Wellstar as a health ambassador, also shared impassioned words on destigmatizing mental health and how it has impacted his own family.
This message was echoed by Wellstar physician leaders Dr. Ryan Breshears, Chief Behavioral Health Officer, and Dr. Avril Beckford, Chief Pediatric Officer, who have witnessed firsthand the concerning rates of substance use, anxiety, depression and suicide among adults and youth rapidly increase throughout the pandemic.
Julie Teer, Wellstar Foundation President, said, “The Gala was a monumental step in helping our Wellstar Foundation bolster collaboration among healthcare workers, community providers, and private and public sectors to enhance the well-being of every community we serve; this includes a pivotal philanthropic focus on behavioral health which is needed now more than ever. Caring for one-in-six Georgians, Wellstar is not only uniquely positioned but committed to transforming healthcare for everyone in Georgia through corporate and community partnership.”
Kim Gresh, Owner and President of S.A. White Oil Company, Inc., was celebrated as Philanthropist of the Year and David Bottoms, President at The Bottoms Group and Chair of the Wellstar Foundation Board of Trustees, was presented with the Exemplary Service Award.
As one of the largest and most integrated not-for-profit health systems in Georgia, Wellstar is the state’s largest safety net health system and was recently ranked among Modern Healthcare’s top 10 providers for charity care in the nation. 100% of Gala proceeds support Wellstar’s commitment to expand behavioral health services across its 11 hospitals and every community it serves. To make a tax-deductible donation or for information on future Foundation events and corporate partnerships, visit wellstar.org/foundation.


Georgians Uplift Rural Communities Through Tax Credit Program
Access to care close to home is something many take for granted until that care is no longer available. Georgia’s rural hospitals provide critical care to residents when and where they need it. However, industry shifts and economic challenges have forced many rural hospitals to close their doors, forcing millions of people to commute — some for hours — to receive the care they need.
Recognizing this strain on rural hospitals and the communities they serve, the Georgia legislature launched the Georgia Rural Hospital Tax Credit program. Through this program, Georgia taxpayers receive a 100% state income tax credit on contributions made to qualifying rural hospitals such as Wellstar Sylvan Grove Hospital.
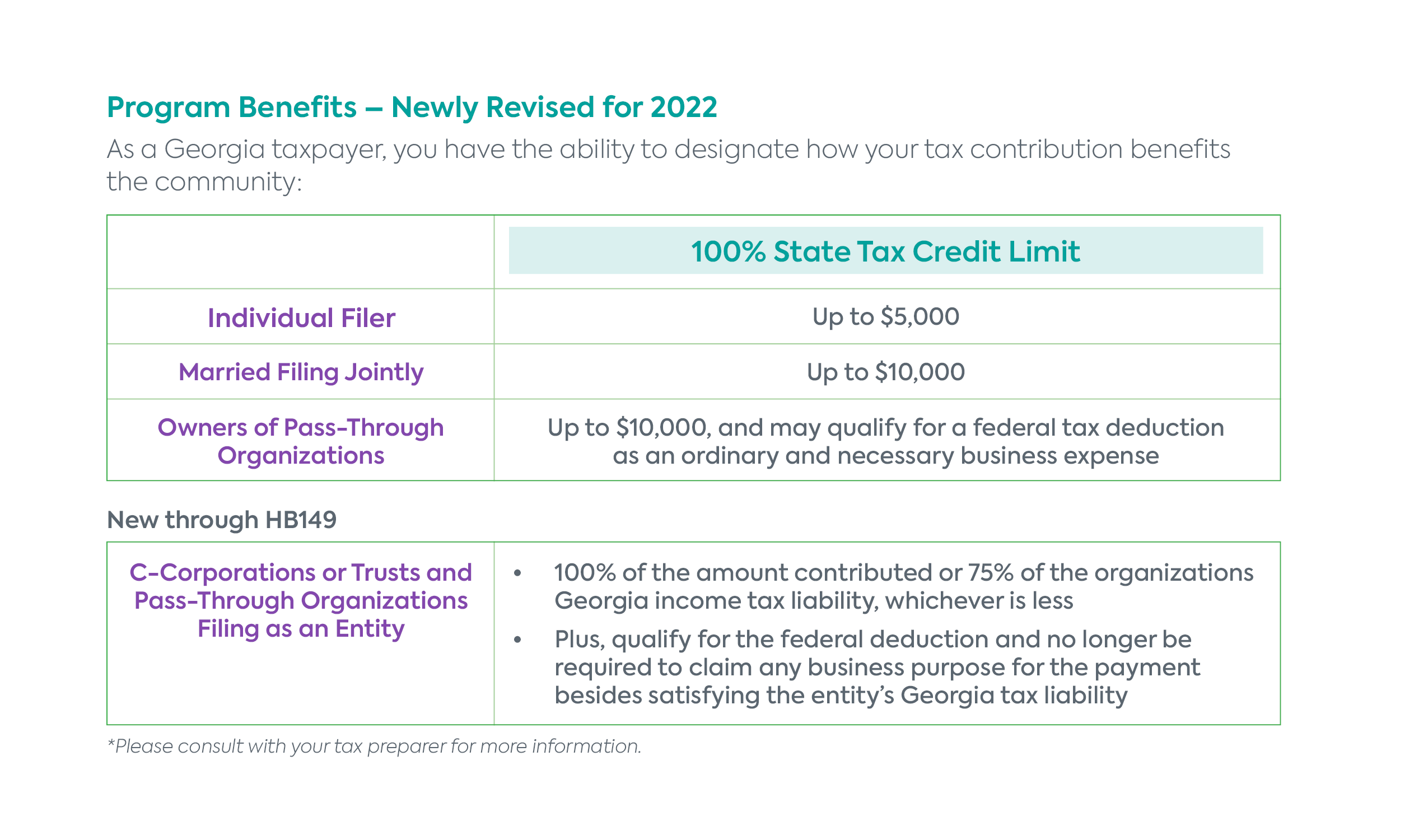
As in past years, contribution limits will be removed on July 1, 2022. Given recent enhancements and increased interest, the program is anticipated to reach its $60 million cap soon after the contribution limits are removed, making now a pivotal time for Sylvan Grove donors to pre-register for unlimited contributions. By registering your contribution early, you help ensure facilities like Wellstar Sylvan Grove Hospital receive the assistance they need.
Starting May 16, 2022 at 9 a.m., our administrative partner — Georgia HEART— will accept pre-registrations to be loaded on a first-come-first-serve basis once the limits are removed. The Wellstar Foundation is offering to assist Wellstar Sylvan Grove Hospital contributors with this pre-registration process. Contact the Foundation at [email protected] for assistance or click here to pre-register directly with Georgia HEART on May 16, 2022.
Since 2016, Wellstar Sylvan Grove Hospital has received a total of $10 million through this program. As facilitated through the Wellstar Foundation, every dollar has accelerated critical upgrades, including a full renovation of the hospital’s emergency department, radiology department expansion and leading-edge innovation, such as advanced CT scanning technology, that enhances physicians’ abilities to make better-informed medical decisions.
Advancements in treatments and technology benefit the residents of Butts County — patients like Mary “Lee” Nelson, a retired Butts County teacher who turned to Wellstar Sylvan Grove Hospital’s outpatient rehabilitation center for post-surgical physical therapy. The outpatient center was recently renovated with state-of-the-art equipment made possible through tax credit program contributions.
The former elementary grade teacher spends her retirement days traveling with her husband Bill, tending to her flower gardens and caring for her chickens. With such an active lifestyle, when Lee learned that she needed a knee replacement in 2021, she knew her local hospital would be able to provide the high-quality, compassionate care needed to get her back on her feet safely and quickly. Now, a few months after completing her physical therapy, Lee shares that she “feels normal again” and able to enjoy all the things that once brought her life so much joy.
Through corporate and community partnership, the Wellstar Foundation is fueling innovation and action to address the vital needs of diverse communities in Georgia, including urban, suburban and rural communities. Wellstar is committed to delivering world-class healthcare to everyone close to home. Philanthropic support of the Wellstar Foundation is advancing innovation and expanding resources to create a healthier Georgia for all. To learn more, visit wellstar.org/foundation or contact the Wellstar Foundation at (770) 956-GIVE (4483).
Wellstar Foundation Healthcare Innovation Series Event Addresses Workforce Development Solutions
As technology and healthcare are both rapidly evolving, Wellstar is leading the way in forging partnerships and fostering collaboration to find creative solutions.
The Wellstar Foundation’s Healthcare Innovation Series brings together thought leaders, community partners and industry experts to discuss the future of healthcare and how to better serve Georgians. The most recent virtual event focused on workforce development, a long-standing challenge for many industries, including healthcare.
The event, titled “Building a Healthy Healthcare Workforce,” was hosted by Wellstar President and CEO Candice Saunders, Julie Teer, senior vice president of Wellstar and president of the Wellstar Foundation, and David Jones, Wellstar’s executive vice president and chief human resources officer.
By the year 2030, Georgia could face a shortage of 50,000 nurses. The demand for providers is increasing faster than the pipeline of new healthcare professionals, and the COVID-19 pandemic has introduced new complications and challenges. To ensure that future generations of Georgians have access to high-quality care from expert providers, Wellstar and its community partners are dedicated to making progress in workforce development.
“Confronting these challenges and creating equitable access to care requires a healthy, strong and long-term pipeline of healthcare professionals,” Teer said during the event. “Bolstering our pipeline is critical for the economic prosperity of our local economies and to addressing deep-seated inequities in health.”
Keynote panelists and breakout session leaders included:
Attendees heard about workforce development challenges and how Wellstar and its partners are working to address them — through solutions like engaging youth in career exploration opportunities, forging partnerships with postsecondary academic institutions, and creating a positive, inclusive environment for team members.
Learn more about the Wellstar Foundation and how its strategic initiatives, which include workforce development, can transform healthcare.
Wellstar GME Internal Medicine Clinic Opens in Griffin
As Wellstar continues to invest in providing quality health care in our communities, primary care patients can now receive care at the new Wellstar GME Internal Medicine Clinic – which also serves as a residency clinic for physicians in Training. Located at 747 South 8th Street, Suite B in Griffin, the clinic, along with the Griffin-Spalding Chamber of Commerce, is hosting a ribbon-cutting event on April 26 at 12 pm.
The GME Internal Medicine Clinic is dedicated to delivering high-quality, evidence-based care to people in the community. “We are your partners in providing whole-person care offering prevention strategies to help you achieve and maintain a healthy lifestyle,” says Dr. Ashok Kumar Kanugula. “This may include routine checkups, managing chronic diseases, immunizations (influenza, tetanus) and age-appropriate screenings (bone density, blood panels), as well as treatment for acute issues, such as abdominal pain and respiratory infections. We can also provide information about nutrition, exercise and mental health.”
The clinic accepts a range of payment options and has established relationships with a variety of health insurance carriers. And to better serve the community, the clinic delivers services to those in need through Wellstar’s Financial Assistance Program.
In addition to providing care for patients, the clinic serves as a graduate medical education (GME) facility, training resident physicians. Residents will begin training at the clinic in July.

Wellstar Health System Honored With Coveted HIMSS Stage 7 Designation
Wellstar Health System is proud to announce it's been honored with the Healthcare Information and Management Systems Society's (HIMSS) Stage 7 validation for its continuous efforts to improve patient outcomes via technological advancements. Stage 7 is the highest ranking an organization can receive. With less than 10% of hospitals nationwide recognized at this level, Wellstar is the only health system in Georgia to achieve this systemwide designation, covering all of its 10 hospitals and nearly quadrupling the number of facilities with this designation across the state. Wellstar's five health parks and more than 300 outpatient facilities also received this distinction.
Wellstar was recognized as Stage 7 in both the Electronic Medical Record Adoption Model (EMRAM) and the Outpatient Electronic Medical Record Adoption Model (O-EMRAM) categories. HIMSS, the world's leading non-profit advocacy and accrediting organization in the healthcare IT industry, conducted a comprehensive review of Wellstar's technology advancements in information governance and compliance, IT security tools and controls, and identity access and management. National rankings are evaluated based on healthcare technology adoption within the organization on a scale from zero-to-seven, with zero being completely paper-based and seven being a fully electronic implementation across all health records and associated tools within the organization.
"Receiving this Stage 7 designation from HIMSS is validation of our fierce commitment to digital technology that benefits our patients. We are honored to be recognized for our dedication to implementing technology solutions that provide better outcomes for patients and improve overall effectiveness in quality of care," said Sandra Lucius, RN, MSN, vice president, Head of Care Platforms, Wellstar Health System. "As technology continues to advance, innovation to solve problems and seize opportunities will evolve and impact how healthcare is delivered and used. Wellstar will continue to transform healthcare through mission-driven technology innovation."
One example of technology innovation that contributed to Wellstar's receipt of the HIMSS validation is its clinical quality improvement ERAS program (enhanced recovery after surgery) proven to help post-surgery colorectal cancer patients. The combined efforts of Wellstar's care teams and patients as part of the ERAS program proved a significant 24% reduction in 30-day readmissions, a 61% reduction in pain medications used, and a patient satisfaction rate of 99%.
The organization will be recognized at the 2023 HIMSS Annual Conference & Exhibition April 17-21, 2023, at the McCormick Place in Chicago, Illinois.

Well Starts with Allergy Care
It’s that time of year again—flowers blooming, temperatures rising and people gearing up for outside activities in the warmer months.
If you’re one of the more than 50 million Americans suffering from seasonal allergies, you may take the yellow pollen as a telltale sign to stay indoors. However, that may also mean missing out on fun times with family and friends.
Instead of suffering with frustrating allergy symptoms for another season, take back control of your health with help from Wellstar.
If seasonal allergy symptoms—such as congestion, runny nose or itchy eyes—bring you down, don’t put off getting the proper care.
“Allergies tend to flare up in the spring and summer time,” said Dr. Oswaldo Henriquez, Wellstar ear, nose and throat (ENT) physician. “Allergies are a patient’s response to an environmental allergen or can even be present in the home, such as dust and pet dander.”
Other common causes can include seasonal changes or allergens like perfume and smoke inhalation.
Whether you suffer from seasonal allergies or a chronic condition like asthma, specialty care can help you stay on track.

Well Starts with Spring Screenings
When the weather starts to warm up, many people start getting ready for the spring season. Along with cleaning and decluttering your home, you should also spruce up the space you live in every day—your body.
When you prioritize your well-being and do the proper up-keep for your health, it may help you stay ahead of potential medical issues.
To feel your best this spring and beyond, we’re sharing our top tips to keep you healthy.
Setting our clocks forward can also be your reminder to set up a visit with your primary care provider.
“People should definitely add a wellness exam to their spring-cleaning checklist, regardless of age. Routine preventative care every year is very important,” said Dr. Nayab Dhanani, Wellstar primary care provider.
During a wellness exam, your physician will check your Foundational 4 Numbers—body mass index (BMI), blood pressure, blood sugar and cholesterol levels.
From there, your physician can help create a screening plan to help keep you ahead of chronic conditions or serious diseases. Recommended screenings may vary depending on your family history, gender and age as well as your physician’s orders.
“The importance of screenings is really to be proactive instead of reactive,” said Dr. Facia Dew, Wellstar primary care physician. “It’s better to know a person’s risk factors so we can screen accordingly. Our goal is to meet their unique medical needs and help them live a healthy life.”
Be sure to bring up any other medical concerns, health questions or wellness goals at the appointment. Wellstar providers are partners in your care, committed to keeping you feeling your best physically, mentally and emotionally.
Talking about colon health can feel a little uncomfortable, but getting screened could save your life. If caught early, colorectal cancer has a 91% survival rate.
Starting at age 45, everyone should get a colonoscopy. Those with a higher risk or family history of colorectal cancer may need to start screening even sooner.
Learn more about how well starts with clean colons.

Redefining Healing Experiences with Sound at South by Southwest
Each year a diverse group of artists, entrepreneurs and technologists join policy and business thought leaders from around the globe in Austin, Texas, for the South by Southwest conference and festival. This broad intersection of perspectives and personalities has proven to be fertile ground for big ideas to take root and thrive.
It is within this context that Wellstar Health System participated in the Health & Med Tech track to share how using immersive sound technology in a series of wellness rooms is helping frontline healthcare workers reduce feelings of stress and anxiety. This initiative is the result of a partnership between award-winning immersive audio company and software service Spatial, and Catalyst by Wellstar, Wellstar’s global digital health and innovation center.
During the panel, "Redefining Healing Experiences with Sound," Dr. Hank Capps, executive vice president and chief information and digital officer at Wellstar, shared how impactful the wellness rooms have been to frontline healthcare team members.
"The idea of bringing immersive sound into the wellness rooms and inviting team members who were in the midst of stress, in the midst of a battle, was one of the ways we believed we could make a difference. We went live with the wellness rooms earlier this year to unexpected success and utilization, beyond what we could have pictured," said Dr. Capps.
To help make this impact, the team was challenged to find ways to foster a calming environment without the use of screens, such as TVs. During a 12-hour shift of the near-constant monitoring of vital signs and patient records on computers and mobile devices, screens were something the team was looking to subtract, not add. This insight led to the innovative use of immersive sound technology invisibly imbedded within the walls of the wellness rooms. Team members can choose from a variety of soundscapes and transport themselves virtually to a calm beach, a rainforest with birds gently chirping, or to the bottom of the ocean.
The evidence-based use of sound/music to reduce stress and anxiety is well-documented but patients and consumers are largely unaware of it. In fact, a recent nationwide survey revealed that while only 28% of respondents were aware that sound/music is being used in targeted ways to improve physical and mental well-being, 73% were open to incorporating it as a therapy.

Increasing awareness could help this technology achieve wider adoption. With this pilot project, Wellstar became the first health system to incorporate immersive audio technology with Spatial in a clinical setting.
The response from team members has exceeded expectations.
The four wellness rooms equipped with Spatial technology have been used thousands of times in just over one month of operation. Initial data and anecdotal evidence suggest this component of the wellness rooms is particularly useful in helping Wellstar team members reduce feelings of stress and anxiety. As more is learned from this pilot, the team hopes to expand the use of this technology in patient-facing settings such as labor and delivery rooms or emergency department waiting areas.
Catalyst by Wellstar defines leading-edge, transformative solutions that enhance the health and well-being of people and communities with world-class results and impact. It is particularly meaningful that one of Catalyst’s first pilot projects is enhancing the well-being of people who have given so much of themselves in the service of their communities throughout the pandemic—Wellstar team members.

Well Starts with Clean Colons
For many people, talking about colon health can be a little uncomfortable. However, medical issues don’t just go away if you ignore them.
Being proactive about your well-being with preventative care can help catch colorectal cancer or another serious condition early, often before it becomes a bigger problem.
Wellstar is committed to keeping your colon healthy with preventative screenings and expert care, so you can continue to live well.
Early detection is the best prevention, especially when it comes to colon cancer. If caught early, colorectal cancer has a survival rate of 91%.
“Colon cancer is the second most common cause of cancer death in the United States, so it’s very important that everyone gets screened,” said Dr. Cameron Body, Wellstar gastroenterologist. “For an average risk person, screenings should begin at age 45.”
Those with a higher risk or family history of colorectal cancer may need to start screening even sooner. Talk with your provider to start a screening schedule — and stick with it to stay ahead of the disease.
Schedule your colonoscopy today.
During a colonoscopy, your physician will view the inside or your colon and look for polyps or any other abnormal tissue that could be cancerous. This preventative testing is key to catching colorectal issues at the start.
“A colonoscopy is the gold standard when screening for colon cancer. The procedure itself is not painful, and we make sure you’re comfortable throughout the process,” Dr. Body said.
“The goal is to do a high-quality exam with a good prep to find polyps when they’re small and get them removed to minimize the risk of them subsequently developing into cancer,” Dr. Body explained.
“For colon cancer, it takes a polyp about five to 15 years to evolve into an invasive cancer,” shared Dr. Carmen Klass, oncologist and hematologist with Northwest Georgia Oncology Centers. “If you have a colonoscopy every five to ten years, they can remove the polyp and it will never be declared an invasive cancer.”
“In fact, if all Americans did their screening colonoscopies every five to ten years, then the death rate for colorectal cancer would drop by 50%,” Dr. Klass shared, urging people not to put off the preventative screening.

UlyssesCare
If you looked up the word “active” in the dictionary, you just might find Ulysses Price’s picture.
Between serving on the tennis court, racking up strikes in bowling and learning new moves in martial arts, he defines life by what brings him the most joy: movement.
But all that changed when severe neck and shoulder pain entered the picture. Ulysses could barely do a double take let alone hold play doubles on the court.
“Not being able to do simple things like reach for a bowl in the cupboard or turn my neck were big limitations in my life,” Ulysses said. “I tried to tough it out. But when the pain was non-stop, that’s when I decided I needed medical attention.”
Ulysses turned to Wellstar’s neuro experts to help him take control of his health. Now, after a state-of-the-art neck procedure, Ulysses is back in action and doing his favorite activities — even better than before.
From diagnosis to surgery and recovery, Ulysses formed a lasting partnership with his Wellstar care team and knows he can face any health hurdle with confidence.
When pain became a constant part of Ulysses’ life, he sought help from his Wellstar primary care provider.
Ulysses' provider took his pain seriously. After an MRI revealed a serious spinal issue, he connected Ulysses with expert neuro care at Wellstar right away.
That’s when Wellstar Neurosurgeon Dr. Phillip Parry joined the team, determined to help put an end to Ulysses’ pain. Dr. Parry stressed how important primary care providers are when it comes to keeping a keen eye out for potential medical issues.
“The value of having a primary care provider who can identify neck and low back pain cannot be overstated,” Dr. Parry said. “Having these conditions addressed early by the right specialists is extremely important.”
Catching neurological conditions at the start is key to helping patients have the best outcome possible. The same was true for Ulysses, whose spine issues were interfering with his everyday life.
“Ulysses had a narrowing in the cervical canal of his cervical spine, the bony portion through which the spinal cord is transmitted,” Dr. Parry said. “As we age, virtually all patients develop some amount of this compression.”
“In Ulysses’ case, his spinal compression had become so severe that it was causing spinal cord dysfunction,” Dr. Parry explained. “His condition resulted in weakness in his hands, being unable to walk with confidence and feeling very unstable on his feet.”
Working together, the pair discussed the potential treatment options for his pain. Because Dr. Parry always kept an open dialogue, Ulysses felt comfortable being an active participant in his care.
“I always try to be proactive about any medical procedure and do my research to know as much about it as possible,” Ulysses said, sharing how Dr. Parry took time to answer his questions. “Dr. Parry listened and spoke with me about the most up-to-date procedures, and that made me quite comfortable with him as a person and a physician.”
Soon, they created a care plan that would help Ulysses live his healthiest life for years to come.

Wellstar Opens Wellness Rooms Across Facilities Benefitting Frontline Team Members
Frontline team members now have a place to reflect, refuel and recharge at work, funded by the Wellstar Foundation, with innovative technology provided by Catalyst by Wellstar and strategic design implemented by our Employee Wellness group.
Tucked away at nearly every Wellstar facility is a haven for team members to unwind from a challenging shift or stressful day. These Wellness Rooms, which opened in 2022, were designed to transport team members beyond the walls of their facility.
In the Wellness Rooms, lights are dimmed, soundscapes play lightly in the background and the air is filled with fresh, calming scents. Team members flow in and out of the room at their leisure with a tap of their badge, grabbing a healthy snack, a spritz of an essential oil, or a moment of stillness while enjoying the massage chair.
The rooms vary by size at each location, but every room is equipped with tools to provide a serene and safe environment for team members who find themselves in search of calm amidst what can sometimes feel like chaos.
Since opening, thousands of team members have benefited from the Wellness Room, utilizing the space as an outlet for stress management and as a resource for workplace self-care.
Brianna Arrington, an emergency department technician at Wellstar West Georgia Medical Center, recently found herself needing a safe place to process the tragic loss of a pediatric patient. Brianna was led to a Wellness Room by her leader and encouraged to take a moment to breathe.
“This quiet and relaxing space gave me the time to decompress from the anxiety I was feeling and helped me to calm down away from the situation. The Wellness Room was a tremendous help.” Brianna was able to return to her shift and continue serving patients the rest of the day.
Studies show that physically moving away from a hectic environment, even for just a few minutes, helps to regulate our emotional wellness. Thanks to Catalyst by Wellstar and through a partnership with Spatial technologies, some Wellness Rooms are piloting immersive sound technology which is proven to reduce feelings of stress and anxiety. Wellstar is the first health system to use such immersive AI-driven audio technology in a clinical setting. Spatial technology may even be utilized in patient-facing settings in the future, based on positive feedback from team members.
The Wellness Rooms were introduced as part of MyCare Rewards, an Employee Wellness benefit geared toward helping team members prioritize their mental, physical and emotional health. In total, the 16 Wellstar Wellness Rooms across our hospitals and health parks were a $1.5 million investment in the well-being of our team members. Thank you to the Wellstar Foundation for helping to make these rooms possible. The Wellness Rooms will continue to be a resource in times of need and moments of stress, providing a place of solitude to our team members who serve Wellstar patients and communities.

Wellstar Kennestone Regional Medical Center Earns Accreditation for Rectal Cancer Program
Wellstar Kennestone Regional Medical Center has earned a three-year accreditation from the National Accreditation Program for Rectal Cancer (NAPRC), a quality program of the American College of Surgeons. This accreditation demonstrates our commitment to providing personalized, high-quality cancer care close to home for patients in Georgia.
To achieve voluntary NAPRC accreditation, a rectal center must demonstrate compliance with the NAPRC standards addressing program management, clinical services and quality improvement for patients. Centers are required to establish a multidisciplinary rectal cancer team that includes clinical representatives from surgery, pathology, radiology, radiation oncology and medical oncology.
At Wellstar, rectal cancer patients have a multidisciplinary team on their side through every step of treatment. Each patient works with a nurse navigator to schedule appointments with specialists. Patients meet with a medical oncologist, as well as a surgical oncologist or colorectal surgeon. Imaging and lab tests are reviewed by a multidisciplinary board of rectal cancer physicians, efficiently providing patients with input from several experts in cancer care. During the course of treatment, that multidisciplinary board will continue to follow the patient and discuss the best next steps, tailoring care to fit each patient’s individual needs.
Additionally, the program at Wellstar Kennestone met standards addressing the clinical services that the rectal cancer program provides, including Carcinoembryonic Antigen (CEA testing), Magnetic Resonance Imaging (MRI) and Computerized Tomography (CT) imaging for cancer staging, which allow patients to start treatment within a defined timeframe. Rectal cancer programs accredited by the NAPRC undergo a site visit every three years and are also accredited by the American College of Surgeons Commission on Cancer.
“Our patients are surrounded by a team of experienced rectal cancer experts who provide the highest level of personalized care,” said Wellstar Surgical Oncologist Dr. Sahir Shroff, who serves as the rectal cancer program chair. “We are proud to be the first medical center in metro Atlanta to receive this important accreditation. Our pioneering efforts to adhere to the most rigorous standards and combine the latest technologies and techniques help us achieve excellence in rectal cancer care for our patients.”
Accreditation by the NAPRC is granted only to those programs that are committed to providing the best possible care to patients with rectal cancer. The NAPRC provides the structure and resources to develop and operate a high-quality rectal center. Accredited programs follow a model for organizing and managing a rectal center to ensure multidisciplinary, integrated, comprehensive rectal cancer services.

ScottCare
Every day, Scott Hullihen’s gaze falls on a very unique piece of art hanging in his home.
To the untrained eye, the spiraling streaks across the canvas could be mistaken for an abstract painting in a museum. But for Scott, it holds a much deeper, personal meaning: hope for a cancer-free future.
A closer look reveals a puzzling QR code in the corner of the print and, when scanned, it plays the very voicemail from his Wellstar radiation oncologist that got him through the most difficult days in his cancer journey.
“The picture is his voice in soundwaves. I get to see it every day,” said Scott. “It’s the most thoughtful thing I’ve ever seen in my entire life.”
The ebbs and flows of the piece show how he conquered the highs and lows of his difficult rectal cancer diagnosis, with support from Wellstar as the constant through it all.
Just like the highly personalized art print, his expert team of physicians formed a tailored care plan for Scott, right down to his DNA.
Together with his Wellstar team, Scott beat cancer and is back to living life to the fullest.
Scott was a typical guy in his 30s, working in technology and spending time with friends and family.
“Everything was normal,” he said. “I’d go to sporting events or concerts.”
But his diagnosis of colorectal cancer at just 35 years old was anything but typical.
“That was shocking,” he said.
In 2020, Scott’s stomach started hurting—and it didn’t stop. He started eating better and cut certain ingredients from his diet. He regularly rode his bike for 15 miles.
“I was getting in good shape!” he said.
But the pain continued, with an urgency to use the bathroom, constipation and blood. His doctor referred him to a gastroenterologist for a colonoscopy in August. Immediately after the procedure, he learned there was a tumor in his colon.
“It was a quiet car ride,” Scott remembered sitting silently next to his mother, who had driven him there.
That Friday, a biopsy confirmed it was cancer. Scott was immediately referred to the Wellstar Rectal Cancer Multidisciplinary Program, the first and only treatment center in metro Atlanta accredited by the National Accreditation Program for Rectal Cancer (NAPRC), a quality program by the Commission on Cancer.
After the weekend, Scott met with Dr. Sahir Shroff, a cancer surgeon.
“People raved about how good a surgeon Dr. Shroff is—I learned he was one of the best in the state,” Scott said. “He saved my life.”
The board-certified and fellowship-trained surgical oncologist reassured Scott.
“This is one of the most subspecialized rectal cancer programs in metro Atlanta,” he said. “Every person with rectal cancer is reviewed at our multidisciplinary meeting to provide the highest level of care.”
Select doctors are designated to stage and treat rectal cancer patients following evidence-based guidelines. The team includes colorectal surgeons, medical oncologists, radiation oncologists, gastroenterologists, pathologists and radiologists. Higher experience in treating rectal cancer leads to better outcomes for patients.
Scott also had a nurse navigator coordinate his cancer staging and treatment. Nancy Page answered questions and scheduled important appointments, such as CT scans and MRIs as well as meetings with various specialists.
A licensed Wellstar genetic counselor was also on Scott’s team. Amy Ekwurtzel found that Scott had two genetic abnormalities that make him slightly more susceptible to colorectal cancer. This information gave the team additional clues about the best way to care for Scott.
New Technology at Wellstar is Improving Outcomes for Complex Brain Bleed Patients
Wellstar is home to a new tool that is improving treatment for patients experiencing intra-cerebral hemorrhages, or bleeding strokes.
Wellstar Neuro Care has been on the cutting edge of minimally invasive procedures and surgeries for patients suffering with strokes and hemorrhagic strokes. This latest treatment offers minimally invasive surgery for a disease with devastating outcomes. The Artemis Neuro Evacuation Device uses a neuroendoscope — a small tube with a camera — that is inserted into the brain to reach the bleeding in areas of the brain that were previously unreachable by neurosurgeons. The clot is pulled out using the end of the tube, either with suction or a device that eats away at the clot.
Wellstar is a leader in this groundbreaking treatment — only a handful of health systems in the country offer it. Now, Wellstar patients can access this care close to home, which is especially crucial for brain bleeds — a condition that has been nearly impossible to treat in the past.
While 80% of strokes occur because a blood vessel in the brain or neck is clogged, these deep-in-the-brain, often fatal bleeding strokes can be difficult to access without damaging other parts of the brain. Often, these patients’ conditions are managed with therapies to keep the pressure in the head down. Bleeding strokes are dangerous as well — about 40% of people who experience one die within 30 days, and 75% are severely disabled, according to Wellstar Neurosurgeon Dr. Benjamin Zussman.
However, innovative technology like the FDA-approved Artemis system can improve those outcomes, and Wellstar is keeping that world-class care close to home. The tool has been used at Wellstar North Fulton Medical Center and Wellstar Kennestone Regional Medical Center.
“With the cutting-edge Artemis tool and new protocol for treating these difficult types of brain bleeds, we can be safe about the removal of these clots deep in the brain. It's a ‘finesse’ tool,” Dr. Zussman said. “We can access and remove the clot without damaging other parts of the brain, which can heal faster and better. It saves lives and saves quality of life.”
To learn more about stroke care at Wellstar, visit wellstar.org/neurocare.

Well Starts with Digestive Health
After taking a bite of food, you may not think about its journey through your body. From beginning to end, your digestive system is working hard to keep you healthy.
“Your digestive system plays an essential role in your well-being, helping your body to absorb nutrients, provide energy and fuel for your favorite activities,” explained Wellstar Gastroenterologist Dr. Arif Aziz.
That’s why it’s so important to do your part to protect your gut health.
Wellstar helps your digestive system stay on track, so you can feel your best and keep doing the things you enjoy most.
Your digestive system is made of an entire team of organs: the esophagus, stomach, intestines (small and large), pancreas, liver, gallbladder, rectum and anus.
“With so many parts working together, your digestive system requires expert care to stay well,” said Wellstar Gastroenterologist Dr. Inder Tandon. “Regular check-ups with your Wellstar provider can help identify potential digestive issues early.”
At a routine exam, your provider can screen serious diseases like colorectal cancer and help identify chronic and common digestive conditions.
“If specialized care is needed, your primary care physician can refer you to our expert team of gastroenterologists right away,” Dr. Tandon shared.
Find a Wellstar provider near you and schedule a check-up today.
Most colorectal cancer starts as a growth, or polyp, in the colon or rectum. Because polyps develop slowly over time, you may experience few warning signs and not know you have a medical issue for months, or even years.
That’s why it’s so important to get a colonoscopy—it could save your life. When caught early, colorectal cancer has a 91% survival rate.
People with average risk should have a colonoscopy starting at age 45. Those at high risk or with a family history of colon cancer may start screenings even sooner.

Finding Answers with Wellstar’s Autonomic Program
For nearly 30 years, Madge Hand knew something was going on with her body, but never determined what was causing her head-spinning health issues.
She had been in and out of several hospitals, looking for answers and trying different treatments, but her physicians couldn’t pinpoint the right diagnosis.
Now with the help of Wellstar experts, Madge is managing her dysautonomia – a disorder of the autonomic nervous system, which controls involuntary body functions like heart rate – so she can get her health back on track.
Madge, 79, started noticing symptoms when she was in her 50s. When she moved from lying down to sitting up or from sitting up to standing, her blood pressure would drop drastically — going as low as 60 over 30, compared to the normal level of about 120 over 80. Her doctors at the time were unable to determine the issue. She also experienced frequent nausea and was unable to eat.
She started rehab for general weakness. When she later broke her hip due to dizziness, she struggled to complete rehab because when she tried to walk, her blood pressure would drop and she would feel faint.
Madge has some answers and is now working with Wellstar’s autonomic program, one of only a few programs in the country certified to treat these disorders, to get back on track.
It turned out that Madge has dysautonomia — her autonomic nervous system isn’t working like it should, which affects her blood pressure and makes her feel faint. She is also managing her orthostatic hypotension, which causes her blood pressure to change suddenly when she stands. To prevent her blood pressure from suddenly dropping, she takes a steroid to keep it higher, along with midodrine, a medication used to treat orthostatic hypotension.
Only a few specialized programs are certified to treat autonomic disorders, but Madge can get the personalized care she needs close to home. Dr. Howard Snapper, a Wellstar cardiovascular disease specialist, is one of fewer than 50 physicians in North America board-certified to diagnose and treat these conditions. The autonomic center at Wellstar treats disorders of the autonomic nervous system, which controls involuntary body functions like heart rate, temperature, sweating and digestion.
Madge’s first appointment with Dr. Snapper was virtual, keeping care convenient. As Wellstar has one of only two autonomic disorder programs in the Southeast, patients can travel long distances to see specialists. Virtual appointments remove barriers to care for autonomic disorders, and the program recently expanded care with two new advanced practice providers.
“Sometimes, the symptoms of autonomic disorders can be confused with signs of other conditions,” Dr. Snapper said. “However, Madge had many of the common symptoms, including sudden changes in blood pressure, nausea and fainting.”
Madge said she is grateful that the health issues she has been dealing with for almost 30 years are now being addressed.
“Since I started working with Dr. Snapper, I feel so much better,” Madge said. “Now I can complete my rehab, and I know how to keep my blood pressure under control.”
Wellstar offers virtual appointments with the autonomic program, as well as in-person visits in Woodstock. To schedule an appointment with Dr. Snapper, call (678) 324-4400.
Preeminent Wellstar Leaders Join Inaugural Class of Georgia Nursing Hall of Fame™
Wellstar Health System is proud to announce that two extraordinary women have been inducted into the Georgia Nursing Hall of Fame™, produced by Georgia Nurses Foundation (GNF). Candice L. Saunders, FACHE, president and CEO of Wellstar, and Joyce McMurrain, MSN, RN, a nurse manager and coordinator of the Student Nurse Extern Program at Wellstar Kennestone Hospital, were honored along with eight additional nurses at a recent inaugural inductee ceremony. The 10 inductees are exemplary registered nurses who made or are making improvements to advance the nursing profession locally, nationally, and internationally.
Wellstar Kennestone Hospital’s longest-serving team member, McMurrain, has been a nurse for nearly 60 years, with 56 years—and counting—served at Kennestone Hospital. For many years McMurrain was the nursing director/executive nursing director for Women's Services at Kennestone, and she also served in that position systemwide. She later transitioned to director of special projects, and is now cultivating the next generation of nurses through her role as nurse manager and student nurse extern program coordinator. She uses her vast experience to guide new nurses and helps nearly 100 nursing students each year gain invaluable hands-on experience in preparation for nursing careers.
“Joyce has a natural ability to develop others and is committed to equipping students with the education and opportunities to excel in patient care and gain confidence in their job. She has been indispensable throughout Wellstar’s extraordinary growth and change and has contributed to its evolution to become one of Georgia’s largest and most integrated health systems,” says Saunders.
Saunders has served as a trustee of the American Hospital Association, chair of the American Hospital Association’s Regional Policy board for Region 4, and past chair of the Georgia Hospital Association. She was named one of Modern Healthcare’s Top 25 Women Leaders and among Georgia Trend Magazine’s 100 Most influential Georgians. A strong patient advocate who began her healthcare journey as a critical care nurse decades ago, Saunders has become a nationally recognized leader in improving community access to vital healthcare needs and enhancing the patient care experience. Saunders joined Wellstar in May 2007 as president of Wellstar Kennestone Hospital. She assumed the role of president and CEO in 2015, becoming the health system's first female CEO.
“Candice’s impact on the nursing profession is evident through her continued commitment to attract and retain top nursing talent. Candice began her career as a critical care nurse, and she remains passionate about investing in programs and supporting the growth and development of nurses at every stage in their career to ensure our patients and communities have access to high quality, compassionate care for generations to come,” says Dr. O. Scott Swayze, Chair, Wellstar Health System Board of Trustees.


Wellstar Paulding Hospital Expands Cardiac Services with New Procedures
Wellstar Paulding Hospital is now offering device implantations and catheter ablations in a new, state-of-the-art heart care lab, expanding the hospital’s cardiology services.
If you have a heart rhythm disorder and need a permanent cardiac device like a pacemaker or defibrillator implanted, Paulding’s cardiologists now offer these procedures close to home with qualified, compassionate providers who will take the time to get to know your needs.
Your care team will continue to support you after the device is implanted, too. Your electrophysiologist will ensure your device continues to work properly and check the battery life, and you’ll be able to work with our experts to create a personalized diet, exercise, lifestyle and medication plan to keep your heart in top shape.
Paulding also offers another solution for arrhythmia — catheter ablations. During this procedure, a small tube is inserted into a blood vessel, then guided to the heart to scar areas of tissue that are causing the abnormal heart rhythm. The scars block the electrical impulses that cause the abnormal rhythm.
Wellstar Cardiac Electrophysiologist Dr. Anand Kenia is performing these procedures at Paulding and sees patients in Hiram. To make an appointment with Dr. Kenia, call (678) 324-4444.

Wellstar Pediatric Emergency Departments
When a kid experiences a sudden medical emergency, it can be a stressful experience for both the parents and the child.
With four dedicated pediatric emergency departments, Wellstar Health System helps families have peace of mind that their little ones are in expert hands. Find a location near you:
Here, we know quick action, advanced services and compassionate care are essential to treating children like 12-year-old Alex. When he broke his leg during football practice, the injury could have caused lasting damage if he didn’t get the proper care.
“From the moment we arrived at the ED, the experience was absolutely phenomenal. He wasn’t treated like a number,” said Stephanie, Alex’s mother. “Knowing that the Wellstar team really cared about my son helped build my trust.”
Due to the severity of the break in Alex’s leg, surgery was a likely outcome.
“There was a 90% chance that my son would need surgery,” Stephanie explained. The odds seemed stacked against them.
However, the skilled pediatric team, led by Dr. Mark Brown, didn’t give up. They expertly set Alex’s break in a cast. Because it was done so well, he never required surgery to heal.
Now, months after the injury, Alex is on the mend and finishing up his last few physical therapy sessions. He will make a full recovery and can keep playing the sports he loves.
That’s because Wellstar knows kids aren’t just “mini adults.” Our pediatric specialists take time to understand your child’s unique needs, even in an emergency.
Our pediatric emergency departments are designed for our youngest patients, from birth to early adulthood. We deliver emergency care for a full range of pediatric emergency conditions, including:
Wellstar Pediatric Emergency Departments are powered by Pediatric Emergency Medicine Associates (PEMA) to provide high-quality care. Pediatric patients also have access to child life specialists who are trained to help children understand their injuries, medical care and even how to cope with difficult emotions.
In addition to our skilled medical team, each facility offers special equipment — like small casts and crutches — that are the perfect size for kids at any age or stage. Having the right technology, treatments and resources in place helps your child heal and feel better.
Medical emergencies are just as serious for children as they are for adults. If your child needs care for a life-threatening condition, call 911 right away.
For routine care and other specialty services, find Wellstar pediatric care near you.
Wellstar has a wide network of experts close to home. From well-child exams and specialty care to diagnostic testing and high-tech treatments, our team is here to protect your child’s health.

Wellstar Health System Partnership Provides Maternal Health Resources, Supports New Mothers
Wellstar Health System has partnered with Healthy Mothers, Healthy Babies Coalition of Georgia (HMHBGA) to provide maternal health resources in support of new mothers and birth givers in Georgia. Through Wellstar Community Health and the Wellstar Center for Health Equity, the partnership supports pregnant and postpartum birth givers and encourages positive maternal health and wellness by providing vital resources and education.
According to the 2019 HMHBGA State of the State Report, 58 percent of pregnancy-related deaths in Georgia were preventable. Wellstar’s participation expands HMHBGA’s Pickles & Ice Cream perinatal care package project created to help address pregnancy mortality. Started in 2021, the Pickles & Ice Cream program through Wellstar plans to reach 150 birth givers a month.
The free care packages will include:
Alongside these vital tools, educational information will include topics such as postpartum care planning and safe sleeping. As one of the key partners in this initiative, Wellstar will also distribute COVID-19 safety kits, including cloth masks, hand sanitizers, and informational materials to new mothers.
HMHBGA has impacted the health and well-being of women, children, and families for the past 48 years by supporting the community through direct services, advocacy, and community education.
The Wellstar Center for Health Equity is an extension of Wellstar’s long history of community engagement and allyship to provide people-centric care, and was formed to convene, activate, and support community partners and advocates to address, impact, and drive lasting change at a grassroots level.
Pregnant or postpartum moms, birth givers and organizations serving pregnant women may request a care package. For more information, please visit this link.

Wellstar Autonomic Center Expands Care for Autonomic Disorders
For people with autonomic disorders, finding treatment can be difficult. With only a few specialized programs in the country, getting care can require traveling a long distance.
However, patients in Georgia can access this crucial care close to home. Wellstar Cardiovascular Disease Specialist Dr. Howard Snapper, who sees patients in Woodstock, is one of fewer than 50 physicians in North America certified to diagnose and treat autonomic disorders.
Autonomic disorders, including postural orthostatic tachycardia syndrome (POTS), involve the autonomic nervous system, which regulates involuntary body functions like heart rate, temperature, sweating and digestion.
When people with POTS move from sitting down to standing up, their heart rate increases by about 30 beats per minute, but their blood pressure doesn’t change. This sudden increase can lead to dizziness or fainting. Most patients with POTS are younger women about 13 to 50 years old.
“Autonomic disorders are not that rare—about 2 to 3 million people in the country are affected—but they are often underdiagnosed because the symptoms can indicate other conditions,” Dr. Snapper said. “It can also be difficult to get the proper diagnosis and treatment to start improving these conditions.”
Dr. Snapper sees patients from as far as California, and Wellstar has one of only two autonomic disorder programs in the Southeast. With the addition of two new advanced practice providers, the program at Wellstar now has increased capacity and can help more patients live healthier and more comfortably.
To schedule an appointment with Dr. Snapper, call (678) 324-4400.

Wellstar Honors the Life and Legacy of Dr. Martin Luther King Jr.
Wellstar Health System honored the life, legacy, and many contributions of Dr. Martin Luther King Jr. with a tribute and virtual ceremony on Jan. 13. The event included team members, faith leaders, and powerful voices from the diversity, equity, and inclusion community with uplifting and moving blessings, song, dance, images and messages.
Wellstar physicians, caregivers, and team members are connected by the desire and commitment to serve with compassion, pursue excellence and honor every voice as the system strives to meet the vital needs of patients and communities.
During the virtual event, Wellstar president and CEO Candice L. Saunders reflected on the organization’s deep commitment to caring for people and Dr. King’s view of the world that all life is interrelated.
The ceremony’s keynote speaker, Dr. Johnetta Betsch Cole, chair and seventh president of the National Council of Negro Women and former president of Spelman College, an historically black college, emphasized the theme of the event from Dr. King’s “Letter from a Birmingham Jail,” wherein he stated: “Injustice anywhere is a threat to justice everywhere.” She talked about the importance of being an ally and advocate for any struggles against injustice, and encouraged all to build a better world where we can stand together. Dr. Cole was introduced by Le Joyce Naylor, Wellstar’s senior vice president and chief diversity, equity & inclusion officer.
In addition to inspiring messages from Dr. Cole and Saunders, the event included prayers and blessings from David A. Spencer Jr., manager of Wellstar Spiritual Health; Cavit Agu, chaplain for Wellstar Health System; Rabbi Judith Beiner of Jewish Family and Career Services of Atlanta; and Patricia Symonette, director of Wellstar Spiritual Health, who sang “Show Me How to Love,” by Babbie Mason. The Fellowship Bible Baptist Church Worship and Arts Ministry sang and danced to “Lift Every Voice and Sing,” by J. Rosamond Johnson and James Weldon Johnson. Dr. Scott Swayze, chair of the Wellstar Board of Trustees, closed the event with a message about Wellstar’s commitment to compassion, excellence, and inclusion.
Wellstar is honored to celebrate the life and legacy of American Civil Rights Movement leader and activist Dr. Martin Luther King Jr. and acknowledge this important federal holiday and National Day of Service in recognition of his enduring impact and example. Wellstar has added Martin Luther King Jr. Day to the paid holiday calendar starting Jan. 17, 2022.
5 Habits to Become the Healthiest You
Small changes add up to big results. By incorporating simple habits into your life, you can kickstart your wellness journey and stay on track for the long run.
Use the SMART goal-setting system to help define your goal and develop attainable resolutions.
Keep in mind, you may encounter some bumps in the road along the way. Recognizing all the small accomplishments can help you stay motivated and win in the long run.
“Focus on what small steps you’ve accomplished rather than how far you have to go,” Dr. Gomez shared. “Also, have a resiliency plan to help you bounce back after a more challenging day.”
Build new habits into your regular routine by beginning small and adding on over time. With this “habit stacking” technique, you pair your new habit with something you’re already doing. For example, if your goal is to drink more water, drink a glass of water while making your morning coffee or tea.
Seeing your primary care provider at least once a year is the single most important thing you can do for your health.
At your annual exam, your physician will help keep you healthy and reach your wellness goals. They screen for diseases to stay ahead of medical issues and check in on your overall well-being.
Set a reminder on your phone or calendar to prompt you to book an appointment. You can also use an important date, such as your birthday, anniversary or a holiday, as a marker to remind you to schedule a visit.
If you’re focused on improving your fitness routine, put a plan in place to be more active.
“Begin to incorporate a little more exercise into your daily routine,” said Wellstar Primary Care Physician Dr. Jeremy Boyd. “The Centers for Disease Control and Prevention offers a suggestion of 150 minutes of aerobic activity a week. I like to break that down to a good 40 minutes four times a week.”
Having a bedtime routine is essential to catch more Zs throughout the year. When you wake up feeling rested, you often feel more productive and energized throughout the day.
Get started by setting a specific time to go to sleep—and stick to it. Make sure you reserve at least seven to nine hours per night for sleep.
Limit your screen time before getting in bed. Bright screens from a phone, computer or TV can keep your brain awake and make it harder to fall asleep.
If you’re having trouble getting to sleep, have a decaffeinated cup of tea or take a warm bath to help you relax.
When it comes to losing weight, many people look for a quick fix, which can often create unhealthy ways of eating. Creating a healthy eating plan from the start can help avoid any fad diet pitfalls.
Nutrition plans that restrict or eliminate food groups and those with extreme calorie deficits are difficult to maintain and can often produce more weight gain or undesired results, according to Wellstar Registered Dietitian Kelly Prian.
Diet trends can also create a negative relationship with food, which can make it harder to achieve your goals. Prian shared that those with long-term success focus on maintaining a plan that enables steady weight loss over time.
A healthy nutrition plan is balanced and emphasizes whole foods, such as fruits and vegetables, lean proteins, low fat dairy, nuts and seeds, and whole grains.
Try not to overcomplicate healthy eating. You can start by filling half your plate with vegetables or having fun trying new recipes.
Self-care is an important aspect of your mental well-being and should be made a consistent part of each day.
“Make self-care a priority and a non-negotiable,” Dr. Gomez said.
“Think of self-care as a form of personal healing and a way to strengthen resilience,” Dr. Gomez explained. “Much like the way exercise enhances physical health, self-care enhances mental health.”
According to Dr. Gomez, it can be helpful to turn tasks we do on “autopilot” into more meaningful experiences.
“When washing your hands, give yourself a hand massage,” Dr. Gomez shared. “When driving, use red lights to practice deep breathing. Listen to a book on tape or language lessons rather than the radio or call someone to reconnect.”
If you feel overwhelmed by stress or anxiety, Wellstar behavioral health specialists are here for you.
“Working with a mental health provider is different than speaking with a friend or even a life coach,” Dr. Gomez said. “Mental health professionals are trained and licensed to address psychological or emotional wellness.”
Need support? Connect with a Wellstar behavioral health specialist.

Know Where to Go for COVID-19 Care
With the spread of the highly contagious Omicron variant of COVID-19, our communities are seeing a surge in cases of the virus, as well as a higher demand for testing.
Wellstar, along with other Georgia health systems, has experienced high volumes at our facilities, particularly in emergency departments. Our dedicated care team continues to work hard to keep our community healthy, and our facilities will continue to provide life-saving care, including in emergencies when those we serve need us most.
However, to keep emergency care available to those with critical health needs, people should seek care at the facility most appropriate for their condition.
If you are experiencing symptoms of COVID-19, you have several choices for testing and care. If you test positive, isolate from others, monitor your symptoms and contact your primary care provider to discuss treatment options.
If you are asymptomatic but have a known or possible COVID-19 exposure, you can seek testing at an urgent care, primary care office or other testing site.
While Wellstar offers rapid and PCR testing at all of our urgent care centers, those locations are experiencing longer wait times due to high demand. Find a testing site near you on the Georgia Department of Public Health website.
Get tested if you have mild or moderate symptoms. If you test positive, your provider can help you determine the best course of treatment.
If your symptoms escalate and become more severe, go to an emergency department.
If you experience severe symptoms, immediately seek care at your nearest emergency department or call 911.
The Centers for Disease Control and Prevention recommends you seek emergency care if you experience any of the following symptoms:
Even in a pandemic, it is important to not delay care for life-threatening emergencies, whether you have COVID-19 or are experiencing another health emergency like a stroke or heart attack. Our emergency care experts are here to care for you and your family in critical situations when you need us most.
Your Mask Matters
After nearly two years in the COVID-19 pandemic, wearing a face mask may be second nature to many of us. However, as the highly contagious Omicron variant spreads, it’s important to know single-layer cloth masks offer minimal protection.
Wellstar Health System has recently updated its mask policy when visiting our facilities, and recommends people follow these guidelines to stay safe.
For more safety tips and resources, visit Wellstar’s COVID-19 resource page.
Metro Atlanta Health Care Systems Address Public on COVID-19
Six major health systems that serve metro Atlanta and the state of Georgia have unified to address the public regarding the latest COVID-19 impacts and the result of the rapid spread of the Delta and Omicron variants.
Children’s Healthcare of Atlanta, Emory Healthcare, Grady Health System, Northeast Georgia Health System, Piedmont Healthcare and Wellstar Health System are once again experiencing a staggering surge in adults and children with COVID-19 symptoms and diagnoses. Collectively, the healthcare systems have experienced 100–200% increases in COVID-19 hospitalizations in the past eight days and the vast majority of inpatients are unvaccinated. This comes at a time when the health systems are preparing for an influx of patients with seasonal flu.
Emergency room activity has also increased significantly for both emergent and non-emergent situations, including those seeking COVID-19 testing without the need for further care or treatment. To keep emergency rooms available to individuals who have the most critical health needs, individuals should obtain care at the most appropriate medical facility for their condition and seek COVID-19 testing at primary care locations, public health and mass testing sites or use at-home testing kits.
While hospitals in metro Atlanta and throughout Georgia have best practices in place to actively manage capacity and provide high-quality patient care, we need the public’s help and support. Doing the following will help us all navigate this significant wave, minimize serious illness and hospitalizations from COVID, and better manage emergency room diversions and wait times at our facilities:
The health and safety of our patients and communities remains our top priority. The six metro Atlanta health care systems will continue to work together to educate and inform the public regarding COVID-19 and address the most critical health needs impacting our area. We also would like to express our appreciation to the Governor for his support of our workforce and the newly announced funding to address staffing shortages at hospitals across the state due to COVID-19, and to the Georgia Department of Public Health for continued outreach to the public regarding issues affecting our patients, care team members and community.

Here’s to a Healthy You in ‘22
With the holiday season now behind us, people look forward to the fresh start of the New Year and all the possibilities it brings. For many of us, that means setting resolutions to live a healthy, full life.
Without the proper planning and support, however, these ambitions can quickly be put off or even forgotten. In 2022, it’s time to break the cycle and make progress towards your goals.
By following tips from Wellstar health experts, you can create realistic resolutions, better your health and stay motivated.

Tracking Prostate Cancer in High Definition with PSMA Imaging
Wellstar patients were among the first in Georgia to benefit from an FDA-approved imaging technology that detects the extent of prostate cancer earlier and with greater accuracy than current imaging methods.
A diagnostic agent is given to patients as an injection. Once it is in the body, it binds to PSMA, or Prostate Specific Membrane Antigens. Prostate cancer cells usually have a higher level of PSMA.
When used with PET scans, this innovative technology gives physicians a clearer image of prostate cancer lesions and enables providers to determine the best course of treatment. It is the most sensitive scan available for prostate cancer.
Wellstar is among the first in Georgia to routinely offer PSMA PET scans.
While standard scans have limited sensitivity for prostate cancer, this advanced imaging is much more capable of identifying prostate cancer, which allows Wellstar doctors to determine if the cancer is limited to the prostate or if it has spread to other parts of the body.
“It allows us to make sure we’re not missing any sites of cancer that aren’t picked up with old-school imaging,” Wellstar Urologist Dr. Justin Watson said. “If there is an area of cancer outside what we’d typically treat, and we pick it up with this imaging, we can make sure we address that area, too.”
Providers can then tailor treatment to each patient’s individual needs, collaborating with the patient to find the best course of action and improve outcomes.
“This imaging helps us ensure that patients are receiving the right treatment, which improves their outcomes,” Dr. Watson said.
The new imaging technology improves upon scans that were used in the past.
“This is several leaps forward in our ability to see prostate cancer on a scan in high resolution,” Dr. Watson said. “In the older scans, things are difficult to see and sometimes not even perceptible, and with the new scans, they light right up and we know much better what we’re dealing with.”
This PSMA imaging is currently available at Wellstar Kennestone Regional Medical Center and Wellstar Cobb Medical Center, with plans to expand to other locations.
Wellstar urologists, oncologists, radiation oncologists, pathologists and radiologists work collaboratively to provide prostate cancer patients a full range of treatments to consider including active surveillance, CyberKnife/radiation therapy, surgery, hormone therapy and chemotherapy.
To learn more about prostate cancer treatment at Wellstar, visit wellstar.org/prostatecancer or call 1 (877) 366-6032.

Maintain Your Mental Health During the Holidays
If you find the holiday season overwhelming, you’re not alone.
Wellstar experts say many people may have strong emotions at this time of year, especially since the start of the COVID-19 outbreak.
"For many people, COVID-19 was a catalyst for alienation and isolation – further magnified at times by the loss of friends and family members," said Dr. Ryan Breshears, chief behavioral health officer with Wellstar Health System. "The research is unequivocal – loneliness is a driver of morbidity and mortality. Whereas feelings of grief are normal and understandable following loss, during the holiday season, it is imperative that we connect back to meaning, purpose and relationships. Prioritizing that human connection with others can, in essence, be a life-saving measure."
Difficult emotions may be unwelcome visitors this time of year, but you can take steps to help yourself feel better.
Looking for more ways to stay well? Learn how to give yourself the gift of health and partner with a Wellstar primary care provider.

Wellstar Kennestone Hospital Begins Planned Construction and Expansion Project
Wellstar Health System, one of the largest and most integrated healthcare systems in Georgia, is announcing that the planned construction and expansion project to further enhance patient services and facilities will begin at Wellstar Kennestone Hospital on December 20, 2021. During construction, the Church Street entrance to Wellstar Kennestone Hospital will be closed.

WHEN: Starting December 20, the covered walkway from the hospital’s Blue Parking Deck to the main entrance will be replaced with a temporary covered sidewalk, shifting the Labor & Delivery Entrance and Drop-Off to inside the Blue Parking Deck at the existing Kennestone Outpatient Pavilion (699 Building) entrance. To access the Labor & Delivery entrance, visitors will need to use Kennestone Hospital Boulevard, off Tower Road, then follow the signs into the covered Blue Parking Deck.
Wellstar Kennestone Hospital is taking the following steps to minimize the impact on patients, team members, providers, and the community:
WHY: Wellstar Kennestone Hospital is prepping the site for the proposed expansion project and new patient tower. Wellstar is developing the new tower to expand its women and children services, enhance campus amenities, and address community requests for more private rooms. The new tower will replace the current Baird Building and is expected to open in mid-2025.
To see the latest updates on the project, visit the Wellstar Kennestone Hospital web page.
Innovation is Buzzing at Wellstar Vinings Health Park
Through a new partnership, Wellstar will both help address food insecurity in the communities we serve and have a positive impact on our environment.
Honeybees are an essential part of our ecosystem, and they keep us fed — bees pollinate 70 of the world’s top 100 crops. However, they are dying at high rates as they lose their habitats. Wellstar is taking a step to help by giving a home to three beehives at Wellstar Vinings Health Park in a partnership with Bee Downtown. Wellstar is the first hospital system to partner with Bee Downtown on such an initiative.
These small insects make a huge impact. A single honeybee creates more than 1,200 pollination events each day, so the bees at Wellstar will make billions of pollination events a year. Wellstar’s bees will also produce 80 pounds of honey a year. Some of that honey will be donated to Open Hand Atlanta, which provides home-delivered meals to those experiencing food insecurity and will include honey from Wellstar in its “Market Baskets” of groceries donated to community members in need.
The safety of our patients, community and team members is Wellstar’s highest priority. The bees will be kept in a gated area behind the health park, away from sidewalks and building entrances.
The partnership with Bee Downtown is an initiative of Catalyst by Wellstar, a global digital health and innovation center working to transform healthcare. To learn more, please visit catalyst.wellstar.org.
Innovation is Buzzing at Wellstar Vinings Health Park
Through a new partnership, Wellstar will both help address food insecurity in the communities we serve and have a positive impact on our environment.
Honeybees are an essential part of our ecosystem, and they keep us fed — bees pollinate 70 of the world’s top 100 crops. However, they are dying at high rates as they lose their habitats. Wellstar is taking a step to help by giving a home to three beehives at Wellstar Vinings Health Park in a partnership with Bee Downtown. Wellstar is the first hospital system to partner with Bee Downtown on such an initiative.
These small insects make a huge impact. A single honeybee creates more than 1,200 pollination events each day, so the bees at Wellstar will make billions of pollination events a year. Wellstar’s bees will also produce 80 pounds of honey a year. Some of that honey will be donated to Open Hand Atlanta, which provides home-delivered meals to those experiencing food insecurity and will include honey from Wellstar in its “Market Baskets” of groceries donated to community members in need.
The safety of our patients, community and team members is Wellstar’s highest priority. The bees will be kept in a gated area behind the health park, away from sidewalks and building entrances.
The partnership with Bee Downtown is an initiative of Catalyst by Wellstar, a global digital health and innovation center working to transform healthcare. To learn more, please visit catalyst.wellstar.org.

Preventing & Curing Diabetic Ulcers with Wellstar Wound Care
When someone is diabetic, a small wound can escalate into a major health issue and, in many cases, lead to an amputation. However, with proper wound care and accelerated healing with hyperbaric medicine, Wellstar patients are partnering with providers to treat wounds like diabetic foot ulcers.
Diabetic foot ulcers can develop if diabetes is not well-managed, and some causes of ulcers include poor circulation and high blood sugar. Ulcers may go unnoticed at first because many people with diabetes are also affected by neuropathy and do not have feeling in their feet, said Dr. Ricardo Duran, Medical Director of the Wound Care and Hyperbaric Medicine Department at Wellstar North Fulton Hospital.
Also, if a diabetic person gets a wound, it may not heal as quickly, as people with diabetes are more likely to also experience poor circulation, immune system deficiencies and elevated blood sugar levels.
“When you combine the lack of sensation in the foot with the lack of healing, that leads to even more damage,” Dr. Duran said.
Foot ulcers should be taken seriously — when a diabetic person has an open wound, their five-year mortality rate increases by about 32%, according to Dr. Duran.
When Venson Rolle developed a foot ulcer, he knew he needed to seek care. In Dr. Duran, he found a healthcare partner dedicated to preventing amputation and keeping him healthy. “Dr. Duran was very patient, and he was ready and willing to do anything possible for me to get the correct treatment to heal all the way,” Venson said.
Dr. Duran helped Venson’s ulcer heal by off-loading the foot with orthotics to prevent further injury, treating him with antibiotics and using hyperbaric oxygen therapy.
A hyperbaric oxygen chamber allows the lungs to get more oxygen. That oxygen then flows through the body, promoting wound healing. It helps repair tissues and treat infections.
“It provides oxygen at high pressure and keeps the tissues alive while the antibiotics work to guarantee that we have a better outcome,” Dr. Duran said about the procedure.
Venson, whose ulcer has healed, said he is grateful that the treatment has improved his quality of life.
“I can’t thank him enough,” Venson said about Dr. Duran.
Dr. Duran recommends that people with diabetes work with their primary care provider to manage diabetes and monitor their A1C.
People with diabetes should also check their feet every day, looking on the bottoms of the feet and in between the toes for any signs of wounds or ulcers, Dr. Duran said.
“They should not rely on how it feels, because the sensation is abnormal and they might not feel an ulcer,” Dr. Duran said.
Dr. Duran said people with diabetes should also avoid smoking and eat a diet low in carbohydrates and high in protein to help prevent ulcers.
The Wound Care & Hyperbaric Center at Wellstar North Fulton Hospital doesn’t just treat diabetic ulcers — patients can also find treatment for traumatic injuries, burns, pressure ulcers and other wounds. To make an appointment, call (770) 751-2830.
Wellstar’s Center for Best Health Opens New Office in North Fulton
Patients in North Fulton who need weight management assistance have a new option, with providers who will support them at every step of their journey.
Wellstar's Center for Best Health now has an office in North Fulton, conveniently located at 1360 Upper Hembree Road, just across the street from Wellstar North Fulton Hospital and inside the primary care practice of Dr. Nandini Sunkireddy and Dr. Amy Barfield.
Dr. Sunkireddy is the physician overseeing this Center for Best Health location, and she is welcoming new patients to both primary care and the Center for Best Health.
The Center for Best Health offers a comprehensive approach to weight management and includes behavioral health, nutritional therapy and dietician services, medication management, meal replacement through Optifast and exercise management. When bariatric surgery is an appropriate option, our providers will offer referrals.
Our providers tailor care to each patient’s individual needs and lifestyle, creating the right treatment plan to help each person achieve their optimal health. The interdisciplinary care team includes a physician, dietitian, exercise physiologist and psychologist.
“We support you as a team in every step of your weight loss journey until you reach your goal,” Dr. Sunkireddy said. “We all support your efforts to keep the weight off by helping you develop a healthy lifestyle.”
The Center is for people whose A1C is equal to or greater than 6.5, indicating diabetes, or those who have a BMI equal to or greater than 30 with another chronic health condition such as high blood pressure.
DominiqueCare
As a Hall of Fame basketball star, Dominique Wilkins knows what it takes to stay on top of his game. He’s even nicknamed “The Human Highlight Film” for his legendary slam dunks and athletic ability on the court.
Performing at such a high level, he felt invincible. But after receiving a type 2 diabetes diagnosis at age 40, Dominique was caught completely off-guard.
Turns out, even the pros are at risk for chronic conditions.
“When I was diagnosed with diabetes a year after I retired, it was frightening because both my father and grandfather passed away from type 1 diabetes,” he shared. “It quickly changed my life.”
Dominique didn’t let the news stop him from taking charge of his health. He turned his diagnosis into determination.
Dominique has focused on becoming the healthiest version of himself by eating right, exercising regularly and taking medication.
Ever since teaming up with Wellstar, his rebound has been doubly impressive. Here, he’s found expert care and support to help him live a full, healthy life.
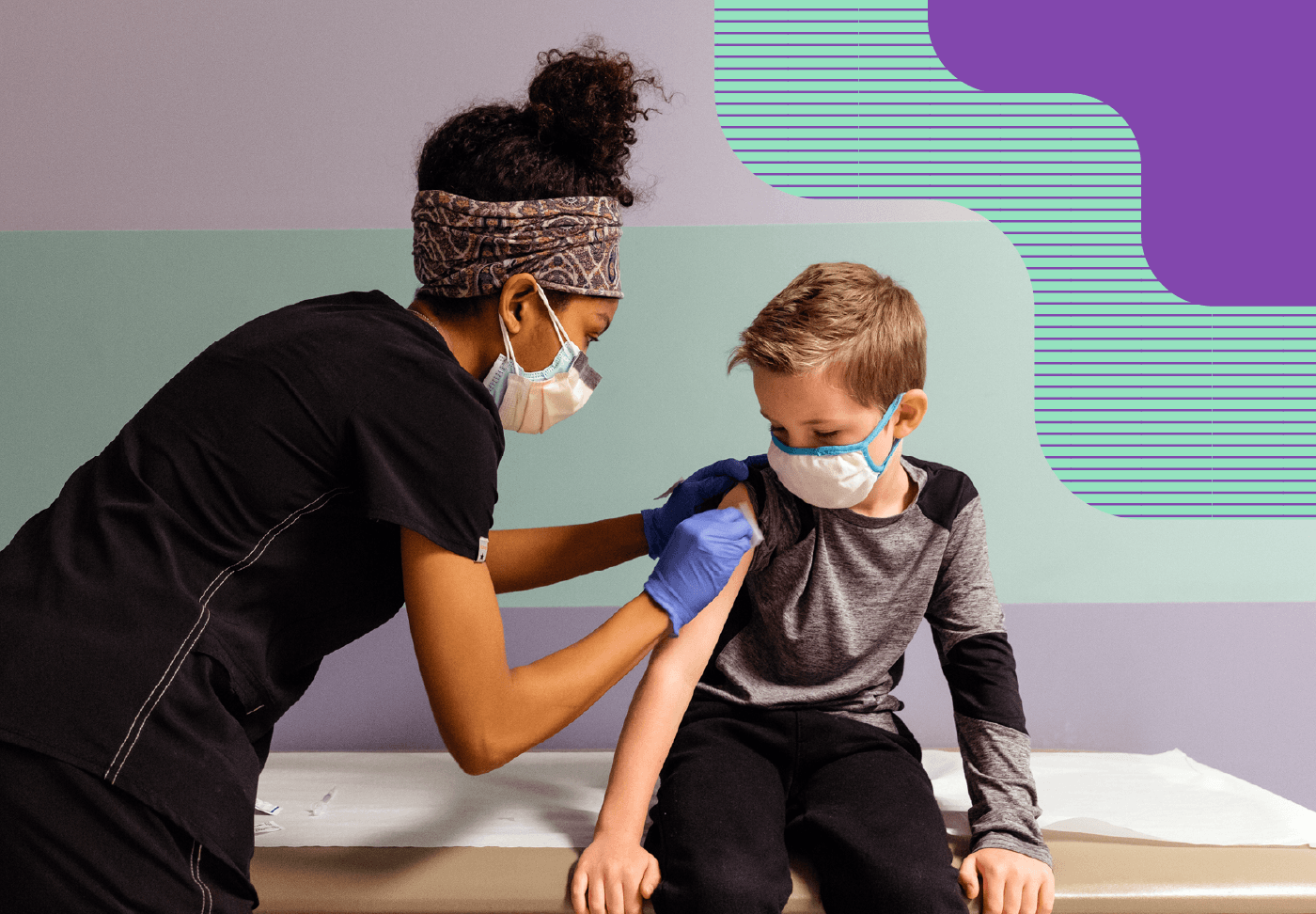
Wellstar Health System Opens Pediatric COVID-19 Vaccination Clinics to Enthusiastic Community Response
Wellstar Health System has opened two pediatric COVID-19 vaccination centers following the United States Food and Drug Administration’s (FDA) Emergency Use Authorization (EUA) of the COVID vaccine for existing Wellstar pediatric patients aged 5 to 11. Wellstar began offering COVID vaccinations for children under age 12 the weekend of Nov. 5 and quickly filled more than 100 vaccination appointments on the first day. To date, nearly 2,000 appointments have been scheduled through January 2022. The Wellstar pediatric COVID vaccination sites are currently located at the East Cobb and Acworth Health Parks, and parents and caregivers are encouraged to schedule a vaccination appointment with their children’s pediatrician.
“During the COVID pandemic, Wellstar has remained dedicated to protecting our practitioners, patients, and the children of our communities,” said Dr. Avril Beckford, chief pediatric officer for Wellstar Health System. “We are incredibly excited by the high demand and interest in pediatric vaccinations and proud of the families who have taken the important step to vaccinate their children to offer some of our youngest patients protection against COVID.”
Wellstar’s COVID pediatric vaccination clinics include waiting rooms for families to relax in while their children are vaccinated. In addition, parents can also schedule follow-up visits, including the second vaccine dose and other important immunizations while waiting.
“I decided to get my two children ages five and seven vaccinated,” said Hunter Carlson, executive director of Health Parks and Pediatric Center for Wellstar Health System. “The kids had a great time and enjoyed interacting with the physicians and staff. In addition to wearing masks, the vaccine will give my children and family an extra layer of protection against the disease.”
The best protection against COVID-19 is prevention, vaccination and stopping community spread. Be sure you and your family members who are age five and up get the COVID-19 vaccine. Parents can also help protect their children’s health by teaching them the 3Ws—wear a mask, wash your hands and watch your distance.
For more health tips and information on how to schedule pediatric vaccinations, visit our Pediatric Care During COVID-19 page.
Reimagining the Future of Care
Hank Capps, MD, Wellstar Health System’s Chief Information and Digital Officer, recently delivered a keynote address about the future of care at the 2021 Healthcare Internet Conference in Las Vegas. This article summarizes Dr. Capps’ remarks regarding how the future of care is taking shape and how digital technology can be leveraged to achieve better patient outcomes and community health.
Never in our recent history has society gone through a period where technological innovation is moving more rapidly than it is right now, while impacting every aspect of our daily lives in the process.

‘Tis the Time for T.H.A.N.K.S. Again
Dr. Danny Branstetter
Another year has come and gone, and while COVID-19 is still with us, this year brings gratitude for one of the best ways to protect against the disease – vaccinations. While safety measures are still encouraged, family gatherings are a bit safer this year due to the safety and efficacy of the vaccines rolled out late last year. COVID vaccines are now available for people who are at least five years old and offer important protection for families, friends, and communities as they gather for the holiday season.
Wellstar Health System has provided the healthy and helpful tips below to help families safely enjoy the winter holidays and give T.H.A.N.K.S. again:
T - TAKE STEPS EARLY: Preventing the spread of COVID during the holidays is more than just wearing a mask, watching your distance, and washing your hands. It’s about caring for those you love by taking steps to be sure you keep everyone safe. The best way to do that is to get vaccinated.
H - HAVE FAMILY PLANS: No matter how you celebrate the winter holidays, COVID can easily throw a wrench into any occasion. Having a family plan to prevent catching or spreading the disease can keep unneeded worry out of holiday gatherings.
A – AWARENESS: Stay aware of the latest COVID-19 news and information by checking updates from credible sources such as the CDC and local public health departments.
N - NEW TREATMENTS ARE HERE: The holidays are a time to gather with loved ones and give thanks. Many new medical advances have been approved that help treat COVID and limit the severity of the disease. That is reason to be thankful!
K - KEEP CALM AND BE KIND: The past two years have been challenging, and many are finding new ways to cope with unexpected loss. Please be considerate and kind and try to remain calm when faced with anxieties about the pandemic.
S -SUPPORT OTHERS: Support those interested in learning more about COVID vaccines by sharing information from credible sources such as the CDC. The spread of misinformation can negatively affect COVID-19 vaccine confidence and because we know how truly effective the vaccines have been in our communities, let’s all work together to focus on the facts from healthcare experts.
Wellstar is committed to providing world-class healthcare during the COVID-19 pandemic. Click here for more information and tips on how to prevent COVID.

Wellstar Kennestone Hospital Celebrates 5-Year ECMO Anniversary
For a half decade and counting, Wellstar Kennestone Hospital has used an advanced treatment called extracorporeal membrane oxygenation (ECMO) to provide vital oxygen supply to people when it matters the most.
For the dedicated team members at Wellstar Kennestone Hospital, their five-year ECMO anniversary marks more than a milestone. It means saving more lives.
ECMO is a cutting-edge technology that has been vital in treating critically ill people — like Zac DiGiorgio — whose lungs are in peril and unable to function on their own.
Dr. Asif Saberi, Wellstar medical director of critical care & ECMO, shared how this state-of-the-art therapy works.
“ECMO is a way to provide air to the body when the lungs fail completely,” Dr. Saberi said. The innovative therapy helps removes carbon dioxide from the bloodstream using a machine when the lungs cannot on their own.
“During ECMO, blood is diverted from the body using plastic catheters — called cannulae — which are approximately the size of a garden hose,” Dr. Saberi explained.
“When the blood is redirected from the body, it is ‘cleaned’ of carbon dioxide which the lungs would have done naturally,” Dr. Saberi said.
After that, the re-oxygenated blood is recirculated through the system to supply life-saving oxygen to the body.
People who suffer traumatic injuries are not the only ones benefitting from the high-tech treatment. Since the start of the COVID-19 pandemic, ECMO has also become instrumental in the fight against the virus.
Recently, ECMO has been key in caring for COVID-19 patients with the most severe symptoms.
COVID-19 is a respiratory virus, and can affect the lungs and a person’s ability to breathe normally. In fact, the American Lung Association reported that the lungs are the first organ affected by the virus.
Symptoms like shortness of breath and difficulty breathing may appear suddenly and be severe. For the most critical cases, expanding access to ECMO can be a gamechanger.
“Our ability to provide one specific therapy, ECMO, for a significant number of young people in the extreme manifestation of the disease, is possibly the difference between life and death,” Dr. Saberi shared.
By offering ECMO right here in Georgia, Wellstar Kennestone Hospital is helping to save lives and fight back against the virus. And, for us, five years is only the beginning.
To learn more about how our team is providing world-class care for the community, visit the Wellstar Kennestone Hospital page.

Break Free from Uterine Fibroid Pain
If you’re a woman suffering from pain or discomfort due to uterine fibroids, you’re not alone. An estimated 26 million women in the U.S. have uterine fibroids — and more than 15 million will experience symptoms or health concerns.
Uterine fibroids are common, non-cancerous growths in the uterus, affecting 20 to 80% of women by age 50. Often, these benign tumors are small and do not cause issues.
However, for some women, the growths can lead to painful symptoms, including:
While all women can develop uterine fibroids, Black women are disproportionately affected. Black women often have fibroids at younger ages, larger growths and more severe symptoms compared to other racial groups.
Pain doesn’t have to be part of life. Women experiencing fibroid pain can find expert care, advanced treatments and support at Wellstar Windy Hill Hospital.
Wellstar Windy Hill Hospital provides a minimally-invasive treatment called uterine fibroid embolization (UFE), which can help improve symptoms and quality of life. While fibroids can also be treated with surgical options like a hysterectomy, UFE offers a non-surgical solution that preserves the uterus.
During this procedure, an interventional radiologist inserts sand-like particles into the artery that supplies the fibroid, blocking its blood supply. This method prevents estrogen and other nutrients from reaching the tumor, which can cause the fibroid to shrink up to 50%.
Wellstar Windy Hill Hospital’s trained imaging team performs UFE every day, offering a wealth of expertise and experience. Providing high-quality, comprehensive fibroid care close to home can make all the difference for people with fibroid pain.
“UFE offers many women a minimally-invasive solution to treat fibroid symptoms,” said Dr. Jordan Ray, interventional radiologist with Quantum Radiology, who works with the imaging team at Wellstar Windy Hill Hospital. “When this uterine preservation therapy is compared with other treatment options, patients recover faster and experience better outcomes without the need for surgery.”
In addition to a quicker recovery time and fewer complications, women who choose UFE at Wellstar also benefit from Wellstar Fibroid Care Coordinators.
Wellstar Fibroid Care Coordinators help the process go smoothly for patients, including scheduling appointments, obtaining insurance verification and coordinating referrals. One-on-one care is provided at every step, from pre-op to surgery and through recovery.
With complete fibroid care and a supportive team at Wellstar Windy Hill Hospital, women can get back to living pain-free.
For more information and to find out if UFE is the right treatment for you, call (770) 644-1636.

World-Class Resources, Personalized Care: West Georgia Cancer Treatment
Patients in West Georgia don’t need to drive to Atlanta for life-saving cancer care. The Enoch Callaway Cancer Center keeps quality care close to home and combines the resources of a large facility with the personalized, compassionate feel of a smaller location.
“One of my missions is to bring great cancer care to people close to where they live, so they can access that care much more easily,” said Wellstar Radiation Oncologist Dr. Robert Taylor. “To have Wellstar backing this world-class treatment, building this new cancer center and this fantastic team that we have, is absolutely stellar.”
At the Enoch Callaway Cancer Center at Wellstar West Georgia Medical Center, patients will find the latest in technology and clinical trials, paired with expert providers who care for both their physical and mental well-being.
Cutting-edge technology at the Cancer Center allows providers to target tumors using X-ray technology, keeping the journey to living cancer-free painless for patients.
Stereotactic ablative radiotherapy takes about 30 minutes per treatment, with some patients requiring multiple treatments and others only needing one. It is most effective in early stage brain or lung cancer and can also be used to treat metastatic cancer.
“We’re able to use X-rays to very precisely target a tumor and literally kill that tumor inside there without the patient undergoing any surgery,” Dr. Taylor said. “Despite the name, there’s no cutting involved, and there’s no anesthesia involved.”
The patient lies on a table for the treatment, and “at the end of that 30 minutes, they will get up off that treatment table and walk out of the facility feeling the same as they did when they came in,” Dr. Taylor said.
“It’s absolutely miraculous to see people get off the table and know their brain tumor has been cured or their lung cancer has been cured,” Dr. Taylor said.
Protect Your Lung Health During the COVID-19 Pandemic
Prevention plays a clear role in keeping your lungs healthy and, since the start of the COVID-19 pandemic, that has never been more true.
COVID-19 is a respiratory virus that can affect the lungs, which may impact your ability to breathe normally and, in some cases, even cause lasting breathing problems after recovery.
“Infections like COVID-19 come predominantly through the airways,” said Wellstar Pulmonologist Dr. Hitendra Patel, explaining how the virus often enters the body.
Within the first days of infection, COVID-19 starts attacking cells in the respiratory system. In fact, the American Lung Association reported that the lungs are the first organ affected by the virus.
Being infected with COVID-19 can lead to shortness of breath, difficulty breathing and cough — symptoms which can appear suddenly and be severe.
“It’s important people do everything in their power to protect their lung health,” Dr. Patel urged. “This is especially true during the COVID-19 pandemic and as variants emerge.”
While the world continues to work together to control COVID-19, there are ways you can be proactive and protect your lungs.

Wellstar Paulding Hospital Designated a Level IV Trauma Center
When kids or adults are injured, a specialized trauma team is ready 24/7 in Paulding County to provide high-quality patient care. As a result of its commitment to advanced trauma care, Wellstar Paulding Hospital was recently designated a Level IV Trauma Center by the Georgia Department of Public Health (DPH). Level IV Trauma Centers demonstrate the ability to provide advanced trauma life support prior to transfer of patients to a higher-level trauma center when necessary.
“Wellstar Paulding Hospital is part of the largest trauma network in the state, delivering compassionate, high-quality care to people in our community suffering from accidents, incidents and injuries,” said Frances Van Beek, assistant vice president of Trauma & Neuro Services for Wellstar Health System. “Patients benefit from our team’s tight-knit communication and collaboration, as well as our physician and caregiver expertise that enables us to save lives every day.”

Babies, kids and teens now have their own emergency department at Wellstar Douglas Hospital
For a child, going to the hospital can be scary. That’s why Wellstar Douglas Hospital’s new $5.7 million Pediatric Emergency Department (ED) offers a kid-friendly and kid-sized experience for Douglas County’s youngest patients. The nautical-themed 7,600 square-foot facility provides specialized care for children from birth to 18 years of age.
The world-class “just-for-kids” facility has a separate entrance and waiting room from the main Emergency Department and is currently open from 11 a.m. to 11 p.m. The ten treatment rooms feature child-sized furniture, equipment and supplies.
“We created an environment that is optimum for healing and that helps our youngest patients feel as comfortable as possible,” said Dr. Avril Beckford, chief pediatric officer, Wellstar Health System. “Children in Douglas deserve to see doctors and nurses who understand them. We also wanted to give parents a state-of-the-art facility staffed by pediatric physicians close to home – there is no need to travel long distances with a sick child now, because this specialized facility is right here, in the Douglas County community.”
Staffed by kid-friendly nurses and skilled providers devoted to children, the new kids’ ED is a result of collaboration between the architect, construction firm and pediatric experts. Wellstar’s pediatric team cares for children at more than 114,000 emergency visits a year across Wellstar’s hospitals.
“From the outside, there are colorful floor-to-ceiling glass windows,” Dr. Beckford said, as she imagined a child’s first impression. “It feels almost like you’re walking into an aquarium.”
Inside the pediatric ED, children and their parents are greeted by warm staff members, soothing murals of ocean life, a large flat screen TV and child-sized furnishings.
To help children be seen and treated more quickly, some rooms will be dedicated to patients with less serious conditions – such as sore throats and sprains. There will also be a trauma bay and a dedicated room for adolescent gynecological concerns.

Wellstar Clinical Partners Medicare ACO Significantly Reduces Cost for Patients
The Centers for Medicare & Medicaid Services (CMS) announced the 2020 results for the Medicare Shared Savings Program (MSSP) and Wellstar Clinical Partners (WCP) Medicare Accountable Care Organization (ACO) helped CMS save over $18 million for the entire performance year. During the 2020 calendar year, WCP Medicare ACO also received its highest quality score and yielded the third-best financial performance, resulting in cost savings for patients.
“Even through the most challenging times such as the current COVID-19 pandemic, Wellstar has remained dedicated to providing high-quality, world-class care for our patients,” said Dr. John Brennan, executive vice president and chief clinical integration officer of Wellstar Health System. Dr. Joseph Havlik, chairman of the board for WCP added, “While we continue to work together to keep our communities safe, we’re all proud that we have been able to remain focused on excellent quality, appropriate cost, exceptional patient experience and caregiver well-being.”
Wellstar achieved a quality score of 97%, a metric that rates ACOs on patient experience, patient safety, preventive health and at-risk populations. The WCP Medicare ACO performed in the top 15 percent of ACOs for 2020 based on generated savings, out of more than 500 other ACOs.
“Our physicians and partners are passionate about the health and well-being of our patients,” said Barbara Corey, senior vice president of Managed Care for Wellstar Health System. “The scores and accomplishments for the 2020 calendar year are a true testament to our commitment to providing compassionate and exceptional care.”
One of the largest and most experienced ACOs in Georgia, the WCP Medicare ACO is consistently named one of the top ACOs in the country. Additionally, the ACO is the only one in Georgia to help Medicare bend the healthcare cost curve for seven of the last eight years. Medicare Shared Savings Program (MSSP) ACOs are groups of doctors, hospitals, and other healthcare providers who come together voluntarily to provide coordinated high-quality care to their Medicare patients.
The WCP Medicare ACO leverages its internal resources, infrastructure, and partnerships with employed and affiliated physicians to deliver high quality, cost-effective healthcare to the communities it serves. Since 2012, the WCP Medicare ACO has been a consistent, high-quality, top performing ACO and it is among the top MSSP ACOs when measured by cumulative savings to Medicare of over $111 million.

BreathofFreshAirCare
Whether you’re running a marathon or simply running errands, having healthy lungs helps you to live comfortably and do the activities you enjoy.
Lung health is an important part of overall wellness. It’s best to prevent health issues before they start, and Wellstar experts will partner with you to personalize a plan to keep your lungs healthy.
Book an appointment online to check in with a provider about your lung health and follow these tips to breathe a little easier.
If you are a smoker, keep in mind that there are both short-term and long-term benefits to quitting. One to nine months after the last cigarette, your shortness of breath should decrease. Within 10 years of quitting, a former smoker's risk of developing lung cancer is 30% to 50% below that of a person who continues to smoke.
Also, if you don’t smoke, do not pick up the habit. Nicotine is highly addictive, even more so than many other drugs including narcotic opiates, according to Wellstar Pulmonologist Dr. Hitendra Patel.
Dr. Patel said that vaping is gaining popularity, especially among younger people. However, vaping irritates a person’s airways and increases their risk of asthma.
“Nothing but air should go in and out of the lungs,” Dr. Patel said. “Any other chemical or substance, or inhalation of smoke of any kind, is going to be detrimental and harmful.”
Wellstar Primary Care Physician Dr. Jignesh Dholaria said misinformation about vaping is common.
“People have the notion that vaping is somehow safer and that it doesn’t have the same chemicals that cigarettes do,” Dr. Dholaria said. “We’re seeing a lot more harmful effects from vaping just because we don’t always know all the chemicals that are in these vapes. That has caused a lot more lung-related injuries.”
While staying active is a critical component of overall wellness, it’s especially important to keep your lungs in top shape.
“As you’re breathing in and out, getting rid of carbon dioxide and inhaling more oxygen, that helps your tissues, which helps you feel better overall,” Dr. Dholaria said.
Even if it is raining—or if pollutants are especially high that day and you’re worried about lung irritation—there are ways to get your steps in. Dr. Patel recommends going to an air-conditioned shopping mall or store to get some exercise if being outside is not an option.
“Continuing to exercise to the fullest of your body’s ability is an important step of maintaining whatever lung health you have,” Dr. Patel said. “If you start with healthy lungs, staying on an exercise program and regimen is vital.”
Balance that exercise with some rest, too. Dr. Patel, who is also the medical director of the Wellstar sleep program, said being well-rested can ward off sickness, including some respiratory illnesses.
“If you don’t sleep well, that means your immune system is not going to function as well as it should,” he said.
In addition to getting your sleep, some relaxation and breathing techniques can have benefits for both mental wellness and lung health.
Dr. Patel recommends “4-7-8 breathing,” which involves inhaling for four seconds, holding your breath for seven seconds and then exhaling for eight seconds.
Benefits of breathing exercises may include lower stress and anxiety levels, lower blood pressure and better sleep.
If you have asthma, know your lungs and avoid the environmental triggers that cause the condition to flare up, Dr. Patel said. Common triggers include pet dander, seasonal changes, allergens like perfume and smoke inhalation.
Asthma can also run in families, although there is often no specific reason why a person develops asthma, Dr. Patel said.
“Sometimes people underestimate how bad asthma can be,” Dr. Patel said.
If you have asthma, see your primary care physician to monitor your lung health. Pulmonologists specialize in caring for people’s lungs, and they often collaborate with primary care providers to create personalized plans to manage their patients’ asthma.
Early detection is key in cancer treatment, but many lung cancers present in later stages, Dr. Patel said.
“In that area in the middle of the lungs and the middle of the chest, there are no pain fibers or pain sensors in there,” Dr. Patel said. “If a tumor occurs there, patients don’t know it. They don’t feel it, and it doesn’t hurt them.”
Lung cancer is sometimes found when it spreads and causes complications, Dr. Patel said.
If you are at increased risk for developing lung cancer, ask your provider about screenings. You should consider screenings if you are a current or past smoker. Visit our lung cancer screening page to learn more about if screening, which involves low-dose CT scans, could benefit you. To keep up with your lung health, find a Wellstar physician near you.
Día de los Muertos 2021: A time to honor and safely celebrate
Día de los Muertos, or Day of the Dead, is a festive, multi-day cultural celebration among Mexican and Latinx communities where family and friends come together to pay respects to friends and family members who have died. The celebrations can sometimes take a serious or a humorous tone, as celebrants remember funny events and anecdotes about the departed, marked by gatherings, music, colorful costumes, and food.
This year, Día de los Muertos celebrations are expected to take place during the global pandemic once again, which means the COVID-19 safety measures observed over the past 20 months should still be followed to protect your loved ones. This is particularly important since 26.2% of all COVID-19 cases in the U.S. have been among Hispanics and Latinos, representing 18.45% of the total deaths from the virus.
To keep everyone protected during this special celebration, Wellstar has compiled some tips for a fun and safe Día de los Muertos celebration.
1 – Vaccination can make celebrations safer: Now that we have the protection of COVID-19 vaccines available, every celebration and gathering can be safer. The more people in your group who have been fully vaccinated, the better for everyone, especially if other safety measures are followed. If you are eligible, be sure and get a booster as soon as you can, too.
2 – Make masks the star of Catrina costumes: Masks are not only fun, they’re also proven to minimize the spread of the virus for everyone age two and older. Get creative by incorporating masks in Catrina costumes and make-up by using fabric paint, glued-on sequins, or stickers to decorate them. In a pinch, use a printed Catrina mask and do your make-up to match or complement the mask. Don’t forget to share photos on social media with the hashtag #celebraciónsegura.
3 – Celebrate outside with appropriate social distancing: Outside is the best place to celebrate. Weather and health permitting, being outside to celebrate Día de los Muertos can promote airflow and help minimize close contact with others. For parades and visits to gravesites, wear a mask and stay at least two meters apart from people who do not live with you. “Air” hugs and waves are much safer than physical hugging and kissing during the pandemic.
4 – Avoid shared food and utensils: Because parties can be a big part of Día de los Muertos, not sharing food and utensils is one of the best ways to keep the spread of COVID-19 in check. If you do get together with a few close friends and family members, take measures to make it a safe celebration by bringing your own meal and utensils to limit sharing or use disposable items. As convenient as it may be, a buffet-style meal is not a good idea during a pandemic. Space your tables and chairs out, possibly outside or in a large area, to limit the spread of the disease, and wear a mask when you are not eating, especially those who are unvaccinated.
5 – Wash hands and sanitize: During the celebration, keep disinfectant wipes nearby to use on surfaces such as tables, chairs, and doorknobs. Everyone should frequently wash and sanitize their hands and remind children and other family members about all safety measures to help keep everyone COVID-free.
6 – Stay at home: Everyone loves a party, but it’s best to avoid any gathering, particularly if you have underlying health conditions such as diabetes, heart or lung issues, obesity, cancer, or other conditions that compromise your immune system. With the rise in pediatric COVID-19 cases, since many children are still not vaccinated, they may also be at greater risk of infection. Anyone can be a carrier or become infected and seriously ill, but these groups are at the greatest risk of contracting and succumbing to COVID. If anyone in your group is feeling ill or has symptoms, it's best to play it safe and stay home to celebrate.
Regardless of how you choose to celebrate Día de los Muertos and the autumn season with fun activities during the pandemic, be sure and refer to the Centers for Disease Control and Prevention guidelines for specific guidance on how to stay safe and well.
Wellstar Paulding Hospital Achieves Magnet® Recognition for Nursing Excellence
Wellstar Health System announces that Wellstar Paulding Hospital achieved global Magnet recognition in October. This honor is a reflection of its nursing professionalism, teamwork and excellence in patient care. The American Nurses Credentialing Center’s (ANCC) Magnet Recognition Program® distinguishes organizations that meet rigorous standards for nursing excellence. Wellstar Paulding Hospital is only the 12th hospital in the state of Georgia to receive this recognition.
With this credential, Wellstar Paulding Hospital joins the global community of Magnet-recognized organizations. Only a small and select group of U.S. healthcare organizations have achieved Magnet recognition due to the complex requirements and meticulous evaluation process. This prestigious honor further underscores Wellstar Paulding Hospital’s commitment to world-class, compassionate, and tailored care in all the communities we serve across Georgia.
“Magnet recognition provides our community with the ultimate benchmark to measure the quality of patient care,” said Jill Case-Wirth, chief nurse executive for Wellstar Health System. “Achieving Magnet recognition validates the culture of excellence that is a cornerstone of how we serve our community. It’s also tangible evidence of our nurses’ and interprofessional teams’ commitment to providing the very best care to our patients, of which we are extremely proud.”
Magnet recognition is the gold standard for nursing excellence and is a factor when the public considers healthcare organizations. U.S. News & World Report’s annual showcase of “America’s Best Hospitals” includes Magnet recognition in its ranking criteria for quality of inpatient care.
Research demonstrates that Magnet recognition provides specific benefits to healthcare organizations and the communities they serve, such as:
“Magnet recognition has many benefits — not just for the nurses who provide care, but also for the patients who receive that care,” said Vicky Hogue, vice president of Patient Services & chief nursing officer at Wellstar Paulding Hospital. “For example, changes in nursing practice are guided by research for better outcomes, which results in higher patient and employee satisfaction and a shorter patient stay.”
The Magnet Model provides a framework for nursing practice, research, and measurement of outcomes. Through this framework, ANCC evaluates applicants across a number of components and dimensions to gauge an organization’s nursing excellence. The foundation of this model comprises various elements deemed essential to delivering superior patient care. These include the quality of nursing leadership and coordination and collaboration across specialties, as well as processes for measuring and improving the quality and delivery of care.
“Ultimately, this recognition aligns with the Wellstar Paulding’s culture of ‘Neighbors caring for Neighbors,” Hogue said.
Staying Healthy with Wellstar for 15 Years
Whether she’s riding motorcycles with her husband, enjoying a roller coaster with her daughter or keeping others well as a chiropractor, Kimberly Smith-Howard stays busy.
But Kimberly still makes time to visit Wellstar Spalding Medical Center for her regular screenings like mammograms—and says she has made health and wellness a priority since her breast cancer diagnosis in 2006.
Kimberly, who has lived in the Griffin area since high school, had just turned 40. She saw her gynecologist for her annual checkup and got her first mammogram. It came back abnormal, and so did her Pap smear. She was diagnosed with Stage 2 breast cancer and cervical pre-cancer.
Kimberly said maintaining a positive attitude helped her through treatment, and she was encouraged along the way by a team of experts.
“When people are going through such a bad time, and they’re not feeling well, it really means so much to have healthcare professionals who are concerned as much about your mental health as they are your physical health,” Kimberly said. “They’re not just there to do a job, get through the day and go home. They’re there to really encourage the patient and make them feel better physically and mentally.”
After chemotherapy, radiation, a lumpectomy and a hysterectomy, Kimberly has stayed healthy for 15 years. Her diagnosis renewed her focus on her own wellness, and she decided to enter the healthcare field herself. In 2011, she went back to school, earning a bachelor’s degree in health coaching and later her chiropractic degree from Life University. Now, she is working on a master’s degree in positive psychology.
Kimberly still goes to Wellstar Spalding for care.
“I’ve always had the most compassionate nurses and the most competent doctors. Everybody has always treated me really well,” she said.
That care she relies on is convenient as well, she added.
“I love being close to home. I love that I have a hospital that does such a great job that’s right at my back door,” Kimberly said.
She encourages women to make time for health screenings and seek care if something seems wrong.
“Always do your routine check-ups and take care of yourself. Know your body,” she recommends.
To schedule a mammogram, call (678) 581-5900.

Preventing Heart Failure Episodes with Easy-to-Use Technology
Remote heart monitoring technology is helping Wellstar patients prevent heart failure flare-ups by keeping their providers up-to-date with real-time information about their health.
The CardioMEMS HF system monitors pulmonary artery pressure. Changes in pressure are an early indicator of worsening heart failure, but providers can often address the issue through some easy adjustments to the patient’s care.
The system gives patients and providers the opportunity to be more proactive in heart care, reducing hospitalizations and helping prevent acute heart failure episodes.
“With heart failure, as with all health issues, it’s best to take preventative action and stop problems from occurring,” Dr. Hans Lee, medical director for Wellstar's congestive heart failure program, said. “Monitoring your heart health and staying in touch with your cardiologist can help keep you out of the hospital and keep your heart in shape.”
The device is implanted by an interventional cardiologist. Once the sensor is implanted, patients take daily readings at their convenience, saving trips to the doctor’s office. Physicians then review the data and contact the patient if needed.
Wellstar offers this technology at Wellstar Kennestone Regional Medical Center, Wellstar North Fulton Medical Center, Wellstar Paulding Medical Center and Wellstar Douglas Medical Center.
Consult with your Wellstar cardiologist to learn whether the CardioMEMS system could be beneficial for your care plan. To find a cardiologist, visit our heart care page.

Halloween 2021: Make it Spooky and Play it Safe
Halloween is right around the corner, and while many Georgians are looking to celebrate this year, many may have questions about how to do so safely.
We’re still in a global pandemic, but we are one year smarter about the best ways to protect ourselves and others from COVID-19, including the safe, effective vaccines that are now available. In fact, the Centers for Disease Control and Prevention recently released guidelines recommending vaccination to minimize COVID-19 risk and to keep family and friends safe while celebrating holiday occasions such as Halloween.
Moreover, Halloween is a great occasion to show your creative flair and incorporate mask wearing. Adding decorative touches to face masks and even transforming a face shield into a superhero mask can be fun and adds a layer of protection from COVID and other viruses.
Wellstar has created these SPOOKY Halloween tips for a healthy Halloween celebration during the pandemic.
S- SANITIZE often and thoroughly. Have your kids wash their hands before heading out, then bring along sanitizer and use it frequently while trick-or-treating. Sanitize candy wrappers when you get home and remind children of safety measures that can help keep everyone COVID-free. If children are visiting your home for trick-or-treating, keep hand sanitizer handy to help prevent the spread of viruses.
P- PHYSICAL DISTANCING is still highly recommended by the CDC. Whether trick-or-treating at a front door or hanging around food and drinks at a party, large group gatherings should be avoided as much as possible. Six feet distancing when possible and small groups are still recommended, even when outside.
O- OUTDOORS is the best way to celebrate Halloween, weather permitting. Being outside promotes air flow and helps minimize close contact with others. If guests are coming to your home for Halloween, consider sitting outside. If you’re planning to make “Grab-n-Go” treats instead of offering a big bowl of treats for kids to dig into, space the bags out for added safety. Reminder: being outdoors doesn’t mean you should ignore sensible safety COVID precautions.
O- OBSERVE your youngest trick-or-treaters. They don’t always know how to stick to the safety guidelines, so keeping an eye on them and making sure that children use face masks, sanitizer, and other safety measures will help make Halloween safe and fun.
K- KIDS having fun and creating positive childhood memories is what Halloween is all about. Try to follow the recommended CDC guidelines for holidays to avoid or minimize COVID exposure while having fun.
Y- YOUR JUDGMENT is key to making good and healthy decisions and minimizing COVID-19 exposure. In addition to wearing masks and getting vaccinated for layers of protection for you and your loved ones, take additional safety precautions such as washing your hands and be sure to stay home if anyone in your family has symptoms.
Wellstar is committed to providing high-quality, tailored, and compassionate care. For more information and the latest updates on COVID-19, visit wellstar.org/COVID-19.

SandyCare
The roots Sandy Kaecher has built in Paulding run deep.
When she moved to Dallas, Georgia over a decade ago, Sandy wanted to make a real difference in her adopted hometown. From countless hours of volunteering to serving on the county commission, she has been a pillar in the community from the beginning.
In 2014, she even attended Wellstar Paulding Medical Center’s groundbreaking ceremony, eager for the area to have easy access to world-class healthcare. However, she never expected to battle breast cancer at the same facility years later.
During her fight, Sandy partnered with an entire team of cancer experts, right here in her beloved community. She also found comfort and strength in a new bond with Wellstar Nurse Navigator Kellie Mitchell, who was by Sandy’s side through her toughest moments.
Every step of her cancer journey, Sandy got unending support from Wellstar—and even a true, lasting friendship, too.
In 2018, while Sandy was gearing up to run in the local election as the first female Paulding County Commissioner, she wasn’t aware that her body was already fighting a battle of its own.
Sandy noticed dimpling on one of her breasts, and knew something wasn’t right.
The distinctive dimpling that Sandy experienced is one warning sign women can watch for between their annual mammograms. During a breast self-exam, women can use their eyes and hands to inspect their breasts for new or concerning changes.
Abnormalities may include a new lump, swelling or thickening of the tissue, red or flaky skin, pulling in or pain in the nipple area and change in size or shape of the breasts.
Breast self-exams are an important way women can stay in tune with their bodies. However, at-home checks are not a substitute for getting a mammogram done by an imaging expert. These screenings are crucial to catch what the naked eye can’t see and detect health issues, such as breast cancer, in its early stages.
That’s why Sandy brought her concerns to her primary care physician right away.
It wasn’t long before she was connected with the cancer team at Wellstar Paulding. There, she received a follow-up mammogram and ultrasound to discover what was the underlying cause of the dimpling.
The advanced imaging technology flagged abnormal results. Her care team got an even better picture of what was going on inside her body after a biopsy.
The results were clear: Sandy was dealing with a complex case of breast cancer. Based on the high-tech images, the cancer had woven in and out of the breast tissue, making it more complicated to treat.
With her expert Wellstar cancer team ready to battle beside her, Sandy summoned her fiery spirit and prepared for the fight.

Conquering Breast Cancer with a Wellstar Support Team
When Ebony-Joy Igbinoba was diagnosed with bilateral breast cancer at age 38, an interdisciplinary team of Wellstar experts stood by her side to help her face cancer with confidence.
Now she is living cancer-free, with a Wellstar care team dedicated to keeping her healthy.
Ebony-Joy started to feel ill at a church concert in spring 2019. She checked in with her primary care provider Dr. Nandini Sunkireddy, who told her that due to the anatomy of her breasts, a mammogram would give a more accurate picture of her health than a traditional exam.
Once Ebony-Joy had gotten her mammogram, Wellstar acted quickly, calling her the same day to get additional images and then a biopsy. Ebony-Joy was diagnosed with bilateral breast cancer—cancer in both breasts, which is rare, especially at her younger age.
Ebony-Joy decided to get a double mastectomy with Wellstar Breast Surgeon Dr. Laura Pearson. Then, she got chemotherapy at Wellstar North Fulton Medical Center. At every step, she found a support system, including oncologists Dr. Carlos Osmon and Dr. Nagender Mankan, as well as Physician Assistant Kristen Gue. Dr. Pearson and Dr. Asaf Yalif completed her reconstruction.
Ebony-Joy said her providers are proactive, friendly and approachable.
“I trust them with my life, and they’re fighting with me,” she said. “They’re rooting for me.”
Ebony-Joy’s care team looked out for every aspect of her well-being—even as she was being treated for breast cancer, her providers paid attention to all her health needs. She saw a Wellstar psychologist, who helped her cope with the diagnosis.
To watch for any side effects of cancer treatment on her heart, Ebony-Joy sees Cardiologist Dr. Natasha Mamdani. Wellstar Gastroenterologist Dr. Inder Tandon and Wellstar Pulmonologist Dr. Nora Hurt also joined her care team to monitor her health.
“God has blessed me with Wellstar doctors, nurses and staff that are truly dedicated to top-notch comprehensive care,” Ebony-Joy said. “They are my superheroes.”
Ebony-Joy’s care team also knew that her diagnosis did not just affect her—they were concerned for her family’s well-being, too. Her nurse navigators referred her to resources about how to talk to children when their parent has cancer, as well as support groups and financial assistance.
“As a single mother, they knew how important it was for me to fight for my kids,” Ebony-Joy said about her Wellstar providers. “I come from an amazing family, and I am happy to add Wellstar to it as they will continue to support me for years to come.”
Ebony-Joy not only stays informed of her own health—she is looking out for her children, too. She learned that she has a gene mutation that also makes her more likely to be affected by pancreatic cancer. She also discovered that two of her great aunts and her cousin all had breast cancer. Now that she knows her family history, her children will get screened at early ages to stay healthy.
Visit wellstar.org/cancercare to learn more about fighting cancer with Wellstar. To schedule a mammogram to check in on your breast health, call (678) 581-5900.

Support for New Moms at Every Step
From your prenatal care through welcoming your family’s newest member, Wellstar provides compassionate, expert care through pregnancy and childbirth. While this is an exciting time for families, it can also be challenging. Wellstar provides several support groups and opportunities to connect with other families.
The Mother Support Circle is a virtual group for postpartum women to discuss the joys and challenges of transitioning to motherhood. You will learn how to support your physical and emotional health, nutrition and mood changes. The group also covers how to promote your baby’s development through interaction, bonding and setting up routines. Meetings are every Thursday from 10 to 11 a.m. on Microsoft Teams.
Breastfeeding has many nutritional benefits for babies, and it can reduce your stress level and help you bond with your child. Whether you're a new mother with questions about breastfeeding, or you want to meet other parents and share experiences, you're welcome to join one of Wellstar's expert lactation consultants for a weekly virtual Q&A. Meetings are held every Wednesday from 2 to 3 p.m. on Microsoft Teams.
Learn more about support groups at Wellstar. To find a provider, visit our women’s health page.

Wellstar Health System Earns Seventh CHIME Digital Health Most Wired Recognition
The College of Healthcare Information Management Executives (CHIME) is pleased to announce that Wellstar Health System has earned 2021 CHIME Digital Health Most Wired recognition as a certified level 8 in acute, ambulatory and long-term care. This is the seventh time Wellstar has received this annual distinction. The CHIME Digital Health Most Wired program conducts an annual survey to assess how effectively healthcare organizations apply core and advanced technologies into their clinical and business programs to improve health and care in their communities.

“Digital transformation in healthcare has accelerated to an unprecedented level since 2020, and the next few years will bring a wave of innovation that empowers healthcare consumers and will astound the industry,” said CHIME President and CEO Russell P. Branzell. “The Digital Health Most Wired program recognizes the outstanding digital leaders who have paved the way for this imminent revolution in healthcare. Their trailblazing commitment to rapid transformation has set an example for the entire industry in how to pursue a leadership vision with determination, brilliant planning and courage to overcome all challenges.”
“This recognition reflects the care, dedication and extraordinary professionalism the Wellstar team brings to work every day in service of our communities,” said Dr. Hank Capps, executive vice president and chief information and digital officer, Wellstar Health System. “Through this challenging season, the team has delivered on Wellstar’s mission of enhancing the health and well-being of every person we serve.”
A total of 36,674 organizations were represented in the 2021 Digital Health Most Wired program, which includes four separate surveys: acute, ambulatory, long-term care and international acute. The surveys assessed the adoption, integration and impact of technologies in healthcare organizations at all stages of development, from early development to industry leading.
Each participating organization received a customized benchmarking report, an overall score and scores for individual levels in eight segments: infrastructure; security; business/disaster recovery; administrative/supply chain; analytics/data management; interoperability/population health; patient engagement; and clinical quality/safety.

Wellstar Recently Partnered with the American Cancer Society to Provide Free Mammograms to Women in Need
When someone has breast cancer, catching it early can be life-saving. As part of Wellstar’s efforts to address health inequity and enhance the well-being of those we serve, Wellstar recently offered free mammograms so local women could check in on their breast health.
A $5,000 grant from the American Cancer Society provided the mammograms, helping to remove barriers to healthcare access. Mammograms, which were promoted through the American Cancer Society website, were available at imaging facilities at Wellstar Kennestone Hospital, Wellstar Cobb Hospital, Wellstar Douglas Hospital and Wellstar West Georgia Medical Center.
Breast cancer is the most commonly diagnosed cancer among women worldwide, excluding skin cancer.
“Unfortunately, one in eight women will develop breast cancer in their lifetime, so early detection is key,” said Dr. Paula Greaves, Wellstar’s chief women’s health officer. “There are some risk factors that women cannot change, such as genetics, but there are some that women can reduce, such as smoking and nutrition.”
Breast cancer is more treatable when it is caught early and treatment can start as soon as possible.
“Mammograms are essential in early detection,” Dr. Greaves said. “It is recommended that women start getting mammograms at age 40, or earlier if there has been a family history of breast cancer — and to continue not only getting mammograms but seeing their gynecologist for regular breast exams.”
To ensure our communities are educated about cancer screenings and have access to essential care, Wellstar has partnered with the American Cancer Society’s Return to Screening initiative.
“The American Cancer Society’s Return to Screening initiative has brought together mammography leaders from across the state for a meeting once a month to brainstorm and collaborate on ways to get women to have their annual screening mammograms,” said Lynn Hanks, executive director of medical imaging operations for Wellstar. “The learning collaborative allows us to share best practices and what has been successful at other locations.”
To schedule a mammogram, call (678) 581-5900.

Shockwave Technology Keeps Heart Care Safe and Efficient
New Shockwave technology at Wellstar is expanding access to life-saving heart care.
If a patient has a complex calcium blockage in their heart arteries, this innovative technology will break up the blockage using sonic pressure waves. It safely cracks the calcium to prepare the artery for stent placement, keeping treatment efficient when time matters most.
Calcium makes the blockage more difficult to reopen with traditional treatments, including balloons. Previously, if a patient’s artery could not be opened using a balloon, the patient would need to be transferred to Kennestone Regional Medical Center with open heart surgery capabilities to undergo an atherectomy — where a physician would break up the blockage with a small drill or laser. With this new shockwave technology, open heart surgery services are not needed as a backup.
Wellstar’s talented and experienced interventional cardiologists are currently using Shockwave technology, also known as intravascular lithotripsy, to treat complex blockages at Kennestone, Cobb, Douglas, Paulding, North Fulton and West Georgia hospitals, allowing complex care to be performed expeditiously, safely and close to home.
Visit wellstar.org/heartcare to learn more about how Wellstar can keep your heart healthy.

COVID-19 Vaccine FAQs
Along with leading healthcare systems throughout the state and nation, Wellstar Health System is requiring all team members to receive the COVID-19 vaccine to help protect the health and safety of our patients, clinical team and community.
Getting the COVID vaccine is the best way to protect yourself, children and the community from the spread of COVID-19 and new variants.
We understand you may still want information, so here are some Frequently Asked Questions about the safety and efficacy of the COVID vaccines.
The Pfizer vaccine is the first to be approved by the FDA for people age 16 and older. The Pfizer vaccine also continues to be available under emergency use authorization (EUA) for children 5 to 15 years old.
Moderna and Johnson & Johnson vaccines are available under EUA for people age 18 and older.
The CDC strongly recommends that women who are pregnant, breastfeeding or may become pregnant receive the COVID-19 vaccine, due to its proven safety and effectiveness. Please consult with your Wellstar OB/GYN provider prior to taking the vaccine. More information is available from the CDC here.
You will be observed for approximately 15 minutes after your vaccination to ensure you have no immediate adverse reactions, which have been very rare. Familiarize yourself with mild and more severe reactions to the vaccine prior to your vaccination. Mild symptoms include soreness around the injection site, headache, body aches and a mild fever. These side effects mean the vaccine is working to create antibodies to help you fight infection.
Serious side effects that could cause a long-term health problem are extremely unlikely following any vaccination, including for COVID-19. Historically, vaccine monitoring has shown that side effects generally happen within six weeks of receiving a vaccine dose. For this reason, the FDA required each of the authorized COVID-19 vaccines to be studied for at least two months (eight weeks) after the final dose. Millions of people have received COVID-19 vaccines, and no long-term side effects have been detected.
Both the Pfizer and Moderna vaccines require two doses. After the initial dose, a second dose is needed at either about 21 days (Pfizer) or 28 days (Moderna). However, if it is not feasible to adhere to the recommended interval, the second dose of Pfizer and Moderna COVID-19 vaccines may be scheduled for administration up to 6 weeks (42 days) after the first dose.
The Johnson & Johnson vaccine only requires one dose.
At this time, scientists are gathering data to determine how long protection lasts. A third booster shot is recommended for certain age groups.
The U.S. Food and Drug Administration (FDA) has recently amended its Emergency Use Authorization (EUA) for COVID-19 booster shots. Now, everyone ages 18 and older should get a booster shot to enhance their protection. Young people ages 16 and 17 can also get their booster, as well.
The timing of your booster depends on which vaccine you have received and how long it’s been since you received the vaccine. For more information, visit our COVID-19 vaccines page.
At this time, your Wellstar physician is not able to provide COVID-19 vaccinations at their office. To find a COVID-19 vaccination site, visit vaccines.gov.
Duration of protection and new strains of COVID-19 are two important factors that will determine if booster or repeat vaccination is necessary. Investigations are ongoing.
Yes. DPH and the CDC urge everyone to get the flu vaccine as soon as possible and the COVID-19 vaccine.
Yes. You need to sign a consent form prior to receiving the vaccine.
We recommend that you check Wellstar’s COVID-19 resource center for the quickest and most convenient general information about COVID-19 vaccines. If you have additional questions, contact us at (770) 956-STAR (7827). If you call us, please be patient as call volumes have been very high recently.
Yes, but if you have COVID-19 it is recommended you wait 30 days after your positive test result. If you have COVID-19 and have also had monoclonal antibody therapy or plasma it is recommended you wait 90 days.
Yes. You can be vaccinated if you have an egg allergy. Both Moderna and Pfizer are mRNA vaccines and do not require egg or egg products to manufacture.
Scientists began developing a vaccine more than a year ago when the SARS-CoV-2 (COVID-19) virus genetic sequence became available, and Pfizer and Moderna had already been working with mRNA vaccines for several years. Because the vaccine includes mRNA and not a killed or attenuated virus, there’s no need to grow the virus in culture, which can be a difficult and time-consuming step.
The Johnson & Johnson vaccine is what’s called a viral vector vaccine.
To create this vaccine, the Johnson & Johnson team took a harmless adenovirus – the viral vector – and replaced a small piece of its genetic instructions with coronavirus genes for the SARS-CoV-2 spike protein.
The adenovirus vector vaccine is safe because the adenovirus can’t replicate in human cells or cause disease, and the SARS-CoV-2 spike protein can’t cause COVID–19 without the rest of the coronavirus.
This approach is not new. Johnson & Johnson used a similar method to make its Ebola vaccine.
Finally, the vaccines were tested in areas with a high infection rate so scientists were able to gauge effectiveness quickly. No shortcuts were taken in development of this vaccine.
No. Neither the Pfizer, Moderna nor the Johnson & Johnson vaccines contain live virus. It is not possible for the vaccine to give you COVID-19.
COVID-19 vaccines are effective at preventing severe illness. According to the CDC, infections only happen in a small proportion of people who are fully vaccinated and, when they do occur, infections are generally mild.
If a fully vaccinated person does contract COVID-19, they can spread the infection to others. That’s why it’s important to continue following the 3Ws — wear a mask, wash your hands and watch your distance — even after you are vaccinated.
Even after you are vaccinated, you should wear a mask. You should also continue to practice social distancing and proper handwashing. No vaccines for any illness are 100% effective, and it takes up to two weeks after the second vaccine for the body to reach peak immunity.
You can take over-the-counter pain relievers after the vaccine if you develop a mild reaction such as a headache or body aches.
Currently, Wellstar is not providing COVID-19 vaccinations at our medical offices. Find a vaccination site near you at vaccines.gov or visit a local retail pharmacy, such as CVS or Walgreens.
For more information about COVID-19 vaccines, visit the CDC website or our COVID-19 vaccine page to learn more.

Conquering Pain with Spine Surgery at Wellstar North Fulton Hospital
With minimally invasive spine surgeries and compassionate, expert caregivers, Wellstar’s spine patients are returning to their routines, pain-free.
Brenda Hawkins was having problems with her neck, and it got to the point where she couldn’t lift her arms above her head.
As her issues got progressively worse, she sought care from neurosurgeons who were unable to treat her. Then, she went to Wellstar North Fulton Hospital, where she not only found a solution, but a true healthcare partner.
Dr. Basheer Shakir, a neurosurgeon at Wellstar North Fulton Hospital, specializes in spine and neck procedures that are minimally invasive, reducing recovery time for patients. Through the front of Brenda’s neck, he was able to remove discs that were pinching her nerves and causing neck and arm pain. She went home from the hospital the next morning.
A few months later, Brenda found herself struggling with a lower back issue that made it hard to walk. She returned to Dr. Shakir, who presented her with another option that was minimally invasive. This time, he did a procedure through the side of her spine to decompress her nerves and fuse her lumbar spine. She was able to walk out of the hospital three days later.
Brenda said Dr. Shakir is "such a great person and did a great job.”
“He's very personable. I just wanted to walk again, and he enabled me to do that,” she said.
Brenda is one of many patients who have benefited from spine surgery at Wellstar North Fulton Hospital. Spine surgery doesn’t just fix back pain — it can also address issues including weakness, loss of dexterity, numbness, bowel or bladder issues and improper posture.
Liz Helgesen had been dealing with low back pain for 20 years. She couldn’t sit for long periods of time, travel on long car rides or get dressed and put shoes on, and she was experiencing muscle spasms after performing simple tasks. To deal with the pain, she had tried several methods including exercise, yoga, physical therapy, dry needling and medication.
Dr. Shakir was also able to help Liz, performing a procedure to shave the bone and make room for the nerves that were being compressed.
Just three months after her surgery, Liz is able to turn and bend without back pain, and she has told her friends and other healthcare providers about how Dr. Shakir has helped her live more comfortably.
Jeff Chandler has also been able to recover with the help of Dr. Shakir and the team at North Fulton. When Jeff fell off a roof last year, he snapped his pelvis in half and broke his ribs and right shoulder. His July 2020 surgery rebuilt his pelvis and sacrum, stabilized his lower spine and decompressed the nerves.
Jeff said his inpatient rehabilitation care team at North Fulton became like family as he began recovery. He’s now able to walk again with no support after the surgery done by Dr. Shakir.
“Dr. Shakir is great. He is kind, encouraging and realistic — which can be scary, but he is very thorough and a good listener,” Jeff said. “He focuses on the bright side of things and did an awesome job in surgery. He is confident and comfortable.”
Wellstar’s expert neurosurgeons can help stop pain, reduce spine degeneration and help you get back to your everyday routine.
“North Fulton offers state-of-the-art procedures and all modern, minimally invasive techniques that allow operations to be done outpatient or with a very short hospital stay with speedy recovery,” Dr. Shakir said.
To make an appointment with Dr. Shakir and find out if spine surgery is the solution for you, call (770) 664-9600.

Wellstar Appoints Chief Diversity, Equity & Inclusion Officer
Wellstar Health System has hired Le Joyce Naylor as senior vice president and chief diversity, equity, & inclusion officer. Naylor began her role on August 2 to provide systemwide thought leadership, strategic planning, and implementation of DE&I initiatives at Wellstar.
“Wellstar is committed to sustaining a diverse, equitable and inclusive environment that honors and values the voice of each patient and team member,” said Candice L. Saunders, president and CEO of Wellstar Health System. “Le Joyce will work with leaders across our organization to advance Wellstar’s diversity, equity, and inclusion (DE&I) and cultural competence programs to positively impact patients, team members and the communities we serve – both today and into the future.”
Naylor has nearly 20 years of diversity and inclusion experience and an exceptional track record of setting strategy, engaging stakeholders and driving results, including leadership of DE&I initiatives in a healthcare setting. Most recently, she served as the executive director diversity & inclusion officer at the Cleveland Clinic. She was responsible for driving the diversity and inclusion strategy and execution for more than 66,000 employees and oversaw the system’s 21 Diversity Councils and 13 Employee Resource Groups. Under Naylor’s leadership, the Cleveland Clinic received National recognition for their employee resource groups, along with being recognized by DiversityInc. as a Top 10 Health System for twelve consecutive years, most notably ranking #1 in 2019.
Wellstar is dedicated to nurturing a diverse workplace that mirrors its communities. Approximately 81% of the company’s employees are women, and just over half (51%) of the workforce is comprised of minorities. When it comes to ascension, 47% of Wellstar’s executives and 77% of frontline managers are women, while minority executives make up 21% of the workforce, with minorities in 38% of the frontline management roles. Also, Wellstar has 7,300 nurses, of which approximately 90.2% of the system’s clinical RNs are women.
In December 2020, Wellstar formally launched the Diversity, Equity & Inclusion Advisory Council to identify opportunities to grow and drive positive change for our communities, patients and team members. As part of her scope, Naylor will lead the council to collaboratively address workforce diversity, a culture of inclusion, cultural competence, health equity, community engagement, and supplier diversity. Wellstar is regularly recognized for diversity excellence, including accolades from Diversity MBA magazine, Diversity Best Practices, Working Mother/Working Father, and National Association for Executive Women (NAFE), among others. Wellstar was also named among Great Place to Work® and Fortune “Best Companies to Work For” and “Best Workplaces for Diversity,” as well as in PEOPLE “Companies that Care,” in part due to the health system’s emphasis on inclusive policies and programs for Wellstar’s workforce and communities.

Lower Your Risk & Recognize Signs of Gynecological Cancer
In recent years, most cervical cancers have become completely preventable with a vaccine, and there are screening tests to identify it early. However, it’s important for women to understand the warning signs of gynecological cancers that don’t have screening tests, such as:
At your annual women’s health appointment, it’s important to talk to your healthcare provider about your family history and lifestyle choices that can make a positive impact on your health. Here are some ideas to consider lowering your risk for different types of gynecological cancer:
Because there are no screening tests for gynecological cancers other than cervical cancer, it is important for women to be educated on the signs and symptoms—and to act on them.
“Unfortunately, there are many vague symptoms associated with a lot of gynecologic issues,” Dr. Carroll said. “Typically, I tell people if you have any symptom that doesn’t come and go but persists for a couple weeks or more, it’s worthwhile to talk to somebody about it.”
Dr. Carroll said that one symptom patients should always discuss with their provider is post-menopausal bleeding. Also, while most people experience occasional bloating, persistent bloating can be a sign of ovarian cancer and should be discussed with a provider, she said.
Some gynecological symptoms to discuss with your doctor include:
The physicians and healthcare teams at Wellstar are focused on keeping women healthy and preventing and lowering the risk of cancer and other health conditions. However, when a woman does get gynecological cancer, she has access to a team of experienced and knowledgeable gynecological cancer experts close to home.
Our gynecologic cancer care program includes:
Take control of your health and learn easy ways to prevent and screen for cervical cancer.

Wellstar Named National Healthcare Diversity Leader
Wellstar Health System has been recognized by Modern Healthcare as one of ten 2021 Top Organizations for Diversity from across the nation. Wellstar is the only health system in Georgia included in the inaugural listing and was honored for demonstrating a commitment to workforce diversity, including leadership positions.
“Healthcare organizations widely promote their diversity, equity and inclusion efforts when they're first announced. But it's more important to track success and make sure those initiatives deliver on the long-term results the companies and communities they serve expect. This year, we increased the cadence of our diversity recognition program and expanded eligibility to include companies as a whole, as well as individuals,” said Modern Healthcare editor, Aurora Aguilar. “The 2021 class of Top Diversity Leaders lead the pack in healthcare. These are people and companies that exemplify ‘walking the walk.’”
This is the inaugural year for Modern Healthcare’s Top Organizations for Diversity awards, which recognize healthcare companies that are “bolstering the diversity of their workforces” at all levels.
“Wellstar is committed to fostering an inclusive culture and workforce that mirrors the communities we serve and celebrates our diversity,” said Candice L. Saunders, president and chief executive officer, Wellstar Health System. “Some of our greatest impacts are a direct result of the diversity of our people: the incredible talent we attract, the daily contributions of our team members, the positive effects we create in our communities, and the programs, resources, and initiatives we implement as a leading healthcare provider. Being recognized as one of Modern Healthcare ten Top Organizations for Diversity honors not just what we do, but who we are.”
Wellstar has a long-standing commitment to diversity, equity and inclusion. In 2020, Wellstar formally launched the Diversity, Equity and Inclusion Advisory Council to identify opportunities to grow and drive positive change for its communities, patients and team members. The Council holds regular listening sessions to ensure the voices of team members across the organization are heard and reflected in a connected cycle of feedback across the system. Every Wellstar facility and department is represented in Wellstar’s diversity efforts.
Nurturing a diverse workplace that mirrors its communities, approximately 81% of Wellstar’s employees are women, and just over half (51%) of the workforce is comprised of minorities. When it comes to ascension, 47% of Wellstar’s executives and 77% of frontline managers are women, while minority executives make up 21% of the workforce, with minorities in 38% of the frontline management roles.
Wellstar believes every person should have access to safe, high-quality healthcare and offers inclusive medical services across its System. In 2019, Wellstar opened a family medicine practice providing specialized health services to people who identify as LGBTQ+. Additionally, physicians are trained to talk about specific issues that the LGBTQ+ community may encounter and support patients through transition goals with gender-affirming care. Wellstar also employs native-language interpreters across the System to serve patients and their families, including a team of full-time Spanish interpreters, a Mandarin Chinese interpreter, as well as full-time Nationally Certified American Sign Language interpreters to support Deaf and hard-of-hearing patients and their families.
Wellstar is regularly recognized for diversity excellence, including accolades from Diversity MBA magazine, Diversity Best Practices, Working Mother/Working Father, and National Association for Executive Women (NAFE), among others. Wellstar recently received two awards exemplifying excellence that include Great Place to Work® and PEOPLE magazine’s 2021 PEOPLE Companies that Care®, and Atlanta Business Chronicle’s 2021 Healthiest Employers. Wellstar has been recognized for outstanding diversity efforts and named in Fortune’s “Best Companies to Work For” and “Best Workplaces for Diversity.”

Partner with Your Provider to Help Prevent Gynecological Cancer
The more you know about your health, the more empowered you are to take control of it. There’s no greater example of the power you have to protect your future when it comes to preventative health visits and cervical cancer. While cervical cancer is one of the most common gynecological cancers, it doesn’t have to be.
With the guidance of their physician, physician assistant or nurse practitioner, women and teens can learn important information and take action that could potentially save their lives. That’s because most types of cervical cancer are now completely preventable.
Cervical cancer typically affects women between 30 and 50 years of age. Younger women are also at risk.
Of course, prevention works best when it starts early. The human papillomavirus (HPV) vaccine prevents cervical cancer. It is recommended to give the vaccine to children around 11 or 12 but can be given as early as 9 years of age.
If not previously vaccinated, the HPV vaccine is recommended for everyone through the age of 26 and can be administered by a primary care provider or gynecologist. Even some adults in their 30s and 40s who were previously unvaccinated benefit from getting an HPV vaccination.
A pediatrician, primary care provider, gynecologist or many pharmacists and healthcare providers in public health departments can administer the vaccine.
The HPV vaccine has been found to provide close to 100 percent protection against infections and pre-cancers caused by HPV.
According to the Centers for Disease Control and Prevention, HPV infections and cervical precancers (abnormal cells on the cervix that can lead to cancer) have dropped significantly since the vaccine has been in use in the United States. Among teen girls, infections with HPV types that cause most HPV cancers and genital warts have dropped 86 percent. There has been a 71 percent decrease for young adult women.
Women can also be screened for cervical cancer at regular intervals. There are two tests that can help:
Most health plans cover preventative care services—like vaccines and screening tests—at no additional cost. For people without insurance, Wellstar practices have low-cost annual exams that include evaluation for cervical cancer and a Pap test if it is medically appropriate.
To find a primary care provider, gynecologist or pediatrician, call (770) 956-STAR (7827) or schedule online by clicking the “Book Now” button at the top of any page.
Take control of your health and read how to lower your risk and recognize the signs of gynecological cancer.

Keeping Hearts Beating with Innovative LVAD Technology
Wellstar’s expert cardiac care specialists partner with patients at every step, from preventative care to high-tech treatments and supportive life-changing advice.
For Mike Clements, the innovative care he received at Wellstar has empowered him to meet his goals and be there for life’s special moments — including walking his daughter down the aisle at her wedding and meeting his first grandchild.
In October 2020, Mike received a Left Ventricular Assist Device (LVAD) implant to support his heart. An LVAD is a battery-powered pump that is surgically implanted and does the job of the heart, pumping blood throughout the body. The external rechargeable battery pack can provide up to 17 hours of power, and most patients with LVAD implants are able to return to work and other routine activities.
For patients whose hearts cannot effectively pump blood on their own, an LVAD is life-saving technology. The device can either keep the patient healthy until they can receive a transplant or serve as an alternative to a heart transplant.
Your Wellstar cardiologist or heart failure specialist can help you determine if an LVAD is the right option for your heart care.
Mike has been a Wellstar patient for decades, beginning when he began experiencing heart issues and was referred to Dr. David Caras for a consultation. As a Wellstar heart patient, he was ready to receive life-saving care right when he needed it, years later.
After Mike received his LVAD implant, an interdisciplinary team of Wellstar providers helped him recover. After Dr. Richard Myung and Dr. Theresa Luu performed the surgery, he spent three weeks in inpatient rehabilitation at Wellstar Kennestone Hospital, guided by an expert team who helped him adjust to life with the implant.
Mike had been on vasopressors to elevate his blood pressure, and when he lost circulation in his toes and developed gangrene, Wellstar Podiatrist Dr. Ashish Kapila performed an amputation of the toes to control the infection, which could have been particularly dangerous with the LVAD.
And when Mike was determined to walk his daughter down the aisle for her June 2021 wedding, Wellstar helped make it happen. He began cardiac rehabilitation and physical therapy at Wellstar Vinings Health Park. He knew the aisle at the church was 40 feet long, so his physical therapy team measured the distance and practiced with him.
In June, he was able to walk with his daughter at her wedding, with the support of his LVAD implant keeping his heart beating with every step. Then in August, he was able to enjoy another family milestone — the birth of his first grandchild.
Mike said Wellstar made his care personal and helped him feel supported on his heart health journey. The LVAD coordinators and nursing team in the critical care unit and cardiovascular ICU and on the blue floor at Kennestone became like family as he began his life with the LVAD, Mike said.
“I can’t say enough great things about Wellstar Health System. They truly deliver ‘PeopleCare,’ from the physicians to the clinical staff to the maintenance team that cleans the rooms,” Mike said. “Rather than taking a cookie-cutter approach, they take the time to know me and my healthcare needs and coordinate care seamlessly. I feel like we’re a team in this journey together.”

Mike walking his daughter down the aisle

DavidCare: Prostate Cancer Survival & Support
There’s no question that David Moffett is a tough guy.
Having served as a Marine and law enforcement officer, he’s been a pillar of strength, both for his family and within the greater community. But after conquering prostate cancer with the help of Wellstar, David has found a new calling: supporting other men going through the same difficult diagnosis.
Since his recovery, David’s been on a mission to break barriers in men’s health. He has started a prostate cancer support group to teach a new meaning of “strength” and help men feel empowered to take charge of their health.
“Being a husband, father and grandfather, people have always looked to me as a leader. I am used to being the protector and being strong,” David said.
“Through my experience with prostate cancer, I’ve learned a man’s greatest strength is vulnerability. You don’t have to be Superman — being yourself and becoming your best advocate are enough,” he said.
With expert care and support from Wellstar, David redefined his role as a protector and learned to prioritize his own well-being too. Now, he’s spreading the message for other men to do the same.
Unlike a lot of men, David never misses his annual wellness exam. Working as an Operations Coordinator at Wellstar, he knows the important role preventative care plays in overall wellness.
During his routine check-up with Wellstar Family Medicine Physician Dr. Thomas Gearhard in 2019, David’s prostate-specific antigen (PSA) level was taken.
With just a simple blood draw, a PSA test can reveal the presence of prostate cancer or other health conditions, such as an enlarged prostate. When David’s test results revealed an elevated PSA level, Dr. Gearhard referred him to a urologist right away.
There, a nodule was discovered in David’s prostate. Following a biopsy, he was diagnosed with Stage II prostate cancer.
“Finding out that I had prostate cancer was devastating,” he said.
But David didn’t have to go through the battle alone. It wasn’t long before he found a trusted health partner in Wellstar Urologist Dr. Paymon Nourparvar. The pair formed a lasting bond as they both worked together to fight prostate cancer.
“Dr. Nourparvar was a blessing. He became like family to me,” David shared. “There was no question he wouldn’t answer, and no question we couldn’t ask. He made me feel like I could open up and talk about the journey I was on.”
Having an open dialogue with patients is a key part of Dr. Nourparvar’s care philosophy. Because he knows not one person is exactly alike, he always takes a personalized approach with every patient.
“There are a wide variety of treatments for people with prostate cancer, and there’s not a one-size-fits-all approach to it,” Dr. Nourparvar explained. “I treat all my patients how I would like my family to be treated. I tailor all of my recommendations and treatments through that lens.”
Based on David’s age, physical health and lifestyle, Dr. Nourparvar felt surgery was the right path forward to treat prostate cancer. However, Dr. Nourparvar wanted to arm him with a breadth of knowledge to make the right choice for his body.
That’s why Dr. Nourparvar encouraged him to get a second opinion with a radiation oncologist — so David could know all the facts before committing to a care plan.
After hearing both treatment plans, David felt empowered to make an informed decision to treat the prostate cancer.
“Dr. Nourparvar was very transparent and made sure he had all the information to choose the right treatment path for me,” David shared. “Then, when my wife and I made the decision that surgery was our best option, I felt like I could make the right choice for my situation.”

Unique Challenges for ECMO in this Pandemic
Dr. Asif Saberi
By Dr. Asif Saberi, Medical Director of Critical Care and ECMO at Wellstar Kennestone Regional Medical Center & Associate Professor of Medicine at Medical College of Georgia at Augusta State University
This wave of the pandemic is unique. We have learned a lot about COVID-19 as a disease, and we have more therapeutic options today than we did in the spring and summer of 2020. But the disease continues to humble us with its tenacity and increased deadliness with each new iteration or surge, and now with its onslaught on the young and the healthy, it is hitting us where it hurts the most.
As a system, we continue to struggle with limited human resources. There are not as many healthcare workers as we need and the steadfast warriors who have stayed at their posts through about 18 months of the pandemic are weary and burnout is high.
This is an important rate-limiting step in our ability to provide one specific therapy, viz., ECMO, which, for a significant number of young people in the extreme manifestation of the disease, is possibly the difference between life and death. At my institution, the phones have not stopped ringing and we maintain a long list of patients who need ECMO. The most heart-wrenching task for us is the daily sorting of our list, moving someone down and eventually off the list as their likelihood of benefit from ECMO and ultimately survival recedes with time.
This is a call to my colleagues in ECMO. Physicians, ECMO specialists, perfusionists, ethicists, and thinkers. As a breed, we are constantly thinking about solutions that are not in any book. Can we solve this problem?

SteveCare
Steve Shelton, a retired middle school principal who lives in Villa Rica, is living life to his fullest years after having a robotic prostatectomy in December of 2014. The procedure was performed by Dr. Justin Watson at Wellstar Kennestone Regional Medical Center.
Robotic prostate cancer surgery has several key advantages over the more traditional approach. It shortens the time spent in a facility following a surgery. It also reduces surgery site blood loss, scarring and pain, and speeds up recovery. This method also has the potential to preserve nerves.
Steve remembered he was in his fourteenth year serving as the principal of Mount Paran Christian School Middle School when his urologist, Dr. Thomas Emerson, broke the news that he had cancer.
“I had to lean up against the wall for a minute,” Steve said. “Dr. Emerson drew out diagrams and presented us with all of our options. My wife, Brenda, and I made the decision right then that I was going to do the robotic surgery. I wanted to be decisive and take action and I wanted the cancer gone.”
Robotic prostate cancer surgery reduces surgery site blood loss, scarring and pain, and speeds up recovery.
“The robot allows us to see the prostate better and spare the nerves, which can preserve sexual function,” said Dr. Watson.

Wellstar Recognized as One of 2021 People Companies that Care and Atlanta Business Chronicle's 2021 Healthiest Employers
Wellstar Health System has received two prestigious awards that exemplify excellence: Great Place to Work® and PEOPLE magazine’s 2021 PEOPLE Companies that Care®, and Atlanta Business Chronicle’s 2021 Healthiest Employers.
The two accolades underscore Wellstar’s focus on “More than healthcare. PeopleCare.”—putting people first both inside and outside the walls of Wellstar across the many communities and regions served by the health system.
“People are at the center of everything we do at Wellstar, and these awards underscore our dedication to compassionate care and wellness for everyone we serve,” said David A. Jones, chief human resources officer, Wellstar Health System. “We are honored and humbled by this recognition, and commit to continuing to nurture our culture of caring and excellence.”

Great Place to Work® and PEOPLE magazine have honored Wellstar as one of the 2021 PEOPLE Companies that Care®. This is Wellstar’s first time being named to this prestigious list, this year coming in at 50th place of the 100 companies recognized. Earning a spot means that Wellstar is one of the best companies to work for in the country. Wellstar is one of only four Georgia-based companies and one of only six health systems included in the ranking.
Wellstar was highlighted for its LGBTQ+ primary care family practice in Atlanta and for the more than $900 million invested last year in charity care, unreimbursed care and community programs as a leading non-profit health system.
“These companies show up for humanity in a variety of ways—from showing compassion for their employees to giving back to their communities to putting diversity, equity and inclusion in the forefront,” says Michael C. Bush, CEO of Great Place to Work®. “They are paving the way for more socially responsible business and are fostering high-trust workplaces for all. Congratulations to the winners of the PEOPLE's Companies that Care list!”
The PEOPLE Companies that Care award is highly competitive and based on analysis of survey responses from more than five million current employees across all industries and U.S. geographies. Companies were only considered if they are a Great Place to Work-Certified™ organization.

Wellstar was recognized on the Atlanta Business Chronicle’s 2021 Healthiest Employers list in the “Extra Large Company” category as one of only two health systems included. Healthiest Employers recognizes the innovative organizations that have created robust healthy workplace programs and companies that go “above and beyond to create a culture of wellness.”
Wellstar was included in this prestigious list as an organization that takes proactive measures to “better the lives of employees through innovative programs and leadership commitment.”
The assessment measures wellness programming in six categories: leadership commitment, foundational components, strategic planning, communication and marketing, programming and interventions, and reporting and analytics.
In addition to serving its mission to enhance the health and well-being of everyone in the communities it serves, Wellstar invests significantly in its more than 24,000 team members across Georgia, with broad and innovative resources, programs, and initiatives. From wellness rooms, concierge services, fitness facilities and services, and childcare support, to paternity leave, wellness apps, and mental health services and hotlines, Wellstar is committed to putting people first and caring for those who provide care for Georgians each and every day.

Neuro Care You Can Count on at Wellstar
When Vera McAdoo was experiencing bleeding in her brain, Wellstar didn’t give up and stayed by her side for every step of recovery.
In September 2019, Vera was at work as an inventory analyst. Then, she suddenly woke up in the emergency department at Wellstar Kennestone Hospital.
She had a bleeding arteriovenous fistula, an abnormal connection between the arteries and veins in the brain. She had been exhibiting some worrying signs. She was not talking, she couldn’t open her eyes, and her pupils were not responding.
But Wellstar Neurosurgeon Dr. William Humphries saw hope, and Wellstar was there when seconds mattered.
Vera was taken to the angiography suite for a catheter-based treatment to control the source of the bleeding before going to the operating room. She underwent an emergent surgery to remove the fistula and treat the swelling in her brain by removing part of her skull.
She was in a coma in the Neuro-Intensive Care Unit for 30 days, but her care team never gave up. Then, as she started healing, Kennestone’s inpatient rehabilitation program stepped in, ensuring she had the tools and support she needed to return to routine.
Kennestone is home to a specialized Neuro-Intensive Care Unit staffed with a multidisciplinary team of neurocritical care physicians, neurologists and nurses experienced in treating the most complex stroke and aneurysm cases.
“It was a blessing that Dr. Humphries was there and saved my life,” Vera said. “My care at Kennestone was great.”
To learn more about how Wellstar treats conditions involving the brain, visit our neuro care site.

Boost Your GYN Health IQ
In the wake of the COVID-19 pandemic, it may be more important than ever for women to brush up on their health IQ to help stay ahead of gynecological health issues. The more you know could potentially save your life one day.
Dr. Jeffrey Hines, Chief of the Division of Wellstar Gynecologic Oncology, said the pandemic caused many women to skip important cervical cancer and breast cancer screenings.
The Health Care Cost Institute (HCCI), an independent, non-profit research institute found women’s health services were significantly affected in 2020 compared with 2019:
Unfortunately, women are already experiencing the consequences.
“There’s an uptick in cancer diagnoses with more advanced disease,” Dr. Hines said. “It’s so important that women realize that it’s safe to go to their providers to get their mammograms and Paps.”

Wellstar Kennestone Lactation Team Celebrates 50,000 Ounces of ‘Liquid Gold’
The breast milk donation program at Wellstar Kennestone Hospital has reached a major milestone — 104 mothers in the community have helped other families by donating 50,000 ounces of breast milk to keep the most vulnerable babies fed and healthy.
Kennestone’s lactation team is dedicated to making sure every baby has the resources they need to stay healthy from the day they’re born, and the hospital’s breast milk donation program gets babies off to the right start.
If, for any reason, a mother is unable to provide breast milk, or enough breast milk for her baby in the NICU, donor milk from a Human Milk Banking Association of North America milk bank can help fill the gap. “For many babies in our NICU, this is life-saving medicine,” said Roxanne Graham, supervisor of maternal and infant support services at Kennestone.
Through Kennestone’s partnership with the Mothers' Milk Bank at Austin, mothers and their babies throughout the country have the option of using donated breast milk, giving babies a head start on all the benefits of breastfeeding.
Breast milk provides babies with infection-fighting antibodies that lower their chances of getting sick. It also offers protection against developing allergies and is easier for babies to digest. Donated breast milk is pasteurized and screened to ensure safety.
“It improves the quality of human life, especially for babies that are medically fragile,” Graham said. Kennestone’s milk depot opened in 2018. The NICU there has been using donor milk since 2012.
“It has significantly decreased the incidence of necrotizing enterocolitis, which is a serious and life-threatening condition associated with premature infants,” said Marie Black, the assistant nurse manager for Kennestone’s NICU. “We highly encourage our moms to pump for their babies but in instances where there is not enough supply, we have our donor milk for those babies.”
To celebrate reaching 50,000 donated ounces, Kennestone’s “Liquid Gold” display showcases the amount received using 390 gallon containers.
If you are interested in donating breast milk, the process is convenient. Donating mothers are asked to become vetted with the milk bank and provide at least 100 ounces for the first donation. After that, smaller donations can make a difference — 5.5 ounces feeds a premature baby for 24 hours, according to the Mother’s Milk Bank of Austin.
Once you have collected and stored your milk, drop it off at a collection site. In addition to Kennestone, Wellstar Douglas Hospital and Wellstar Cobb Hospital also partner with the milk bank.
Call (770) 793-8087 to learn more about donating life-saving breast milk to Kennestone’s milk depot.


Home in Less than 24 Hours
Surgery for prostate cancer has evolved, offering men with aggressive prostate cancer more treatment choices. One high-tech treatment is a robotic prostatectomy, where the prostate is removed robotically by a surgeon with specialized training.
Robotic prostate cancer surgery has several key advantages over the more traditional approach. It shortens the time spent in a facility following a surgery. This method also reduces surgery site blood loss, scarring and pain, and speeds up recovery as well as having the potential to preserve nerves.
“The robot allows us to see the prostate better and spare the nerves, which can preserve sexual function,” said Dr. Justin Watson, a urologist who performs robotic prostatectomies at Wellstar Kennestone Advanced Outpatient Center for Surgery in Marietta. Dr. Watson typically works closely with other prostate cancer specialists to offer patients a multidisipinary approach. This type of care helps patients get the most comprehensive and personalized care.
Read Steve Shelton's story, a man who had a robotic prostatectomy at Wellstar and is living life to his fullest today.

How to Avoid Heat Exhaustion in Hot Summer Weather
Georgia summers are no joke when it comes to high temperatures and humidity, with 90-degree-plus days very common in our summer months. When you’re out and about—and certainly when exercising—it’s important to pay close attention to how hot weather affects your body.
Heat exhaustion and heat stroke can have serious health consequences, but the good news is that you can help prevent these conditions by keeping close tabs on how you’re feeling and taking a few smart steps.
Your body works hard to maintain a healthy temperature, and it knows how to regulate your internal temperature, for instance, by making you sweat to cool your skin. Health concerns can come up, however, when weather conditions overcome your body’s internal monitoring system and your core temperature gets too high.
Here are some of the things you can do to keep your core temperature in a healthy range on a hot day.
It’s important when outside in the summer heat to know your body and be aware of its limits, especially when exercising.
Watch for symptoms of heat exhaustion like:
If you experience symptoms, take steps to cool yourself down.
Seek medical assistance if:
Expert physicians at your nearby Wellstar Urgent Care location are experienced and able to assist with conditions like heat exhaustion. Your doctor will evaluate and monitor your condition, recommending the appropriate treatment to help balance your body temperature.
If you or a loved one cannot safely reach one of our convenient locations, please call 911 for emergency assistance.

FAQ: COVID-19 Data Updates
To best inform our communities about the state of the COVID-19 surge throughout our 11 hospitals, Wellstar Health System is providing weekly updates on our website regarding the current status of COVID-19 patients we are treating system-wide.
In efforts to keep our communities up-to-date and answer any inquiries regarding this data, we’ve answered frequently asked questions below:
Based on FDA and CDC guidelines, Wellstar considers a “fully vaccinated” person to have had either one dose of the Johnson & Johnson vaccine or two doses of the Moderna and Pfizer vaccines with peak immunity achieved two weeks after the second dose.
A booster shot is now recommended for people ages 18 and older to enhance their protection. Young people ages 16 and 17 can also get their booster, as well. The Pfizer booster has been approved for children 12 to 15, and immunocompromised kids 5 to 11 years old.
The timing of your booster depends on which vaccine you have received and how long it’s been since you received the vaccine. Learn more.
While no vaccine prevents someone 100% from getting sick, the COVID-19 vaccines are proven to be safe and effective at preventing severe illness and death. Because a vaccinated person can still contract the virus and may have mild symptoms or no symptoms at all, it’s advised that even vaccinated people still wear a mask and follow safety precautions.
As COVID-19 cases continue to rise and new variants emerge, Wellstar locations may adjust their visitor guidelines based on the level of community spread and to protect our patients and clinical staff. You can learn more about our visitation guidelines here.
Wellstar Health System has mandated that all team members be fully vaccinated against COVID-19 effective October 1, 2021.
We cannot share data regarding the ages of our COVID-19 patients. However, COVID-19 can affect people of any age. The best way to protect yourself is to get vaccinated and receive a booster shot, when eligible. Learn more.
Just as we are seeing vaccinated people become infected with COVID-19, we are also seeing reinfection in those who have had a case of COVID-19 in the past.
This information is available via the Georgia Department of Public Health’s COVID-19 Daily Status Report which provides a detailed analysis of cases, hospitalizations and deaths by county, as well as other demographics.
Out of respect for our patients, we are unable to provide details of patients’ medical information.
Wellstar is reporting the number of patients currently on ventilators system-wide on our website.
Wellstar is reporting the current number of COVID patients in our care, daily.
All COVID-19 patients have been confirmed to be COVID positive with a COVID-19 test.
Yes, Wellstar Health System does administer monoclonal antibodies for outpatient treatment of COVID-19 patients who qualify based on emergency use authorization (EUA) and data on how variants respond to monoclonal antibodies. If you have COVID-19, contact your Wellstar medical provider to see if you are eligible for this treatment.
To find a vaccination site near you, visit vaccines.gov. Get updates and information on COVID-19 at Wellstar by visiting wellstar.org/COVID19.

COVID-19 Testing at Wellstar Urgent Care Centers
As COVID-19 continues to spread, our communities are seeing a surge in cases, especially among the unvaccinated and in children not yet eligible for the vaccines.
If you are experiencing symptoms of COVID-19 or have been exposed to the virus, it is recommended you get tested so you can take action for your health and to help stop the spread.
While Wellstar is offering rapid and PCR tests at all 18 of our urgent care locations, we are experiencing increased wait times due to high demand. Find additional testing locations by visiting a local retail pharmacy, such as Walgreens or CVS, or through your local health department.
Due to the increase in demand for COVID-19 testing and evaluation, online appointment availability at Wellstar Urgent Care Centers may be limited. We are continuing to see patients on a walk-in basis.
While our urgent care centers will perform COVID-19 testing on children 12 and older, Wellstar recommends choosing a testing location based on your child’s medical circumstance. If your child requires a COVID-19 test and is:
For more information, visit our Pediatric Care During COVID-19 resource page.
Wellstar offers rapid and PCR tests. Both tests involve a provider inserting a swab into your nose to collect nasal secretions from the back of the nose and throat.
PCR tests look for viral genetic material in the sample. Test results are usually available within 24 hours. A lab processes the sample. Same-day results are available at the urgent care centers located at Wellstar health parks when testing is completed by noon.
Rapid COVID-19 tests detect specific protein in the sample, which may indicate a COVID-19 infection. The sample is then processed at the testing location. Results are also available at the testing location, normally in 15 to 30 minutes.
At this time, it is strongly recommended that patients with a non-COVID, non-emergency medical need use WellstarON for care, including:
The best defense against COVID-19 is vaccination. Everyone five and older is eligible to get vaccinated, and the shots are very effective at preventing COVID-19. Visit your local retail pharmacy to stick it to COVID and get your vaccine.
However, our youngest community members under the age of five are especially vulnerable because they can’t get their shots yet. As schools are back in session, it is especially crucial that we step up to protect ourselves and our communities. Follow the 3Ws — wear your mask, wash your hands and watch your distance from others — and get a check-up with your Wellstar primary care provider to stay healthy.
Mask Up. Vax Up. Check Up.
It’s been more than a year since the COVID-19 pandemic began, and at Wellstar Health System, we understand many people may feel frustrated. For a moment, life seemed to be getting back to normal, but now it feels as though we’re back at the start.
However, we can’t give up the fight. As new variants of the virus emerge and spread, it’s time to take action.
We have to rise up and take COVID-19 down. It’s up to all of us to make well happen.
That’s because just as much as saving lives and fighting illness happens every day at Wellstar, creating a healthy world starts with you. And right now, we have hope through new, life-saving tools to defeat the virus.
While these actions may seem small, they have a huge impact when it comes to keeping Georgia safe and healthy.
Right now, people who are unvaccinated and children under the age of 12 who aren’t eligible to receive the vaccine are at risk. Vulnerable members of the community are counting on us to step up and get vaccinated.
Together, we can help save lives and keep each other safe.
As you dedicate yourself to doing your part, Wellstar continues to keep the people and communities we serve safe every day. We have been working hard to make well happen, across all of our hospitals, health parks, urgent care centers and hundreds of medical offices.
From suiting up in PPE to keeping our facilities sparkling clean, our team has put additional measures in place to protect our patients and ensure people can receive safe, expert care.
To learn more, visit our COVID-19 resource page.

Wellstar Kennestone Hospital Performs First Neurovascular Robotic Procedure
Wellstar Kennestone Hospital performed its first robotic neurovascular case — a diagnostic cerebral angiogram, which is a procedure used to evaluate blood vessels in the brain. The ability to complete these high-level procedures is now possible using the CorPath System, a robotic-assisted technology. Neurosurgeons Dr. Ahmad Khaldi and Dr. William Humphries performed the procedure.
“The first case with the CorPath System was very successful. Sitting away from the patient in a radiation-protected cockpit, I was able to use a joystick to advance the catheter, millimeter by millimeter,” Dr. Khaldi said. “Additionally, the enhanced visualization of the technology provided me with great control of the catheter. In my opinion, the enhanced control, visualization, and measurement of the CorPath System will transform the way we perform neurovascular procedures and ultimately improve patient care.”
“An aging baby boomer population is driving demand for new innovative technologies to treat strokes,” added Dr. Humphries. “Robotics offers physicians and patients a minimally-invasive technology that may improve the ability to provide rapid endovascular care to patients in the future.”
The CorPath System allows interventional neurosurgeons to perform the procedure remotely, away from the patient bedside. Seated in a radiation-protected cockpit, the physician uses a joystick to robotize catheters and wires to access the neck and brain blood vessels. Additionally, the technology provides neurosurgeons with the ability to accurately measure blockages and precisely position stents. The hope is that this technology will eventually be used for additional stroke treatments to restore blood flow to the brain and treat other complex diseases such as brain aneurysms.
“We are proud to be one of the first medical centers in Georgia to adopt the CorPath System,” said Wellstar Senior Vice President and Wellstar Kennestone Hospital Chief Operating Officer Callie Andrews. “The adoption of the CorPath System at Wellstar Kennestone truly emphasizes our continuous commitment to delivering state-of-the-art technology to our patients and clinical community.”


BacktoCampusCare: What to Know Before You Go
Whether it’s your first time on campus or you’re a seasoned college student, the start of a new school semester can be exciting, stressful and a little scary all at the same time.
Between finding classes on campus and fitting in with new friends, you may be feeling anxious about the upcoming semester. Keep in mind, new-school-year nerves are normal and there are resources to help you — including your Wellstar primary care physician as well as on-campus counselors.
While the COVID-19 pandemic may make your college experience look different this year, you can use your independence on campus to take control of your well-being.
“As you head back to college, your new freedom also means making important decisions about your health,” said Wellstar Pediatrician Dr. Andrew Doyle. “With new variants of COVID-19 on the rise, getting the vaccine is your best defense against the virus.”
“Be sure to follow other safety protocols on campus like the 3W’s — wear a mask, wash your hands and watch your distance — to keep yourself safe,” Dr. Doyle shared.
To help you start the semester off right, here are some wellness tips so you can take on the new year and live your best, healthiest life.
From medical appointments to personal safety, follow our tips to prepare for college and prioritize your health.
Heading to college can be a big transition, and you may feel anxiety about the upcoming changes, especially during a pandemic. But don’t be afraid to ask for help if you need help getting ready or adjusting.
Talking to your Wellstar is a great place to start, whether your concerns are about physical, emotional or mental health. Our health partners are here to support you and can connect you with specialists to keep you feeling well.
Book your appointment today, and be sure to bring up any questions or concerns you have with your doctor.

Marking Milestones with Wellstar Pediatricians
Because you and your child share the same goal—staying healthy and happy—your Wellstar pediatrician will partner with you both. Regular pediatric check-ups are beneficial for the whole family. Your family’s pediatrician will serve as a knowledgeable, trustworthy contact for all your health questions.
As children prepare for the new school year, one step families can take to stay healthy is to head to the pediatrician for an annual check-up.
“Children grow and change so much in their first few years of life,” said Wellstar Pediatrician Dr. Andrew Doyle. “Therefore, it is very important they see their pediatrician every few months during this time.”
In early childhood, your family should see a pediatrician regularly, with check-ups at these ages:
Starting at age 3, children and adolescents should see their pediatrician once a year through age 21, when they can switch to an adult primary care physician to continue their care.
Your family’s pediatrician will get to know you and your child, personalizing care as they grow. Check with their doctor to ensure your kids are up to date on their immunizations and protected from disease. Flu shots are also recommended every year for everyone at least six months old.
To get your child all set for a healthy school year, visit wellstar.org/kidcare to learn more about our expert pediatricians and book an appointment online.

Wellstar Kennestone’s Emergency Department Celebrates One Year Anniversary
The largest emergency department (ED) in Georgia just passed a huge milestone. Wellstar Kennestone Hospital’s new, state-of-the-art ED has now been serving Cobb County and the surrounding community for one year.
From saving lives with advanced medical care to fighting COVID-19 on the frontlines, our expert emergency team has truly risen to the challenge over the last year — and we’re just getting started.
At 263,000 sq. ft., our Level II Trauma Center is more than double the size of the hospital’s prior ED. However, it’s not just the impressive size of the building that sets it apart.
With cutting-edge technology, leading treatments and expert providers always at the ready, the Wellstar Kennestone ED delivers better, faster care when it matters most.
When it comes to emergency care, every second matters.
From top to bottom, the new ED is built to save lives. The innovative layout includes separate care zones based on medical service, level of care and age, allowing us to treat patients faster. We even have a full-service pediatric area so our littlest patients can receive specialized, kid-friendly care.
Since its opening on July 23, 2020, the Wellstar Kennestone ED has:
While those may be a lot of statistics, Wellstar never treats people like a number. With the ED’s high-tech capabilities and smart design, our medical experts can still personalize care even amid a life-threatening situation.
So, whether you or a family member experiences a traumatic injury or sudden medical emergency like a heart attack or stroke, the Wellstar Kennestone ED offers quick, effective emergency care close to home.
Emergencies don’t stop — even during a pandemic. When the Wellstar Kennestone ED opened during the height of the COVID-19 outbreak, Georgians still needed to find safe emergency care.
We’ve added new infection prevention protocols into our already thorough safety routines, ensuring our medical experts can provide safe, life-saving care every day. In uncertain times, people count on Wellstar for expert trauma and emergency care.
Today, the Wellstar Kennestone ED is continuing to protect the people and communities we serve. From emergency surgery to expert trauma care to behavioral health services, we make sure people can get the emergency care they need without going far.
Learn more about the Wellstar Kennestone ED and how we are making a difference in Georgia.

Prevent Summer Spike
By Dr. Danny Branstetter
While the Delta variant has contributed to a sharp increase in new COVID cases, there are still steps we can take to protect ourselves and others.
"The Delta variant is extremely contagious and responsible for the recent summer spike in COVID cases seen all over the world, including here in Georgia," said Dr. Danny Branstetter, medical director of infection prevention for Wellstar Health System. "The best protection against COVID is prevention, and now is the time to prioritize getting vaccinated, practicing safety measures, and getting tested if you are experiencing symptoms or have been exposed."

BacktoSchoolCare: Keeping Kids Healthy & Safe
A new school year is right around the corner. While kids may be the ones returning to the classroom, parents still have their own homework to do too: making sure their child has a healthy start.
Before heading back to school, Wellstar health experts say it’s more important than ever prioritize your child’s physical and emotional well-being.
“Parents can help their children be prepared for school by starting early,” said Wellstar Pediatrician Dr. Andrew Doyle. “Be sure to speak to your children and address any anxieties they may have now about the new school year.”
“Also, getting them scheduled to see their pediatrician for important screenings and immunizations will help them be their healthiest,” he shared.

High-Tech Safe Surgery at Wellstar Kennestone
A cutting-edge cardiac hybrid operating room at Wellstar Kennestone Regional Medical Center brings a catheterization lab and surgery suite together in one space, making treatment more efficient and encouraging collaboration between our expert providers.
The operating room, which treats more than 600 people a year, is outfitted with the latest technology in heart care. The equipment brings together multiple imaging modalities in one environment allowing for an enhanced view of the patient’s beating heart during procedures.
With tableside control of multiple applications in the lab, providers have the freedom of movement to focus on exacting their treatment strategy, thus improving outcomes. This technology is also safer because it exposes both patients and providers to less radiation.
“This state-of-the-art space is the most advanced hybrid operating room in the Atlanta area,” said Dr. Amar Patel, interventional cardiologist and co-medical director for the structural heart and valve program at Wellstar. “Bringing several services into one room allows us to provide complex cardiac care for our community efficiently and effectively, using the top tools available to us.”
Structural heart procedures, such as valve repairs or replacements, will be performed in the hybrid operating room, along with cardiovascular surgery, vascular surgery and some electrophysiology procedures that can determine the cause of heart rhythm problems.
To learn more about how Wellstar can keep your heart in top shape, visit wellstar.org/heartcare.



Innovative Technology at Wellstar Enhances Liver Health
Wellstar East Cobb Health Park now has a new, non-invasive way to get an inside look at your liver health, quickly and painlessly.
An exam with FibroScan, the first FDA-cleared device for diagnosis and monitoring of liver disease, only takes a few minutes, is painless for the patient and produces immediate results for evaluation by a physician.
Results can be used to rule out the need for an expensive, more painful liver biopsy or other invasive procedure.
“When it comes to your liver health, it’s best to be proactive and take action to stay healthy before issues develop,” said Dr. Arif Aziz, chief of Wellstar’s digestive health service line. “This cutting-edge device allows us to monitor your liver without a painful or time-consuming procedure, and since it’s conveniently located at Wellstar East Cobb Health Park, our patients don’t have to travel to take advantage of this new technology.”
The exam only takes about five to 10 minutes. You will lie comfortably on an exam table and raise your right arm above your head. Then, the operator will apply a water-based gel to your skin and place the probe on your ribcage. They will take 10 quick, pain-free measurements. The technology not only saves you pain, it speeds up the diagnostic process as well — results are available immediately for your physician to review.
This new technology can be especially useful for diabetic patients. Fatty liver disease makes it more difficult to control diabetes and can worsen outcomes.
Fatty liver disease can lead to cirrhosis of liver and associated complications. It is one of the leading reasons for liver transplant in the United States.
To learn more about your liver health and schedule a FibroScan exam, make an appointment with a Wellstar gastroenterologist.

Wellstar Kennestone Hospital Celebrates 71 Years of Community Service and Care Excellence
Wellstar Kennestone Hospital, the largest hospital in the nationally recognized nonprofit Wellstar Health System, is celebrating its 71st anniversary. In addition, Wellstar Kennestone is marking a year of significant accomplishments and accolades that include national emergency and trauma care designations, as well as community and national recognition for service and care excellence.
“Wellstar Kennestone Hospital has proudly provided lifesaving and compassionate care to Georgians for 71 years,” said Mary Chatman, Wellstar Health System executive vice president and president of Wellstar Kennestone and Windy Hill Hospitals. “We are an integral part of the community we serve, and so grateful for the support we have received over the past year, which has been especially challenging for everyone.”
“Our exceptional and dedicated team members stand ready to serve the community’s healthcare needs with excellence and compassion,” said Marianne Hatfield, chief nursing officer at Kennestone. “As one of the largest and busiest hospitals in the state, recent designations and accolades we have received simply underscore what we are committed to doing every day: providing expert medical care to people, no matter their age or stage in life.” Founded on June 27, 1950, Wellstar Kennestone Hospital marked its 71st anniversary this week by hosting a small reception to thank hardworking and selfless team members, dedicated community members, and key supporters.
Wellstar Kennestone has a rich history of delivering quality care for Georgians, and has received many national and regional accolades and certifications for care excellence over the years. The hospital recently received the highest level of recognition for emergency cardiac care in Georgia and was designated a Level I Emergency Cardiac Care Center by the Georgia Department of Public Health, Office of Cardiac Care.
Wellstar Kennestone Hospital was also verified as one of only four Georgia Level II Trauma Centers by the American College of Surgeons. This achievement recognizes the Trauma Center's dedication to providing optimal care for injured patients.
Wellstar operates the largest trauma network in Georgia, with Wellstar Kennestone managing one of the nation's newest and largest emergency departments, with state-of-the-art care for pediatric and adult patients. The new emergency department is connected to the main hospital and is located near the intersection of Church and Cherry Streets at 115 Cherry Street NE, Marietta, Georgia 30060.

Wellstar Kennestone Hospital celebrated its 71st anniversary by hosting an ice cream social to thank team members for providing outstanding and compassionate care to the community.
Wellstar Physicians Named as “Top Doctors” in Atlanta Magazine’s 2021 List
Wellstar Health System has announced that Atlanta magazine recognized 79 Wellstar physicians on its 2021 "Top Doctors" list in the July issue. This list is compiled annually from nominations by physicians whom they consider to be among the top experts in their region for their medical specialty. The number of Wellstar doctors named to the distinguished list increased 14% from 2020 to 2021.
"As a community-based, non-profit health system, Wellstar physicians are focused on providing high-quality patient-centered care to everyone who comes through our doors," said Dr. John Brennan, executive vice president and chief clinical integration officer of Wellstar Health System. "Wellstar is extremely proud of the doctors recognized by this prestigious list published annually by Atlanta magazine, as well as all of our team members, who are committed to delivering outstanding care to every person, every time."
Atlanta magazine's "Top Doctors" list is compiled by Castle Connolly Medical Ltd., a leading healthcare research and information company founded to help consumers reach America's top doctors and hospitals. Physicians are nominated by their peers and selected after a rigorous screening process that reviews professional, educational, and patient care excellence. The final list with detailed information about the doctors’ education, training, and medical expertise is included in Atlanta magazine's July 2021 issue. Below is the complete list of Wellstar physicians who were honored on the 2021 list.


Hey Man, Make Health Your Habit
If you’re a sports fan, you probably know your stats.
Like how NBA Hall of Famer Dominique Wilkins remains undefeated in Atlanta Hawks history for points (23,292) and ranks second in team history in steals (1,245). But there are a few, even more important numbers you should know off the top of your head: your health stats.
Do you know your blood pressure? What about your low-density lipoproteins? Maybe you can clock an eight-minute mile or bench press 250 pounds, but do you know your hemoglobin A1C?
Men are less likely than women to see their healthcare provider once a year. Wellstar Primary Care Physician Dr. Tameka Byrd said it’s crucial men stay up to date on preventative care and essential screenings.
“Yearly physicals can catch illnesses before they start and prevent health issues from getting worse,” Dr. Byrd said. “Your primary care provider will tailor a screening plan depending on your age, health history and other factors so you can proactive with your wellness.”
Getting and staying healthy doesn’t just help us feel better—it ensures we can be there for those we care about too.
“It’s also for loved ones—spouses, partners, children and parents. We’re not only here for us. We’re here for our friends and family,” said Wellstar Urologist Dr. Scott Miller. “The best thing you can do for those you care for is to take care of yourself.”
Stats all men should know to stay in the game include:
BMI determines whether you have a healthy body weight and categorizes obesity levels. A recommended BMI range is between 18.5 to 25.
This blood test measures cholesterol levels and should be part of your wellness routine starting in your 20s. For men 20 or older, healthy LDL levels should be under 100 milligrams per deciliter and aim to keep your HDL above 40.
Your provider will take your blood pressure during your regular visit, but you can also find blood pressure checking stations at many pharmacies or buy your own device to use at home. Blood pressure under 120/80 is considered ideal.
This metric measures whether or not you have healthy blood sugar. If you are diabetic, you should check your A1C every three months.
Men who are 50 or older should discuss prostate cancer testing with their provider, according to the American Cancer Society. Men at a higher risk, including Black men and those who had a brother or father diagnosed with cancer before age 65, should ask their provider about testing at age 45. Patients who had more than one close relative with prostate cancer at an early age should have this conversation with their provider when they’re 40. The Wellstar Prostate Health Program evaluates and treats people with a higher risk for prostate conditions.
An abnormal PSA result could be an indication of prostate cancer. For men in their 40s and 50s, a PSA score higher than 2.5 nanograms per milliliter is considered abnormal, and men in their 60s should have a PSA score of 4.0 nanograms per milliliter or less.
Along with staying up to date on those health stats, men should also be getting regular colorectal cancer screenings. The American Cancer Society recommends that people at average risk for colorectal cancer screening get checked regularly beginning at age 45. Screenings should continue through age 75, and after that patients can discuss their personal risk and history with their provider.
Your Wellstar primary care provider will partner with you in creating a personalized health plan. Find a provider near you and book online or locate an Augusta area provider.
Wellstar Innovation Series Explores Future of Healthcare
More than 100 participants attended the virtual roundtable event, which included a panel discussion and breakout sessions focused on leading technologies that have the potential to transform healthcare. The panel was moderated by Julie Teer, senior vice president of Wellstar and president of the Wellstar Foundation. Panelists included:
“There has never been a time in healthcare when getting the technology strategy right was more imperative than now,” Dr. Goldsmith said. “There is a massive transformation underway in healthcare to significantly increase clinician productivity and enable teamwork across the care continuum, which will be a huge boost to patient satisfaction. Thank you to Wellstar for hosting this important conversation to fuel innovation.”
Digital health is transforming healthcare through integrating innovation and advanced technology into patient care, improving quality of care and expanding access. In addition to the panel, three breakout sessions facilitated conversation about leading-edge, advanced technologies, including:
Physician leaders from Wellstar Medical Group provided expert insights in the breakout discussions on the potential applications and impacts of these technologies on the future of healthcare. Physician experts included:
“The future of healthcare is not a 2025 vision – it is a 2021 reality,” said Sharecare’s Arnold. “Georgia continues to strengthen its position as a global center for public health, information technology, and digital media; and Wellstar is at the center with their focus on partnerships and healthcare innovation. Discussions such as the Wellstar Innovation Series help create momentum around viable solutions that will address gaps in care and a make a meaningful difference in the health and well-being of communities throughout the Peach State and beyond.”
The event followed Wellstar’s March 3, 2021 announcement that it will become the country’s first Sharecare-enabled health system, and the May 18, 2021 launch of Catalyst by WellstarTM, the first-of-its-kind global digital health and innovation center created and operated within a health system. Catalyst by Wellstar is designed to harness, accelerate, optimize, and scale people-centric solutions that:
To further fuel healthcare transformation, Wellstar also announced a partnership with Engage, a collaborative innovation and corporate venture platform. Wellstar is the only healthcare company to partner with Engage, alongside other partners Chick-fil-A, Cox Enterprises, Delta Air Lines, Georgia-Pacific, Georgia Power Foundation, Georgia Tech, Goldman Sachs, The Home Depot, Inspire Brands, Intercontinental Exchange, Invesco, Invest Georgia, Tech Square Ventures, and UPS.
The Wellstar Foundation’s Innovation Series convenes thought leaders, community partners, and industry experts in a series of roundtable discussions to explore how to transform healthcare to better serve Georgians. The conversations aim to facilitate collaboration that will lead to meaningful action and a pathway to transforming healthcare in Georgia. The series covers topics of health equity, digital health technologies, behavioral health and wellness, women’s health and pediatrics, and workforce planning.

Team Up with Wellstar to Fight These Men’s Health Issues
If you’re a sports fan, you’re probably glued to every game, rooting for your team and analyzing every play. But are you as vigilant with your own health?
In addition to knowing your health stats—those important numbers like blood pressure, cholesterol and blood sugar—you should also watch for health conditions that more commonly impact men.
An annual physical gives you the opportunity to ask your provider questions about your health, and you’ll get a few quick, crucial health screenings that can catch issues early and put you on track for staying well.
“See your primary care provider at least once a year to check in on your well-being and stay up to date on essential screenings you may need,” said Wellstar Primary Care Physician Dr. Facia Dew. “Your provider will customize care based on your health history, age and other factors to help you feel your best.”
Some illnesses are more likely to affect men than women, so men should be especially mindful about taking steps to prevent these issues:
Men are slightly more likely to get lung cancer—the lifetime risk for men is 1 in 16, while it’s 1 in 17 for women, according to the American Cancer Society. Black men are about 12% more likely to develop lung cancer compared to white men. Decrease your risk of lung cancer by avoiding smoking.
With a low-dose CT scan of the chest, it only takes a few seconds to check in on your lung health. An order from your provider is required for a lung cancer screening. Contact your Wellstar primary care provider or a pulmonologist to discuss if screening is right for you.
Men are 1.5 times more likely than women to have Parkinson’s disease, according to the Parkinson’s Foundation. Wellstar neurologists and neurosurgeons are experts in helping patients manage this condition.
The risk of kidney stones is about 11% in men and 9% in women, according to the National Kidney Foundation. You can reduce your risk of kidney stones by staying hydrated and eating a low-sugar, low-sodium diet. Your provider can help you evaluate your risk factors, including personal and family history, obesity and being 40 or older.
While all men are at risk for prostate cancer, Black men are more likely to get prostate cancer and are more commonly affected at younger ages. Men who are 50 or older should ask their doctor about testing, and Black men should discuss testing with their provider at age 45. If you have a family history of prostate cancer, you should also consider screenings at a younger age, and your provider will discuss options with you.
According to Wellstar Urologist Dr. Scott Miller, men need to stay active and stay away from smoking. He also noted a few lifestyle changes that are sometimes overlooked can make a difference in how you feel.
“What’s often neglected is a full and consistent night’s sleep,” Dr. Miller said. “And keep stress under control—too much stress can negatively impact our immune systems.”

Improving PeopleCare with New Telesitter Technology
A new, cutting-edge technology is coming to Wellstar — and will be a gamechanger for patient safety.
Wellstar Kennestone Hospital and Wellstar Paulding Hospital are the first in our system to adopt Telesitter, a remote video monitoring system designed to protect at-risk patients.
The state-of-the-art system includes in-room video, two-way audio capabilities and a central monitoring station where trained team members are ready to act in the event of an accident, injury or other emergency situation.
In addition to our frequent in-person checks, this technology helps ensure patients remain safe throughout their stay. It’s the latest way we’re keeping our promise to deliver PeopleCare to each and every person we serve.

LGBTQ Care: High-Quality Healthcare for Everyone
With dedicated health resources and caring, compassionate providers, Wellstar is making primary care more accessible to people who are lesbian, gay, bisexual, transgender and queer/questioning (LGBTQ+).
Historically, many healthcare systems have not focused on the specific needs of the LGBTQ community.
“The LGBTQ community has been marginalized by the healthcare system,” Wellstar Primary Care Physician Dr. Gabriella Maris said. “There is a lack of providers who have adequate training to understand and treat their unique health risks.”
Wellstar believes every person should have access to safe, high-quality healthcare. At each of our primary care locations, we maintain a welcoming, non-judgmental environment to treat patients. Across Wellstar, we’re committed to providing inclusive medical services in a safe, comfortable space to make LGBTQ care more available.
Members of the LGBTQ community may be at a higher risk for certain medical issues.
For example, lesbian and bisexual women may be at increased risk for breast, cervical and ovarian cancer, according to the American Cancer Society. The American Psychiatric Association also shared that LGBTQ people are more likely to experience mental health concerns and use mental health services.
Treating these health concerns starts with trained providers who take a caring, compassionate approach to help patients stay healthy.
Wellstar provides primary care for the LGBTQ community, including wellness exams, chronic disease management, virtual appointments and other health screenings. We also offer special services for people who identify as LGBTQ including:
Gender-affirming care is medical treatment that supports a patient’s gender identity when their identity differs from their sex assigned at birth.
“Gender-affirming care has the ability to save lives,” said Wellstar Primary Care Physician Dr. Danielle Ortega. “We know that a large percentage of transgender individuals, even starting in adolescence, have either suicidal intent or attempts in the past, and we know that gender-affirming care, when appropriate, improves mental health and prevents suicide.”
Wellstar physicians provide great care to patients and our health experts are dedicated to being a true partner in your wellness journey.
“I want for patients to know that Wellstar is their medical home—for them to feel comfortable when they walk in our door and for them to know that this is going to be a clinic that is not judgmental, is truly empathic and is here to help them in whatever way we can,” Dr. Maris said.
Our primary care team puts patients at the center of their care, presenting them with all their options and working with them to decide how to accomplish their goals.
“I get to know patients and understand what their goals are, what their hopes are, who their supports are, what their job entails, what their community is like and, specifically, what their goals are in relation to their health,” Dr. Ortega said.

Wellstar Kennestone Hospital Verified as Level II Trauma Center by American College of Surgeons
Wellstar Health System, which has the largest trauma network in the state, has announced that the Wellstar Kennestone Hospital Trauma Center has been verified as one of only four Georgia Level II Trauma Centers by the American College of Surgeons (ACS). This achievement recognizes the Trauma Center's dedication to providing optimal care for injured patients.
Building on Wellstar’s commitment to healthcare excellence, the system was also named a top-five finalist for the American Hospital Association’s 2021 Quest for Quality Prize and had 130 physicians – representing almost 26% of the total list – named as Georgia Trend “Top Doctors.”
Wellstar operates the largest trauma network in Georgia, with Wellstar Kennestone’s new state-of-the-art emergency department, which opened in July 2020, being one of the largest and busiest in the nation. Kennestone provides comprehensive trauma care, with 24/7 access to on-site trauma, critical care trained surgeons, and a wide range of surgical subspecialties to consistently meet the needs of the most seriously injured patients following the highest care, quality and safety standards.
Established by the ACS in 1987, the Committee on Trauma’s (COT) Consultation/Verification Program for Hospitals promotes the development of trauma centers. Participants provide the hospital resources and level of care necessary to address the needs of all injured patients across the entire trauma continuum of care. Trauma center verification provides a structure for trauma care that can raise the overall level of performance throughout a hospital.
This prestigious verification recognizes the Wellstar Kennestone Trauma Center’s commitment to providing the highest quality of care for injured patients, spanning community outreach and injury prevention efforts, emergency trauma, operative care, critical care, and rehabilitation.
"Receiving this verification further validates the exceptional life-saving care we provide at Wellstar Kennestone for patients who have suffered from all ranges of traumatic injury," said Mary Chatman, Wellstar Health System executive vice president and president of Wellstar Kennestone and Windy Hill Hospitals. "We are so proud of the Trauma Center team's commitment to ensuring that all patients get the appropriate care in a timely and coordinated manner because our communities rely on Wellstar to provide the very best care for every person, every time."
Trauma is the leading cause of death and disability between ages 0-44 and the fourth leading cause of death overall. According to the Georgia Trauma Foundation, nine main causes account for 92.1% of trauma in Georgia. The leading causes of major trauma are motor vehicle crashes (37.7%); falls (22.2%); gunshot wounds (8.0%); motorcycle crashes (5.4%); pedestrian incidents (5.2%); assaults (4.3%); accidents (4.0%); stab wounds (2.9%) and all-terrain vehicle crashes (2.4%).
As an additional indicator of excellence, Wellstar was one of only five national American Hospital Association 2021 Quest for Quality Prize finalists. The award recognizes healthcare leadership and innovation in providing, improving, and advancing health in communities.
Nominees are highlighted for partnering with community organizations to improve health outcomes, developing new models of care, and collaborating with patients to design the patient care experience. One way that Wellstar addresses vital community needs to enhance health and wellness is via the Wellstar Center for Health Equity (WCHE). Over the past year, the WCHE orchestrated multiple, high-impact initiatives, including free pop-up COVID-19 testing, mobile food markets, and anchoring vulnerable patients with resources, benefiting thousands of Georgians. Wellstar was also honored for pandemic response efforts, including quickly leveraging telehealth to serve patients, creating team member mental wellness programs, and allocating and redeveloping resources across the system.
The May issue of Georgia Trend included the 2021 “Top Doctors,” the second annual listing of the state’s top physicians. Close to 26% of the physicians on the list were part of the Wellstar Health System enterprise, totaling 130 doctors across the majority of categories.
Physicians deemed by Georgia Trend as “outstanding” span Wellstar’s service areas, facilities, and service lines, including cardiology, neurology, gynecologic oncology, pulmonology, internal medicine, family medicine, emergency medicine, radiology, endocrinology, pediatric orthopedics, spine surgery, and sports medicine, among others. The physicians are selected via peer voting and review of government information sources. Inclusion on this list of the top medical experts in the state further validates Wellstar’s commitment to world-class healthcare.

Wellstar Saves Lives with Advanced Stroke Care
No one expects to have a stroke—much less one that is rare or complicated to treat. However, these life-threatening medical events can happen to anyone, at any time.
That’s why Wellstar now offers the highest level of stroke care at three locations: Wellstar Kennestone Regional Medical Center, Wellstar MCG Health Medical Center and Wellstar North Fulton Medical Center. Here, patients have access to cutting-edge treatments, advanced technology and an expert neuro team, ready to treat even the most complex strokes.
Our primary stroke centers—including Wellstar Cobb, Wellstar Douglas, Wellstar Spalding and Wellstar West Georgia Medical Centers—are also poised to deliver high-quality stroke care where it’s needed most.
“Wellstar has nine hospitals that provide stroke care in our network,” said Dr. Rishi Gupta, director of stroke care at Wellstar.
Wellstar is the leading provider of stroke and aneurysm services in the state and performs one of the highest numbers of thrombectomy and aneurysm treatments in the country.
When a stroke threatens your life and brain, the neuro specialists at Wellstar have the expertise and experience to treat even the most complex cases.
At our Comprehensive Stroke Centers, the neuro teams use state-of-the-art therapies and technologies to care for strokes faster and more effectively. These include:
With new neurotechnology, Wellstar is changing how strokes are diagnosed and treated locally and across the country.
“We’re now able to do things like telestroke, which allows remote physicians to provide the same level of care while in the emergency room of another hospital,” Dr. Gupta said.
“With artificial intelligence, our team can look at images and assist physicians in rural communities. This technology can determine if a patient experiencing a stroke should seek a higher level of care in a metropolitan area.”
Remember, while Wellstar jumps into action at the first signs of a stroke, stopping one starts with you. Learn signs to spot a stroke or ways to prevent a stroke before it begins.

Spotting Skin Cancer Early
When people plan outside activities or a trip to the tanning salon, skin cancer may be the last thing on their minds. However, prolonged or intense exposure to ultraviolet (UV) rays — either from the sun or tanning beds — is harmful to your skin.
Skin cancer can be sneaky when it starts. The disease often begins as just a mole and, if left untreated, can develop into a bigger skin problem. Melanoma, a dangerous type of skin cancer, is a growing concern for many health experts.
“Of all skin cancers, melanoma is the most serious and it is becoming increasingly more common worldwide,” said Dr. Dean Kirkel, oncologist with Northwest Georgia Oncology Centers. “The disease can spread to the lymph nodes and other parts of the body, and even be potentially fatal.”
Since hiding away from the sun isn’t an option, you can make better choices for your skin health, such as wearing sunscreen, skipping the tanning bed and avoiding sunburns.
In addition to protecting your skin, you can take charge of your health with simple steps to catch skin cancer earlier.

Wellstar Announces First-of-its-Kind Global Digital Health and Innovation Center
Building on a rich history of innovation and impact in healthcare delivery, Wellstar Health System has launched Catalyst by WellstarTM, a global digital health and innovation center.
As part of the center’s work, Wellstar has partnered with corporate innovation and venture platform Engage to connect and collaborate with industry-leading corporations, enterprise startups, and universities to fuel innovation. To foster meaningful discussion, action, and philanthropy around healthcare innovation, the Catalyst by Wellstar leadership team will participate in a Wellstar Foundation-hosted Innovation Series virtual event on June 15.
Catalyst by Wellstar is the first-of-its-kind global digital health and innovation center created and operated within a health system to holistically address healthcare disruption by harnessing problems, solutions, investments, and partnerships across industries. The center defines and drives leading-edge, transformative solutions that enhance the health and well-being of people and communities with world-class results and impact.
As technology continues to advance and consumers become more empowered by digital solutions and information access, innovation to solve problems and seize opportunities will evolve and impact how healthcare is delivered and used. Wellstar is committed to transforming healthcare through problem sourcing from patients, community members, physicians and team members, and partners to lead mission-driven innovation. Catalyst by Wellstar is designed to harness, accelerate, optimize, and scale people-centric solutions that:
“Innovation is vital to our mission of enhancing the health and well-being of every person we serve, today and into the future,” said Candice L. Saunders, president and CEO, Wellstar Health System. “Catalyst by Wellstar positions us to lead change across our system, communities, and the healthcare industry.”
Catalyst by Wellstar convenes and activates best-in-class entrepreneurs, philanthropists, innovation ecosystems, research and development experts, corporate partners, academicians and scientists, and thought leaders inside and outside of the healthcare industry. The center will encompass innovation that drives positive impact related to:
“There is endless opportunity to transform healthcare in positive and meaningful ways,” said Dr. Hank Capps, executive vice president and chief information and digital officer, Wellstar Health System. “With Catalyst by Wellstar, our system is poised to purposefully drive innovation faster than the speed of change through thought leadership and collaboration. Our global digital health and innovation center will equip Wellstar to transform the way healthcare is delivered for years to come.”
The first Catalyst by Wellstar partnership is an investment in Atlanta-based Engage, a first-of-its-kind collaborative innovation and corporate venture platform. Engage brings together industry-leading corporations, enterprise startups, and universities with the shared mission of elevating Atlanta and the Southeast as a leading technology and innovation hub. Wellstar is the only healthcare company to partner with Engage. Saunders has joined Engage’s board of directors and Capps has been named to the Engage Advisory Board.
“As a regional and national healthcare leader, Wellstar brings critical industry perspective to the Engage platform,” said Daley Ervin, managing director of Engage. “Our corporate partners are facing challenges posed by large-scale digital transformation and rapidly evolving customer expectations. Through this partnership, Wellstar will benefit from the expertise of a broad network of industry-leading companies while also leveraging the startup and university research ecosystem on their journey to design the future of healthcare.”
As a result of Wellstar’s investment in Engage, the system will have the opportunity to collaborate with startup technology companies as part of the innovation process, alongside other Engage partners: Chick-fil-A, Cox Enterprises, Delta Air Lines, Georgia-Pacific, Georgia Power Foundation, Georgia Tech, Goldman Sachs, The Home Depot, Inspire Brands, Intercontinental Exchange, Invesco, Invest Georgia, Tech Square Ventures, and UPS. The Engage Fund is managed by Tech Square Ventures. Engage’s exclusive partnership with Georgia Tech, one of the country’s top research and technology commercialization universities, provides unique access to its startup, innovation, and research initiatives.
“Healthcare is one of the strategic areas of focus for UPS and I am thrilled to welcome Wellstar to the Engage partnership," said Matt Guffey, president of Global Strategy and Transformation at UPS and Engage Advisory Board member.
The second Wellstar Foundation Healthcare Innovation Series virtual roundtable will take place on June 15, 2021 from noon to 1:30 p.m. The event will focus on “Designing the Future of Healthcare,” with emphasis on the role of technology and innovation. The Series convenes community, philanthropic, and thought leaders to facilitate conversation and collaboration to propel the transformation of healthcare. More than 100 participants attended the inaugural event and engaged in discussion about how to enhance health equity. For more information, contact [email protected].
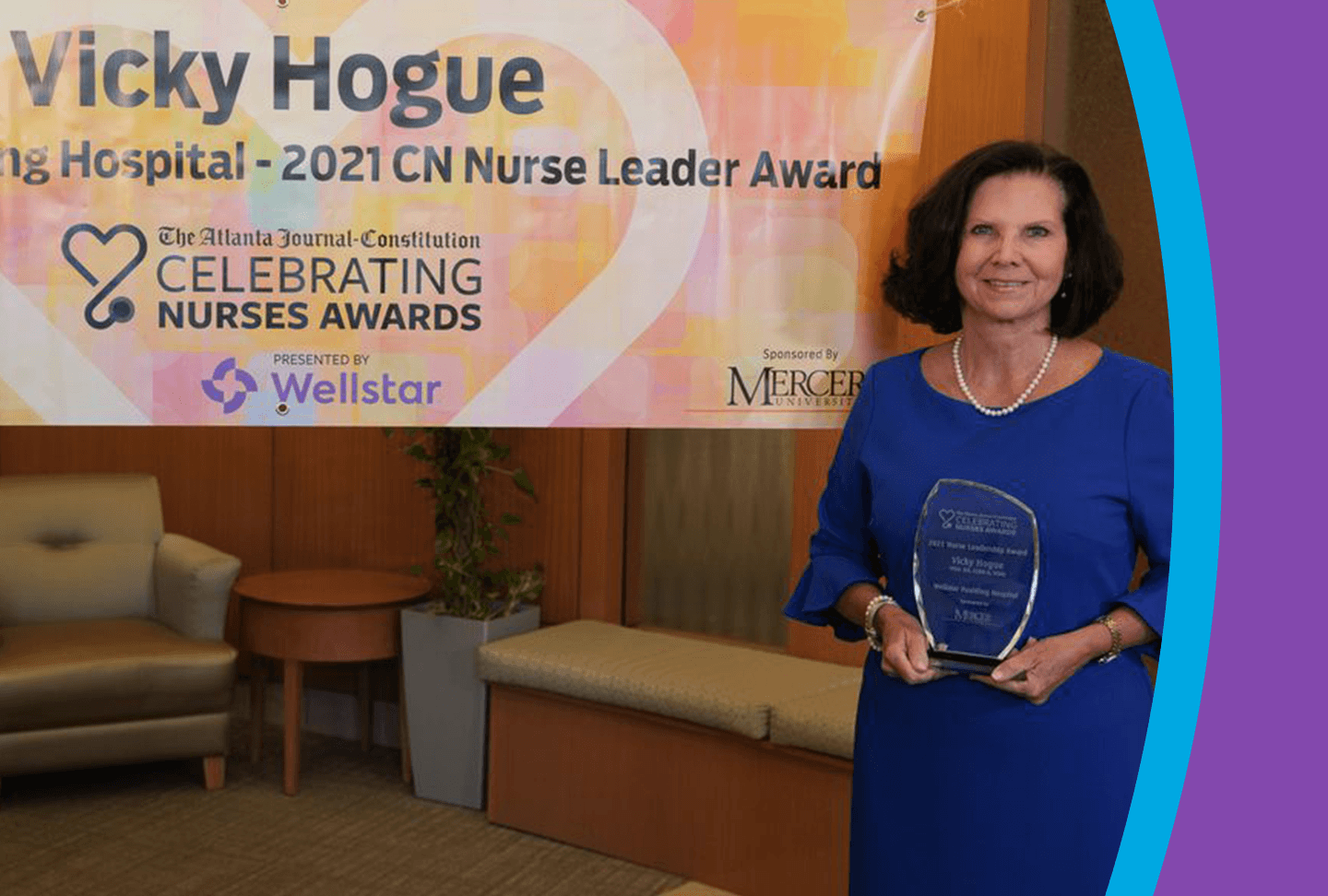
Wellstar Wraps Up Special Week of Gratitude for Nurses
Wellstar Health System wrapped up a weeklong celebration of its healthcare heroes during National Healthcare Week and National Nurses Week honoring team members for their selfless service, sacrifices, and dedication amid the pandemic. Wellstar team members were also recognized by the Atlanta Journal-Constitution and Atlanta Business Chronicle for outstanding work and serving their communities with compassion and excellence.
The Atlanta Journal-Constitution’s 16th Annual Celebrating Nurses Awards honored four Wellstar nurses, including selecting Vicky Hogue, chief nursing officer at Wellstar Paulding Hospital, as the Nurse Leadership Award recipient. Hogue will celebrate 41 years with Wellstar in August and her background includes working as a critical care and ICU nurse. When the pandemic began, she said that the crisis was exactly what she and her fellow nurses have trained for — answering the call to care for the community. In addition to nursing leadership, Hogue was highlighted for serving as a nurse advocate at the local, state, and national levels, volunteering to administer COVID-19 vaccinations and providing unwavering support for team members. Given annually to an outstanding nurse director, Hogue was chosen from 47 nominees to receive the Nurse Leadership Award.
Additional honorees included:
• Clayton Fowler, Wellstar Kennestone Hospital: A registered nurse for 11 years, Fowler helped to care for some of Wellstar’s sickest ICU patients during the height of the pandemic. In March 2020, Wellstar Kennestone was converted to take care of critical COVID-19 patients, and Fowler served on the frontlines providing life-saving therapies, such as extracorporeal membrane oxygenation (ECMO) treatment.
• Laurie Pazda, Wellstar Kennestone Hospital: A veteran nurse with more than 20 years of service, Pazda works in the cardiac intensive care unit and helped provide care for intubated COVID-19 patients designated to negative pressure rooms.
• Laura Moss, Wellstar Spalding Regional Hospital: Moss became a registered nurse in 2019 and immediately started a career of service by providing compassionate care to Wellstar patients. During the pandemic, Moss served as an extended family member to many COVID patients and helped the family of one intubated COVID-19 patient communicate with distant family members by setting up nightly FaceTime visits.
Wellstar held systemwide Nurses Week award celebrations, events, and activities to congratulate honorees and thank Wellstar team members for their dedication and resiliency throughout the pandemic. The Wellstar Nursing Excellence Awards spotlighted nurses at each hospital nominated by their peers for elevating the field of nursing and enhancing the health and well-being of patients. Employees also shared “Videos of Gratitude” showing appreciation for fellow team members.
Three Wellstar team members were also announced as finalists in Atlanta Business Chronicle’s 2021 “Healthcare Heroes” Awards, including two in the Nurse category and one in the Community Outreach category. The finalists are Vicky Hogue (chief nursing officer, Wellstar Paulding Hospital), Nadine Lynch (ICU unit manager, Wellstar Kennestone Hospital) and Dr. Shara Wesley (assistant vice president, Community Health and Wellstar Center for Health Equity). The awards acknowledge “the outstanding work on the frontlines” of the COVID-19 pandemic during an “exceptional year,” and winners will be announced on May 28.
Wellstar Announces “Healthcare Heroes” Award Finalists
During National Nurses Week, Wellstar Health System is celebrating three finalists in Atlanta Business Chronicle’s 2021 “Healthcare Heroes” Awards, including two in the Nurse category and one in the Community Outreach category. The awards acknowledge “the outstanding work on the frontlines” of the COVID-19 pandemic during an “exceptional year,” and highlight some of the many healthcare professionals who have created positive impact through their leadership.
Nursing professionals are instrumental in providing expert, compassionate care, no matter the medical circumstance. The 7,300 nurses at Wellstar are valued and vital caregivers for patients, communities, families, and each other, which has been pivotal to navigating the pandemic.
Two of the three finalists in the Nurse category are Wellstar nursing professionals:
• Vicky Hogue, chief nursing officer, Wellstar Paulding Hospital. Hogue’s background as a critical care and ICU nurse has been instrumental in serving as a leader throughout the pandemic and across her 41-year career. Her leadership is noteworthy and marked by Wellstar Paulding Hospital’s recent recognition as a recipient of the prestigious Malcolm Baldrige Award for performance excellence.
• Nadine Lynch, ICU unit manager, Wellstar Kennestone Hospital. Lynch cares for some of the sickest patients who need extracorporeal membrane oxygenation (ECMO) treatment for vital blood oxygenation, along with many of the facility’s COVID-19 patients. She knows it’s important to focus on more than just the medical care they need, which is why she is always considering ways to ignite her patients’ passions to meet their mental and emotional needs, which aids the healing process.
Both of these nurse leaders have emphasized that close teamwork and collaboration have helped them to achieve positive impact at Wellstar, with people at the center of everything they do.
The Wellstar finalist in the Community Outreach category is:
• Dr. Shara Wesley, assistant vice president, Community Health and Wellstar Center for Health Equity (WCHE). As a convener of thought leaders, community advocates, and action drivers, Wesley has demonstrated over a distinguished career her commitment to public and community health in nearly every facet of the industry.

The WCHE – an extension of Wellstar’s long history of community engagement and allyship to provide people-centric care – was formed under her leadership to drive lasting change at a grassroots level through activating strategic partnerships with government agencies, businesses, philanthropies, non-profit organizations, academia, and citizens.
Qualifications for the awards are that “the nominee must be: employed in the healthcare industry; based in metro Atlanta; and have at least one year in the nominated position or role, and with the same company.” Finalists were selected from nominations for healthcare professionals across Metro Atlanta that highlighted stories of outstanding work with “passion, expertise, and patient care” over the past year. Entries were judged by a panel of editorial staff members from Atlanta Business Chronicle. Winners of the “Health Care Heroes” awards will be announced and featured in a special section of Atlanta Business Chronicle on May 28.
Last month, Great Place to Work® and Fortune honored Wellstar Health System as one of the 100 Best Companies to Work For®, Wellstar’s fourth time on this prestigious list of the best companies to work for in the nation. Wellstar is the only Georgia-based healthcare company included in the 2021 ranking; only two other companies headquartered in Georgia were included in this year’s list.

Wellstar Leads New, Life-Saving Treatment for Ischemic Strokes
When it comes to strokes, seconds can mean the difference between life, death and lasting damage. That’s why Wellstar Health System is dedicated to developing faster, more effective stroke treatments not just for Georgians, but people across the nation.
Wellstar Director of Stroke & Neurocritical Care Dr. Rishi Gupta helped test a groundbreaking device to treat complex ischemic strokes, working alongside UCLA’s Dr. Jeffrey Saver and device manufacturer Rapid Medical.
During a two-year period, patients in 16 medical centers across the country were enrolled in a clinical trial to develop the state-of-the-art stroke treatment, with Wellstar registering the highest number of participants.
Dr. Gupta’s efforts will have a profound impact on stroke treatment moving forward, as Wellstar continues to lead the pack when it comes to neuro care.
“Wellstar is on the cutting-edge of many new stroke technologies and therapies, through our participation in groundbreaking clinical trials,” Dr. Gupta explained. “Our research not only brings patients in Georgia the most advanced stroke treatments close to home, but can help save more lives across the country.”
Now, neurointerventionalists nationwide will have access to the new, FDA-approved technology called TIGERTRIEVER™ to help stop strokes faster and improve patient outcomes.

Types of Stroke
For many people, the warning signs of a stroke—like numbness in the arm, confusion, loss of balance or trouble speaking and seeing—are unmistakable. But often, the underlying cause of these life-threatening medical events can be harder to uncover.
“Strokes are complicated because there’s no pain associated with it,” said Dr. Rishi Gupta, director of stroke care with Wellstar Health System. “Many people think they can sleep it off and they’ll be better in the morning.”
“However, if you are experiencing the signs of a stroke, the faster you get to the emergency room, the more likely it is that we can reverse disability.”
While the telltale symptoms may be similar to one another, all strokes are not alike.
At Wellstar, we know each and every stroke is different. That’s why our neuro team provides tailored care along with fast, life-saving treatment for all types of strokes, even the most complex cases.
Fight back against strokes and learn the difference between the three main types: ischemic, hemorrhagic and transient ischemic attack.

New Wellstar Health System Initiative Strives to Improve Outcomes for Patients with Pulmonary Embolisms
When a patient has a pulmonary embolism, it’s crucial that they receive the right care, right away. A new team of experts at Wellstar brings together specialists from several disciplines to collaborate on care, quickly and accurately assessing patients and formalizing a personalized treatment plan.
The Pulmonary Embolism Response Team (PERT), implemented systemwide at Wellstar, ensures that all our patients receive timely treatment for this serious condition. Pulmonary embolisms, or blood clots in the lung’s arteries, are the third leading cause of death among hospitalized people and the third most common cardiovascular cause of death. With this new initiative, patients have an entire care team dedicated to fighting those statistics.
The PERT includes interventional cardiologists, critical care specialists, pulmonary experts, emergency medicine physicians and hematologists, who look at the patient’s case from multiple perspectives.
“In emergencies like pulmonary embolism, time is of the essence in treating this potentially fatal condition,” said Dr. Salvatore Mannino, Medical Director of Invasive and Interventional Cardiology for Wellstar. “With our new multi-disciplinary, multi-hospital team, several specialists can weigh in at once, speeding up treatment and making sure the patient receives the treatment that will lead to the best outcome.”
If a patient needs to be transferred to another facility for treatment, Wellstar makes that transition seamless, with providers efficiently communicating between hospitals about the patient’s personalized care plan.
Learn more about how Wellstar’s cardiovascular providers can keep you healthy at wellstar.org/heartcare. To make an appointment, call (770) 956-STAR.

Get Care Anywhere with Wellstar Virtual Care
These days, people can connect with friends online or join a virtual business meeting with just a click of a button. So, why not make your next doctor’s appointment just as easy?
With Wellstar Virtual Care, you can visit your Wellstar physician, remotely – from the comfort and convenience of home. All you need is a smartphone, computer or tablet to stay connected with your provider.
From getting wellness exams to managing chronic conditions, Wellstar Virtual Care gives you the flexibility to find safe, expert care anywhere.

Wellstar Addresses Persistent Health Inequities
The system continues to build on its legacy and commitment to serving communities by actively listening to best understand and respond to what consumers want, need, and expect from their healthcare provider.
“As a leader in healthcare, we must take action to meet the evolving needs of people and communities. Health equity connects to everything we do, and recognizing hardships, disparities, and inequities is just the first step,” said Candice L. Saunders, president and CEO of Wellstar Health System. “Through strategic partnerships and programs, Wellstar is committed to supporting people and communities to make a tangible and lasting difference, enhancing the health and well-being of everyone we serve.”
The Wellstar Center for Health Equity (WCHE) – an extension of Wellstar’s long history of community engagement and allyship to provide people-centric care – was formed to drive lasting change at a grassroots level. The six areas of focus were informed by Wellstar’s triennial Community Health Needs Assessment (CHNA) of 2019: Primary Care, Behavioral Health, Food Insecurity, Suicide, Cancer, Women’s Health.
Each of these strategic domains connects to Wellstar medical service lines to bring to bear the deep expertise and broad bench of resources needed to identify pertinent needs, relevant partnerships, and viable programs.
To create meaningful impact, Wellstar has forged strategic partnerships with government agencies, businesses, philanthropies, non-profit organizations, academia, and citizens. Examples of how WCHE has activated resources in the community include:
Walk-up, pop-up family COVID-19 testing: With the support of community partners, Wellstar conducts free walk-up, pop-up family testing at churches and school lunch pick-up sites and distributes safety kits in English and Spanish. To-date, WCHE has orchestrated 29 pop-up testing sites, administered over 3,000 COVID tests, and distributed more than 51,000 wellness kits with culturally and linguistically appropriate safety information.
Reaching faith-based congregants with vital information and vaccines: WCHE is hosting a series of community town halls to debunk myths about COVID-19 and vaccines in partnership with the Wellstar Congregational Health Network. In April, WCHE hosted a Hispanic town hall to address community questions and launched a series of equity-centric and language-proficient vaccination clinics for congregants at faith-based organizations.
Providing nutritious meals to food-insecure communities: In partnership with Goodr, an organization that provides food resources for people in need, and funded in part by Wellstar Foundation donations, the WCHE “Mobile Market” hosts “pop-up” farmers’ markets in seven communities, feeding over 700 families monthly.
Enabling technology-driven community health transformation: WCHE launched a year-long initiative to enhance access to medical care via technology with leading community partners. Supported by contributions to the Wellstar Foundation, the “Community Health Transformation” program enables the following community organizations to reach, engage, and support at-risk individuals with measurable results: Bethesda Community Clinic; Empowerment Resource Center; Healthy Mothers, Healthy Babies Coalition of Georgia; Good Samaritan Health Center of Cobb; and MUST Ministries.
Anchoring vulnerable patients with vital healthcare resources: When the Centers for Disease Control and Prevention (CDC) reported that 80% of COVID-19 patients in eight Georgia areas were Black people, WCHE developed “Anchoring Vulnerable Patients,” a project in Clayton County to assess and address the medical and social needs of Black patients with co-morbidities that put them at risk for contracting COVID-19.

#MyWhy: Wellstar Leaders Share Why They Stuck It to COVID
For more than a year, our communities have done their part to fight COVID-19.
We have stayed home, worn masks when we’ve gone out, been extra careful with washing our hands and avoided large gatherings. That’s meant that holidays and birthdays have looked a little different, all so we can stay safe and healthy.
The separation and fear have been draining, and many of us have dealt with loneliness and stress as we worry about our health and our loved ones.
But now we have something to celebrate. Hope has arrived in the form of the COVID-19 vaccine. All Georgians age 12 or older are now eligible to get their shots.
At Wellstar, we've chosen to lead by example. Across our health system, frontline healthcare workers and leadership have "stuck it to COVID." Whether they want to gather with friends and family, travel to a new destination or help protect vulnerable members of the community, our Wellstar team members all have their #MyWhy — the reason they chose to get vaccinated.
For Dr. Jeffrey Hines, chief of gynecologic oncology for Wellstar, getting the shot was about a sense of responsibility. As medical director of the Wellstar Center for Health Equity, Dr. Hines works to ensure our underserved populations have access to the care they need to stay safe and healthy. He got the COVID-19 vaccine to protect those around him.
“I’m a father, I’m a husband, I’m a brother and I’m a grandfather, and it’s important for me to protect my family,” Dr. Hines said. “I understand the science, and the science is important, but equally important to me is I want to be a trusted voice to people in the community who are most at risk for this and perhaps may have the most questions.”
Dr. Sophia McIntyre, senior vice president of Wellstar Medical Group, also said she got her shot to stop the spread, noting that COVID-19 has disproportionately affected minority communities.
“The reason why I got the COVID-19 vaccine is to ensure that I’m doing my part to bend the curve,” Dr. McIntyre said. “We know that African Americans and Latino Americans are dying at a higher proportion.”
Dr. Danny Branstetter, Wellstar’s medical director for infection prevention, has been at the forefront of Wellstar’s work to fight COVID-19 and keep our communities safe. Now, he wants to see life return to normal, because health isn’t just about your body. It’s also about your personal connections and overall well-being.
“I’m tired of being separated from my friends and family. I’m tired of seeing small businesses fold,” Dr. Branstetter said. “I’m tired of seeing the increased burden this places on those without resources. I’m tired of the loneliness this puts on those who are isolated and the elderly. My question is, aren’t you tired, too?”
All of us play a part in ending this pandemic.
“We’re in this together, and we can end this together through vaccination,” Dr. Branstetter said.
To find a vaccination site near you, visit the Georgia Department of Public Health website or local retail pharmacy.

Defeating Pain with Successful Spine Surgeries at Wellstar
Barbara Deans was worried she would never walk again — until she went to Wellstar.
She had a herniated disc on her sciatic nerve, along with degenerative disease, which is one of the most common causes of back and neck pain. She had tried epidurals and other treatments without much improvement, and it got to the point where she couldn’t walk without taking heavy pain medication.
But Barbara was determined to stay mobile. She turned to Dr. Marcus Gates, a neurosurgeon at Wellstar Cobb Hospital, about her next steps. Barbara was a little hesitant about surgery, but after getting to know Dr. Gates and discussing her treatment options, she felt confident about conquering her pain.
“Dr. Gates made me feel comfortable,” Barbara said. “He explained all the details of the surgery, such as how long the incision would be and how long it would take. He has a great bedside manner.”
For Dr. Gates, surgery is about more than the procedure — it’s about the person and how he can help them live a fulfilling life.
“Everything is tailored to the patient. It's customized care,” Dr. Gates said. “So what I'm trying to do is listen to the patient, figure out what exactly they need and try to provide that care as efficiently as possible.”
Barbara said Dr. Gates helped ease her fears about surgery and envision her life without pain.
“Dr. Gates told me I would walk out of the hospital after surgery,” she said. “He inspired me, and I believed him.”Barbara was back to doing her usual activities the same day of the minimally invasive surgery.
To learn more about how you can find success through spine surgery and find a solution for your pain, make an appointment with Dr. Gates in Austell or Smyrna at (470) 956-4410.

Barbara Deans

Take Action Against Strokes
A stroke can happen to anyone, anywhere and at any time. In fact, every four minutes someone in the United States experiences a stroke, according to the Centers for Disease Control and Prevention (CDC).
During Stroke Awareness Month this May, Wellstar health experts are spreading the word about how they’re helping Georgians can stay ahead of these life-threatening medical events.
“Because we live in the stroke belt here in Georgia, it is imperative we provide cutting-edge care for stroke victims,” said Dr. Rishi Gupta, director of stroke and neurocritical care with Wellstar Health System. “Wellstar’s ability to leverage our hospitals to work as one, cohesive unit and provide the same quality of care across the board really sets our health system apart.”
With the largest Joint Commission stroke-certified network in Georgia and access to advanced stroke care, Wellstar is dedicated to treating strokes faster and more effectively. But while we’re always ready to jump into action with life-saving treatments, stopping a stroke starts with you.
Do your part to lower the risk of a stroke and learn the warning signs that may help save a life.

Wellstar Partners with Northwest Georgia Oncology Centers for Collaborative Care
A cancer diagnosis can be unexpected and scary for both patients and their loved ones. But at Wellstar, we know the key to fighting cancer lies in a collaborative team approach.
That’s why we’ve partnered with Northwest Georgia Oncology Centers (NGOC) to bring the highest level of expert cancer care to Georgia. Here, you will have a multidisciplinary team by your side — an entire group of experts who will take the time to get to know you and will help you face cancer with confidence.
“We’re there for our patients, to come up with their cancer plan, to get them through that, but we also follow them, oftentimes for 5 years or 10 years, to make sure that their cancer doesn’t come back,” said Dr. Michael Andrews, chief cancer officer at Wellstar. “It can be a very rewarding and close relationship.”
NGOC is a team of board-certified medical oncologists and hematologists passionate about fighting for each patient. They are leaders and innovators in community-based cancer care and focus on creating the best outcomes for each patient.
And with convenient locations all throughout metro Atlanta, you can get the care you need without the added stress of travel.

Wellstar Health System Celebrates Accolades
Wellstar Health System, one of the largest healthcare systems in Georgia, announces multiple accolades, including national, regional and local recognition for facilities, service lines and leaders. Awards and accreditations for quality, safety, performance excellence and community service exemplify Wellstar’s commitment to world-class healthcare.
“Dedication to excellence is a hallmark of Wellstar,” said David Jones, executive vice president and chief human resources officer of Wellstar. “People are at the center of everything we do. Achieving these accolades is a testament to our team’s hard work to enhance the health and well-being of every person, every time. It is not only our mission—it is our calling and our honor to offer tailored, compassionate healthcare to the people we serve.”

How People Benefit from Remarkable Robotics at Wellstar
Thanks to high precision instruments and tiny incisions, robotic-assisted surgeons give people a chance to have better outcomes—such as less recovery pain, fewer complications and shorter hospital stays, or for some outpatient procedures, no hospital stay at all.
“We offer patients the best-in-class robotic surgical services, spanning from cancer and cardiothoracic procedures to highly coordinated bariatric robotic surgery—and everything in between,” said Dr. Scott Miller, a Wellstar urologist in North Fulton.
Wellstar has grown to house 14 state-of-the-art da Vinci robotic surgical systems at several of our hospitals and two outpatient surgery centers.
Because of the remarkable demand for robotics and the comprehensive offerings of the program, Wellstar recently named Dr. Miller the Director of Robotic Surgical Services. In his role, he ensures best practices are followed to deliver consistent, high-quality robotic procedures across all Wellstar locations.
Robotic surgery allows physicians to do complex surgeries with smaller incisions, less pain and less risk of infection.
For example, the length-of-stay in the hospital for a patient who has a an open colon resection is typically around a week versus just 1 ½ to 2 ½ days for a patient who has the same procedure performed by a surgeon with the assistance of a robotic surgical system.
Less tissue manipulation limits how much the tissues are altered and how long body processes go uninterrupted, which enables patients to have quicker recoveries and get back to their lives faster.

Keep Your Seasonal Allergies Under Control
As the weather starts to warm and flowers bloom, spring is in the air – and so is pollen.
If you deal with frustrating symptoms like a stuffy nose, sneezing or watery eyes, you’re not alone. Each year, more than 50 million people in the United States have allergies, according to the Asthma and Allergy Foundation of America.
Wellstar knows every Achoo! can impact your daily life, making it difficult to enjoy outside activities with family and friends. Instead of sitting on the sidelines, you can use simple strategies to take control of your seasonal allergies.
Seasonal allergies are your immune system’s response to certain environmental triggers, such as pollen from trees, grass or flowers. Your body’s reaction to these allergens can include coughing, sneezing, runny nose, red or itchy eyes, throat irritation and post-nasal drip.
By playing it smart and planning ahead, you can take steps to relieve your allergy symptoms. Follow the helpful tips below to say goodbye to seasonal allergies:
• Masks make a cool accessory. Wearing a mask can not only keep others safe from COVID-19, but also prevent you from breathing in pollen and other allergens.
• Try over-the-counter medications. Consult your Wellstar provider about common allergy remedies like antihistamines and nasal spray.
• Check the weather report. Avoid outside activities on days that are dry, windy or have a high pollen count of 1,000 or more.
• Don’t invite allergens inside. Keep windows and doors shut to prevent pollen from blowing into your home and contaminating surfaces.
• Stay on top of spring cleaning. Dust and vacuum often to remove potential allergens, such as dust, dander and pollen.
• Don’t forget your four-legged friends. Be sure to wash or brush your pets more often to remove loose fur and dander.
When at-home remedies aren’t enough, Wellstar Allergy & Immunology is ready to care for you. If your symptoms are severe, you may need specialized treatment for allergies or be dealing with a chronic condition, such as asthma.
At Wellstar, we diagnose and treat a full range of adult and pediatric allergy conditions. Our allergists will partner with you to create a personalized care plan, which may include allergy shots, prescription medication or other therapies.
Don’t sneeze or sniffle through another season. Wellstar provides the world-class, tailored allergy care you need at convenient locations across metro Atlanta.
Click the “Book Now” button at the top of any page to schedule an appointment.

Wellstar Kennestone Hospital Wins Best in Real Estate Award

Wellstar named Great Place to Work® & Fortune 100 Best Companies to Work For®
Wellstar Health System is recognized as one of the best companies to work for in the country for the fourth time; People-centric programs, benefits, and culture foster an inclusive, team-based workplace
Great Place to Work® and Fortune have honored Wellstar Health System, one of the largest and most integrated healthcare systems in Georgia, as one of the 100 Best Companies to Work For®. This is Wellstar’s fourth time on this prestigious, national list. Wellstar is the only Georgia-based healthcare company included in the 2021 ranking; only two other companies headquartered in Georgia were included in this year’s list.
“In a year of immeasurable challenges, our Wellstar team members and caregivers have remained focused on our mission to enhance the health and well-being of everyone we serve,” said Candice L. Saunders, president and CEO, Wellstar Health System. “Earning the 100 Best Companies to Work For award is a testament to their bravery and unwavering commitment to providing people-centric care for millions of Georgians.”
The Fortune 100 Best Companies to Work For® award is based on analysis of survey responses from more than half a million current employees across the U.S. In that survey, 79% of Wellstar’s employees said Wellstar is a great place to work. By comparison, the average percentage of employees in the U.S. who say their company is a great place to work is only 59%.
"Offering the resources, support, and workplace culture team members need to be their best benefits everyone and everything we do,” said David Jones, executive vice president and chief human resources officer, Wellstar Health System. “We care for our employees so they can care for our community. We are grateful for the recognition from Fortune and, especially, for the all the people who make Wellstar a great place to work.”

Preventing Cancer with Wellstar’s Genetics Experts
While Wellstar’s expert cancer specialists are well-equipped to help their patients fight cancer, they’re also dedicated to stopping cancer before it starts.
Part of preventing cancer is knowing your risk and taking action early. Wellstar’s Genetic Risk Assessment Program helps patients determine whether they may be at higher risk for some cancers.
At Wellstar, our focus is PeopleCare—personalized healthcare tailored just for you. For cancer care, that means taking a close look at what makes you unique—your distinct genetic makeup that sets you apart. Genetic counselors use a compassionate approach to guide patients and their families so they can make informed healthcare decisions.
“We are the busiest genetic counseling program in Georgia,” said Wellstar's Chief Cancer Officer, Dr. Michael Andrews. “Cancer care now is very genetically-based, and the specialists in our program can look for certain abnormalities and adapt treatments based on what they find.”
Genetic mutations play a major role in about 5–10% of cancers. A patient with a family history of cancer who learns they have specific genetic mutations can partner with their provider to be more proactive, whether that involves screening, lifestyle changes or medical treatments. Taking a few proactive steps could prevent cancer, even if the patient’s genetics may put them at a higher risk.
Genetic testing can also benefit cancer patients and empower their whole families with important information. If a cancer patient learns they carry a mutation, it can help relatives decide if they could benefit from genetic testing. Also, people who have certain cancers and also have specific DNA sequences may benefit from targeted therapies.
Some possible signs of hereditary cancer include:
Some gene mutations can increase your cancer risk, so if your provider finds that you are affected, they may recommend increased screenings and other precautions to monitor your health.
Take charge of your health—and maybe help out a family member, too—by learning more about how your genetics could affect your cancer risk. Call (470) 793-7472 to book an appointment with a Wellstar Genetic Counselor. Both in-person and virtual visits are available. Learn more at wellstar.org/cancercare.
Delta Sigma Theta, Inc. National President and CEO, Members Get COVID-19 Vaccine at Wellstar
Wellstar and Delta Sigma Theta, Inc., the largest African American women's organization in the world with more than 350,000 college-educated members, have united to reach vaccine-reticent populations in Georgia by sharing personal “My Why” stories and reasons for receiving the COVID-19 vaccine.
Who: Beverly E. Smith, national president and CEO of Delta Sigma Theta Sorority, Inc., joined Wellstar team members in sharing a personal reflection about receiving the COVID-19 vaccine. A recent poll found that Black voters in Georgia are less sure about vaccine safety than another racial or ethnic group, with 36 percent reporting that they are unsure if the vaccine is safe or not. The video aims to tackle these concerns and offer hope for the future as more Georgians become fully vaccinated. Delta Sigma Theta Sorority Inc. national president and CEO, Beverly E. Smith, joins Wellstar team members in sharing a personal reflection about receiving the COVID-19 vaccine.

CindyCare
To say Cindy Mejia is “busy” is an understatement.
She’s constantly crunching numbers as an accounting manager for a large research institute, trying out new recipes in her kitchen at her Roswell home, or trying to keep up with her little granddaughter (who just discovered how much fun it is to run).
But one Wednesday in September, Cindy woke up and reached for her computer, trying to get an early start to her workday. She felt a little groggy and couldn’t remember her password but didn’t immediately realize something was wrong.
Then she stood up. Her right arm and leg weren’t functioning, and that’s when Cindy knew what was happening—she was having a stroke.
“The first thing I thought was, ‘I need to get to Wellstar North Fulton right away,’” Cindy said. “I knew the hospital was nearby and has a good reputation.”
That decision ultimately saved her brain and life.
For Cindy, the critical care she needed was close to home, too—she lives four miles from Wellstar North Fulton Medical Center. There, her care team sprang into action, bringing her the treatment and peace of mind in a moment of crisis.
“From then on, I felt well taken care of,” Cindy said. “I was relieved, and I knew I was going to be OK.”
When a patient has a stroke, every second matters. Each minute that ticks by could be the difference between a permanent stroke and a return to routine. So at North Fulton, Cindy’s care team assembled quickly to save her brainpower.
“We’re like the pit crew on a NASCAR team,” said Dr. Ed Malcom, an emergency medicine physician at Wellstar North Fulton. “We have our emergency stroke care response down to a science. Everyone knows their role and works together to act quickly.”
Cindy was one of the first patients at Wellstar North Fulton to benefit from the hospital’s new addition to its stroke program. While the hospital has been a primary stroke center for years, the introduction of thrombectomies at the hospital gives patients a close-to-home, life-saving option for stroke care—saving them both time and brainpower.
A thrombectomy is a minimally invasive procedure used to unclog an artery, restoring blood flow to the brain and preventing further damage. It does not involve cutting of the brain but instead starts with the insertion of a catheter through the patient’s groin.
“Recently, we’ve developed our own capability right here in the North Fulton area to pull the clot out of the brain. That’s a giant leap forward,” Dr. Malcom explained. “It's good for the whole state because there's only a handful of hospitals that do that, and it's good for the residents that live in that North Fulton area to have a hospital so close. They don't have to take a helicopter ride somewhere to get that procedure done. It saves time.”
For Cindy, having that procedure just a few miles from her home, right when she needed it, helped save her brain function.
“If Cindy would have gone to a different hospital that didn't provide this care, then it would have been a long time before she was able to have blood flow restored to the brain,” Wellstar Neurosurgeon Dr. Benjamin Zussman said, explaining how critical each section was when it came to Cindy’s care. “The delay could have been 30 minutes or even an hour, and it's possible that she would have had permanent stroke, permanent damage to her brain instead of making the recovery she did.”
Offering thrombectomies at Wellstar North Fulton has brought long-needed stroke services to the area north of Atlanta, so patients like Cindy don’t have to travel into the city through busy traffic to get the treatment they need.
Proximity to care is especially important for critical situations like strokes, said Dr. Rishi Gupta, director of stroke care at Wellstar.
“Any disease that is time-sensitive where patients need to get to the hospital quickly, get treated quickly—the geography is everything, particularly in bad weather when helicopters cannot fly,” he said, explaining how logistics can impact life-saving stroke care. “We need to be able to provide services in the communities the patients reside and the North Fulton program is uniquely positioned to do that.”
Signs of a stroke can include a loss of balance, dizziness, blurry vision or sudden vision loss, drooping in the face, arm or leg weakness, and difficulty speaking. Patients who experience any of those symptoms should call 911 and seek medical care right away.
Cindy said she is glad she got to the hospital as soon as she could—“I am so thankful that I took quick action and that I had Wellstar so close.” At Wellstar North Fulton, she not only received the highest level of stroke care. Wellstar takes a multidisciplinary approach to stroke care, including specialists such as critical care specialists, neurologists, neurointerventionalists and physical therapists on the care team.
“When you're feeling pretty healthy, you don't think a stroke can happen to you. It happens so quickly. You don't necessarily get a warning,” Cindy said, sharing the importance of listening to your body’s signals when it comes to health. “You can feel one way one day or one minute, and the next minute, it changes.”

Wellstar Partners with Morehouse School of Medicine to Support At-Risk Populations
Responding to vital needs among vulnerable communities during the pandemic, Wellstar is the first Georgia-based health system to become a national partner in new initiative
Wellstar Health System has joined Morehouse School of Medicine (MSM)’s National COVID-19 Resiliency Network (NCRN) of partners to further inform community-driven response, recovery, and resiliency strategies for addressing the impact of COVID-19 on communities.
In response to the needs of at-risk communities across the health system’s service areas, Wellstar has partnered with the MSM-NCRN and its 40 network partners across the U.S. to collaborate on offering COVID-19-related services to disproportionately impacted communities. As a not-for-profit system dedicated to providing “More than Healthcare. PeopleCare.” Wellstar is committed to addressing inequities that impact the health and well-being of people and communities through more than 450 community partnerships, Wellstar Community Health initiatives, and activities led by the Wellstar Center for Health Equity (WCHE).
One of the most critical barriers to health during the pandemic has been consumer access to reliable, science-based, culturally appropriate, and native language information resources, which the partnership will facilitate. Wellstar is the first Georgia-based health system to become a national partner in this important, new initiative.
“Wellstar is pleased to partner with Morehouse School of Medicine to provide vital information and resources for at-risk communities,” said Candice L. Saunders, president and CEO, Wellstar Health System. “The NCRN is a strong complement to the important work that our Wellstar Center for Health Equity is doing, and we are thankful for the collaboration.”
Morehouse School of Medicine’s National COVID-19 Resiliency Network Builds Community Resiliency
The MSM-NCRN coordinates a strategic and structured national network of national, state/territorial/tribal and local public and community-based organizations that, together, will work to mitigate the impact of COVID-19 on racial and ethnic minority and rural populations. The network helps to provide awareness of culturally appropriate health education information and linkage to care, helping organizations and families recover from pandemic difficulties. In addition to educational and informational resources in at least 10 languages to accommodate cultural competency, initiatives will include COVID-19 testing, vaccinations following phases directed by DPH, training opportunities for community leaders.
“Our national network connects individuals, families, community organizations and clinical providers to timely and relevant COVID-19 information and services in their neighborhood,” says Dominic Mack, MD, MBA, professor of family medicine and director of the National COVID-19 Resiliency Network in the National Center for Primary Care at MSM.
“Morehouse School of Medicine’s National COVID-19 Resiliency Network is designed to not only provide structure to the resources that are on the ground-level fighting this pandemic but is an important resource for our partners in serving the underserved and getting people the healthcare they need,” said Valerie Montgomery Rice, MD., MSM president and dean. “Organizations such as Wellstar here in Georgia, its Wellstar Center for Health Equity, and the partnerships we cultivate, are critically important to the mission of health equity and in fighting and defeating COVID-19.”
Wellstar Center for Health Equity Addresses Health Inequities across Georgia
The WCHE addresses health inequities across Georgia to enhance the health and well-being of the people and communities served by Wellstar. Through partnerships such as the one with MSM-NCRN, the WCHE implements multi-disciplinary approaches to address deeply entrenched social disparities and healthcare gaps. Programs led by the WCHE over the past year include walk-up, pop-up COVID-19 family testing; distribution of masks and safety kits to at-risk communities; Congregational Health Network communications, collaboration, information, and support; Spanish-language educational information for Latinx communities; a technology-driven Community Transformation initiative for local non-profits; joint Webinars on health equity topics in collaboration with Partnership for Southern Equity, Atlanta Regional Collaborative for Health Improvement (ARCHI), and Georgia Health Policy Center; and a series of “Mobile Market” free farmer’s market-style grocery shopping experiences for hundreds of families with Goodr.
The partnership between Wellstar and MSM-NCRN will extend the organizations’ reach and resources to enhance information access and drive positive impact.
The NCRN launch follows a $40 million award from the U.S. Department of Health and Human Services Office of Minority Health to coordinate a strategic network focused on delivering COVID-19-related information to communities hardest hit by the pandemic. The launch of the NCRN occurs alongside the release of new digital technology accessible through the NCRN website. It provides location-based recommendations on where community members can get a COVID-19 test or receive a COVID-19 vaccine when distribution increases in the coming months.
Learn more about our COVID-19 vaccine updates. To access MSM-NCRN COVID-19 resources, visit www.msm.edu/ncrn.

ValerieCare: Spine surgery success at Wellstar North Fulton Hospital
Valerie Orff was done with excruciating pain.
After suffering with severe back aches for 30 years, the Roswell resident had tried everything. Massage therapy, chiropractic care and even dry needling. But nothing provided permanent relief — until she went to Wellstar.
When Valerie’s pain, which had been steadily worsening over the past eight years, got to the point where she couldn’t play soccer with her grandchild, dance or sit on a motorcycle (one of her favorite past times), she told her primary care physician she needed a true solution. That’s when Wellstar stepped in.
Dr. Basheer Shakir, a neurosurgeon at Wellstar North Fulton Hospital, carefully and thoroughly examined Valerie and discovered what had been bringing her discomfort and slowing her down — a disc in her back was degenerating, and one of her vertebrae was moving back and forth on another one, instead of staying in place.
“This was causing back and leg pain that affected her daily activities and quality of life,” Dr. Shakir said.
Dr. Shakir knew Valerie was hesitant about getting surgery. But after spending time getting to know Valerie, and learning about her busy, active lifestyle, the two decided on a minimally invasive surgery that could quickly get her back to her routine.
Valerie’s Wellstar team was able to perform a fusion operation by accessing the disc through her side, without traumatizing the muscles in her back. This shortened her hospital stay, minimized her pain after surgery and accelerated her recovery.
Although she had initially been nervous about spine surgery, Valerie said Dr. Shakir listened to her concerns, presented all her options and explained everything in detail so she knew what to expect. In short, he treated her as much more than just a “neuro patient,” but as a person.
Now, 12 weeks after surgery, Valerie is pain-free for the first time in three decades.
“I put my faith and trust in him, and now I can’t even tell you how good it is to get up every day and go to bed with no back aches. I sleep through the night, go to the gym and lost 15 pounds,” she said.
If you are struggling with back pain, Wellstar’s expert neurosurgeons and orthopedic surgeons can help you decide if spine surgery is right for you.

Wellstar Hires Chief Information and Digital Officer
Physician leader and digital healthcare strategist Hank Capps, MD, to drive next-generation healthcare delivery strategy for leading health system.
Wellstar has hired Hank Capps, MD, as executive vice president and chief information and digital officer. In his role, Dr. Capps will be responsible for advancing the system’s digital strategy to reimagine and enhance the consumer healthcare journey and experience, while evolving and optimizing the not-for-profit company’s operational technology-based platforms, processes, and partnerships.
Dr. Capps joins Wellstar after more than 18 years with Novant Health in North Carolina, where he held a series of clinical and administrative roles as an executive leader. His proven skills and expertise as an accomplished operator and digital healthcare strategist will further equip Wellstar to leverage advanced technology to transform healthcare with deeper patient engagement and consumer control.
“At Wellstar, we put people at the center of everything we do, and that includes our digital strategy,” said Candice L. Saunders, president and CEO, Wellstar Health System. “As both healthcare delivery and technology continue to evolve at a rapid pace, Wellstar is focused on how to accelerate and leverage the intersection of these two industries to improve patient care and outcomes. Dr. Capps is the experienced and visionary leader we need to define the path forward for our system and the communities we serve.”
The global COVID-19 pandemic has triggered an unprecedented shift in the healthcare industry, resulting in consumer and provider demand for next-generation care and tools. Dr. Capps will head a team of technology and digital healthcare experts to identify gaps and opportunities in healthcare delivery and consumer engagement to create innovative, world-class solutions that fulfill this expectation.
“Wellstar’s industry leadership in healthcare excellence is grounded in continually and intentionally enhancing both the patient and provider experience,” said Dr. Capps. “The pandemic has impacted the dynamic of that consumer journey, accelerating technology adoption and exacerbating the need for creative solutions that enable access to quality care. I am thankful for the opportunity to be part of the Wellstar team as we leverage emerging technology and innovative thinking to transform the future of healthcare.”

Wellstar Center For Health Equity Event To Answer Questions About COVID-19 Vaccines
The Wellstar Center for Health Equity will host a Virtual Town Hall this Thursday, March 4, at 6:30 p.m. to address community questions about COVID-19 and vaccines. To register, visit wellstar.org/townhall
Marietta, Ga. (MARCH 2, 2021) — Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, is hosting a Wellstar Center for Health Equity Virtual Town Hall with its Congregational Health Network this week.
What: The event, held in collaboration with the Wellstar Congregational Health Network, Morehouse School of Medicine National COVID-19 Resiliency Network (MSM-NCRN), and Atlanta Regional Collaborative for Health Improvement (ARCHI), will address pertinent questions about COVID-19 and vaccines with faith communities across Georgia. The 90-minute event will feature a panel of healthcare experts, including Wellstar and Morehouse School of Medicine physicians, who will address questions provided by the community in advance of and during the event, including the latest information and resources to combat COVID-19.
When: The Virtual Town Hall will be held via Zoom on Thursday, March 4, at 6:30 p.m. and will offer participants the opportunity to ask questions and get answers from healthcare experts who are dedicated to community education and outreach. Faith leaders and congregation members are invited to register at wellstar.org/townhall.
Panel: The panel of experts will include Dr. Tabia Henry Akintobi, Morehouse School of Medicine; Dr. Jeffrey Hines, Wellstar Center for Health Equity; and Dr. Zandraetta Tims-Cook, Wellstar Medical Group.
ABOUT WELLSTAR HEALTH SYSTEM
At Wellstar, people are at the center of everything we do. By listening actively to what people want, need and expect from their healthcare, Wellstar is able to provide “More than Healthcare. PeopleCare.” — at every age and stage. Nationally ranked and locally recognized for our personal, high-quality care, inclusive culture, and exceptional doctors and team members, Wellstar provides access to compassionate, high-quality care through our: 11 hospitals; 300+ medical office locations; 9 cancer centers; 74 rehabilitation centers; 3 hospice facilities; 1 retirement village; 29 imaging centers; 16 urgent care locations; and 5 health parks. As one of the largest and most integrated healthcare systems in Georgia, Wellstar is growing our services, footprint, capabilities, and ability to meet evolving patient needs. Our passion for people extends into the communities we serve. As a not-for-profit health system, we thoughtfully reinvest annually in prevention and wellness programs, as well as charity care for eligible patients. Our Wellstar Foundation also supports our mission to enhance the health and well-being of every person we serve with funding for equipment, services, and programs that provide more than healthcare.

Wellstar and Sharecare Partner to Deliver Personalized Health and Wellness Platform
Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, and Sharecare, the digital health company that helps people manage all their health in one place, announced a strategic partnership to collaborate on unique, market-leading innovations in personalized care delivery, population health, and consumer engagement.
“People are at the center of everything we do,” said Candice L. Saunders, president and CEO, Wellstar Health System. “Our partnership with Sharecare was forged to deliver an innovative experience that will engage and empower people in improving their health and wellness in unprecedented ways. Together, we are building on our vision for the healthcare system of the future that empowers the consumer.”
Wellstar will leverage Sharecare’s digital engagement platform and expertise to equip its team members with enhanced resources and health information to take control of their day-to-day well-being. Through this partnership, Wellstar also will become the first “Sharecare-enabled” health system in the country, utilizing Sharecare’s solutions to accelerate the transformation to value-based care and applying resulting insights to optimize, expand, and, ultimately, re-imagine the overall consumer healthcare experience.
Sharecare delivers each person a customized digital experience where they can easily access extensive information, engagement resources, and clinically validated tools to improve their individual health and well-being, no matter where they are in their health journey. In Summer 2021, Wellstar will roll out Sharecare’s award-winning virtual care platform to its 24,000 team members to help them manage their overall physical and mental well-being and navigate related employee benefits, all in one place. In addition to the comprehensive content and resources already available through Sharecare, the two organizations will focus on innovating incentives and rewards administration that tie to engagement and outcomes and capitalize on existing Wellstar workplace well-being strategies and programs, such as employee fitness centers and biometric screening programs.
“Our team members are dedicated to caring for Georgians each and every day,” said Saunders. “That’s why it’s important that we care for them with world-class solutions that equip them to be at their best.”
As the country’s first Sharecare-enabled health system, Wellstar will work with Sharecare to co-develop consumer-facing offerings—available in Georgia through Wellstar exclusively through 2023—to achieve better health outcomes. To accomplish this, Wellstar will integrate its electronic medical record system with the Sharecare platform and utilize the digital health company’s robust portfolio of provider solutions, data management tools, and artificial intelligence capabilities to better identify and close gaps in care. Once a condition or potential care gap is identified, Wellstar providers can “prescribe” patients with additional information, digital therapeutics, and clinical programs through the secure, unified Sharecare platform, where in turn people can access those resources, monitor their progress, and, ultimately, become more engaged in their overall health and well-being.
“In addition to supporting our client partners throughout the pandemic, we have also continued to innovate and make strategic acquisitions—the collective impact of which has yielded new strategic opportunities, including accelerating our ability to bring our vision for the Sharecare-enabled health system to life,” said Jeff Arnold, founder, chairman, and CEO of Sharecare. “The key, however, was finding the right health system partner—one who shared our commitment to not only compassionate, community-driven care but also digital innovation and optimizing patient-clinician encounters through data. As a Georgian, I take pride in the fact that the ideal partner to help us realize this vision is Wellstar.”
To support the definition and development of the consumer-facing offerings, Wellstar has made a $10 million strategic investment in Sharecare, joining several investors who also are customers. The firms will collaborate on platform deployment, integration, and content strategy to drive value for all audiences, with a focus on the consumerization of healthcare and evolving the consumer healthcare experience. As Sharecare’s newest strategic partner, Wellstar is joining the company’s already impressive roster of investors, whose reach extends from the living room to doctors’ exam rooms and into the workplace. Select Sharecare strategic partners include hospitals, healthcare investment firms, and health plans, in particular HCA, Trinity Health, the Heritage Healthcare Innovation Fund and CareFirst; media companies Discovery Communications, Harpo Productions, and Sony Pictures Television; high-growth technology investment firms such as Claritas Capital; noted institutional investment funds such as Wellington Management; and other major reputable corporations such as Aflac Corporate Ventures, Quest Diagnostics, Wells Fargo, and Swiss Re. The partnership between Sharecare and Wellstar is the first of its kind for the two organizations.
The closing date of the strategic investment from Wellstar preceded the February 12, 2021 announcement that Sharecare has entered into a definitive merger agreement with Falcon Capital Acquisition Corp. (NASDAQ: FCAC), a special purpose acquisition company.
At Wellstar, people are at the center of everything we do. By listening actively to what people want, need and expect from their healthcare, Wellstar is able to provide “More than Healthcare. PeopleCare.”—at every age and stage. Nationally ranked and locally recognized for our personal, high-quality care, inclusive culture, and exceptional doctors and team members, Wellstar provides access to compassionate, high-quality care through our: 11 hospitals; 300+ medical office locations; 9 cancer centers; 74 rehabilitation centers; 3 hospice facilities; 1 retirement village; 29 imaging centers; 16 urgent care locations; and 5 health parks. As one of the largest and most integrated healthcare systems in Georgia, Wellstar is growing our services, footprint, capabilities, and ability to meet evolving patient needs. Our passion for people extends into the communities we serve. As a not-for-profit health system, we thoughtfully reinvest annually in prevention and wellness programs, as well as charity care for eligible patients. Our Wellstar Foundation also supports our mission to enhance the health and well-being of every person we serve with funding for equipment, services, and programs that provide more than healthcare.
Sharecare is the leading digital health company that helps people—no matter where they are in their health journey—unify and manage all their health in one place. Our comprehensive and data-driven virtual health platform is designed to help people, providers, employers, health plans, government organizations, and communities optimize individual and population-wide well-being by driving positive behavior change. Driven by our philosophy that we are all together better, at Sharecare, we are committed to supporting each individual through the lens of their personal health and making high-quality care more accessible and affordable for everyone. To learn more, visit sharecare.com.
Falcon Capital Acquisition Corp. is a newly incorporated blank check company whose business purpose is to effect a merger, capital stock exchange, asset acquisition, stock purchase, reorganization or similar business combination with one or more businesses or entities. While the Company may pursue on initial business combination opportunity in any industry or sector, it intends to focus on business in the media, digital media/consumer technology, mobile gaming, interactive entertainment, health wellness/lifestyle and related industries which capitalize on its management team's expertise. The Company's management team is led by Alan G. Mnuchin, the founder and chief executive officer of Ariliam Group. The Company has formed an investment partnership with Eagle Equity Partners, which is a founding investor in the Company's sponsor.
In connection with the proposed business combination, FCAC has filed a registration statement on Form S-4 (the "Registration Statement") with the U.S. Securities and Exchange Commission (the "SEC"), which includes a proxy statement/prospectus, and certain other related documents, to be used at the meeting of FCAC stockholders to approve the proposed business combination. Investors and security holders of FCAC are urged to read the proxy statement/prospectus, any amendments thereto and other relevant documents that will be filed with the SEC carefully and in their entirety when they become available because they will contain important information about Sharecare, FCAC and the proposed business combination. The definitive proxy statement/prospectus will be mailed to stockholders of FCAC as of a record date to be established for voting on the proposed business combination. Investors and security holders will also be able to obtain copies of the Registration Statement and other documents containing important information about the business combination and the parties to the business combination once such documents are filed with the SEC, without charge, at the SEC's web site at www.sec.gov, or by directing a request to: Falcon Capital Acquisition Corp., 660 Madison Avenue, 12th Floor, New York, NY 10065, Attention: Saif Rahman, Chief Financial Officer.
FCAC and its directors and executive officers, under SEC rules, may be deemed participants in the solicitation of proxies from FCAC's stockholders with respect to the proposed business combination. A list of the names of those directors and executive officers and a description of their interests in FCAC is contained in the final prospectus for FCAC's initial public offering, which was filed with the SEC on September 23, 2020, and is available free of charge at the SEC's web site at www.sec.gov, or by directing a request to Falcon Capital Acquisition Corp., 660 Madison Avenue, 12th Floor, New York, NY 10065, Attention: Saif Rahman, Chief Financial Officer. Additional information regarding the interests of such participants will be set forth in the proxy statement/prospectus for the proposed business combination when available. Each of Sharecare and its directors, executive officers and other members of its management and employees, under SEC rules, may also be deemed to be participants in the solicitation of proxies from the stockholders of FCAC in connection with the proposed business combination. A list of the names of such directors and executive officers and information regarding their interests in the business combination will be contained in the proxy statement/prospectus for the proposed business combination when available.

Wellstar: PeopleCare Online
At Wellstar, people are at the center of everything we do, from compassionate medical care in hundreds of locations across Georgia to your online experience of accessing that care. That's why we've redesigned our website with you in mind.
Our new website is crafted to enhance your healthcare experience and features a clean, modern layout that will make it even easier for you to access physicians, make appointments, find services and locations nearby, and so much more.
The new and improved wellstar.org is part of the ongoing evolution of the Wellstar brand and yet another example of PeopleCare. We want to make sure that you get the information and resources you need as quickly as possible.
The updated, mobile-friendly online presence will help you find critical resources in just a few taps. You can easily locate helpful features like “Find a Doctor” and “Pay Your Bill” directly on the homepage. If you are visiting another page on the website, simply click the “For Patients and Families” tab on the top left of the menu bar.
Some key resources on Wellstar's new website include:
Get the most up-to-date information from our health experts by heading to the COVID-19 Resource Center. You'll receive the latest news on the COVID-19 vaccine, testing and other helpful tips like how to care for a sick loved one and managing your mental health during the pandemic.
In addition to the user-friendly design and up-to-date information, our new modern platform provides enhanced stability and security. That means you can always feel safe when browsing our website or paying your bill online.
This launch is just the beginning for wellstar.org, as we continue to address the ever-changing healthcare needs of the community. We hope you like our new digital home!
If you have any questions, comments or concerns, please contact us at [email protected].

JohnCare
John Petrick loves the simple things in life. He revels in time spent with family, reeling in a big catch and feeling the crisp wind in his face during a morning bike ride.
However, for a man that enjoys such simple pleasures, John’s heart health is quite complicated. For a long time, his well-being felt like a puzzle that no one could quite figure out.
John’s complex heart issues first began over two decades ago, when he nearly died after his heart suddenly went into an abnormal rhythm.
After the life-threatening heart episode, specialists in California diagnosed him with ventricular tachycardia (VT), a severe heart condition in which abnormal electrical signals cause the heart to beat faster. Then later, he was also diagnosed with atrial fibrillation (AFib), an irregular and rapid heart rhythm that can cause heart palpitations and shortness of breath.
From defibrillators to heart surgeries, John and his Californian care team worked hard to manage the ups and downs of his heart conditions. But after spending years in the Golden State, John was ready to take on a new adventure: moving over 2,000 miles away to Georgia.
“The decision to move to Georgia was difficult because of my heart conditions,” John shared. “I needed a doctor who would really take the time to sort everything out.”
Luckily, it wasn’t long before John was connected with an entire team of Wellstar heart experts delivering comprehensive care all within the same health system.
Before being referred for specialty care by his Wellstar primary care provider, John briefly received heart care from another health system in Georgia. However, he had some reservations about his treatment.
“Honestly, it wasn’t the level of care—especially in terms of empathy—that I was used to,” he admitted. “And that’s a scary situation when you have a condition like mine.”
That was never a problem at Wellstar. As soon as he met with Wellstar Health System Director of Cardiac Electrophysiology Dr. Narendra Kanuru, John knew the physician was in his corner.
“I could tell Dr. Kanuru really took the time to study my case,” John said, remembering his first visit with the specialist. “He recited my medical history from the last 20 years, without having to look at any papers.”
Since then, they have developed a great healthcare partnership, always keeping an open line of communication.
“I feel so comfortable expressing any fears or apprehensions about my conditions or treatment with Dr. Kanuru. He’s always very receptive,” John shared. “His level of empathy, professional expertise and ability to communicate and understand me is just as valuable as his technical, medical skills.”
Along with Dr. Kanuru’s expertise, Wellstar Cardiologist Dr. David Caras provides an essential complement to John’s cardiovascular care. While a cardiac electrophysiologist hones in on the functional and rhythmic areas of the heart, a cardiologist offers a broad spectrum of heart care.
While each focusing on their areas of expertise, the two heart specialists collaborate to create the best treatment plan for John, and adjust it along the way.
“Dr. Kanuru and Dr. Caras work together as a team,” John said. “It’s truly remarkable and beautiful. Often, I’ll go to see one of the doctors and they’ll mention a conversation they had about me with the other recently.”

John&JaninCare
If “adventure” were a gene, John Petrick surely passed it on to his daughter, Janin.
The father-daughter duo has always wanted to experience everything life has to offer. Together, the pair has survived an avalanche in the Alaskan wilderness, spent the night stranded on a cliff and even made a cross-country move from California to Georgia.
But one thing they never expected to have in common was a rare heart condition.
Instead of putting their shared adventures on pause, John and Janin teamed up with Wellstar in different ways to manage their heart conditions. With an entire team of heart specialists working seamlessly together, the pair found the expert, specialized cardiac care they needed—and it never skipped a beat.
For more than two decades, John managed the ups and downs of atrial fibrillation (AFib) and ventricular tachycardia (VT) with specialists in California. But after moving cross-country to Georgia, he had to start over from scratch.
With such complex heart conditions and a more recent diagnosis of congestive heart failure, John knew he couldn’t trust his care to just anyone. At Wellstar, he soon found an expansive, multidisciplinary team—including cardiologists, electrophysiologists and surgeons.
Similarly, Wellstar would also end up helping John’s daughter, Janin, following her treatment for a severe heart episode—one that was strikingly similar to her father’s. After several spells of faintness, Janin was equipped with a Holter monitor, a wearable device that records heart rhythms.
“After just 18 hours, I got a call from my doctor’s office. My electrophysiologist was gravely concerned about the readings,” Janin recalled. “Apparently, the night before, my heart had completely stopped for five seconds. And, at that very moment, I was in a dangerous arrhythmia.”
Just like her father, Janin was diagnosed with VT and an atrioventricular block, which occurs when the electrical signals traveling from the upper chambers of the heart to the lowers chambers is blocked.
She soon got a defibrillator implanted to help keep her heart in regular rhythm. As Janin started to get back on track after the surgery, her doctor felt more answers could be uncovered. At her electrophysiologist’s suggestion, she participated in genetic testing.
At Wellstar, John underwent the same genetic testing to see if any clues about their heart conditions could be uncovered in their DNA. With just a simple blood draw, the Wellstar genetics team can get an inside look at the hereditary markers for certain genetic conditions.
After sharing so many adventures and similar personality traits, it was no surprise when the results revealed the same exact abnormality in both of their genes.
However, the genetic discovery—playfully nicknamed the “Janin Genome” by John and his daughter—was a first for the heart specialists. While genetic tests for other heart conditions like cardiac disease may be more commonplace, testing for arrhythmic heart disorders like VT is rare.
“When we got the results, they told us, ‘We've never seen this before—such an identical test result, regarding the same gene and the same anomaly affecting heart rhythm,’” John said. “The doctors concluded there may be a genetic connection to our heart problems, and it was worth paying attention to and exploring further.”
The Petricks are now in the process of getting the genetic testing done for the whole family, so all of their loved ones can take charge of their own wellness.
“After we had our testing, it was a starting point for our family,” Janin said, explaining how the genetic testing had a positive ripple effect for her family members. “We encouraged every single one of our blood relatives to go through genetic testing.”

Pregnancy, Breastfeeding & the COVID-19 Vaccine
As you prepare to welcome a new little one to your family, you are faced with so many decisions about childbirth and parenting, which have been complicated by the COVID-19 pandemic. During this exciting but possibly stressful time, your Wellstar provider can guide you through these difficult choices, taking into account your personal medical history and your unique pregnancy situation.
Now that the U.S. Food and Drug Administration has authorized the Moderna, Pfizer and Johnson & Johnson vaccines for emergency use against COVID-19, many patients have questions about how getting the vaccine could affect pregnancy and breastfeeding.
As vaccine supplies become more plentiful and eligibility expands to more age groups, OB/GYN experts recommend that vaccines be offered to those who are pregnant or breastfeeding. Here is their guidance for new mothers considering the COVID-19 vaccine.
According to the American College of Obstetricians and Gynecologists (ACOG), pregnant women are more likely than people who are not pregnant to experience severe illness, be admitted to the ICU and need to use a ventilator for breathing. There is also a higher risk of death from COVID-19.
Don’t worry about the vaccines altering you or your baby’s genetic material—that’s not how the mRNA vaccines currently available work. The CDC and ACOG agree that the vaccine cannot cause any genetic changes in you or your baby because they do not enter the nucleus of cells, where DNA is housed. The vaccines trigger a protein response in your body that helps build immunity. For more information on how the vaccines work, check out Wellstar’s COVID-19 Community Toolkit.
The Society for Maternal Fetal Medicine confirms these vaccines cannot give you or your baby COVID-19. The vaccines currently available contain mRNA, not any form of the COVID-19 virus.
The American Society for Reproductive Medicine and ACOG both recommend that those trying to become pregnant or considering a future pregnancy still get vaccinated. You will not have to delay or avoid pregnancy after getting both doses of the vaccine. There is also no reason to delay pregnancy attempts because you got the vaccine.
ACOG recommends that COVID-19 vaccines be offered to lactating women. The Association of Breastfeeding Medicine agrees and says there is no need to avoid starting or to stop breastfeeding if you get the shot.
If you have any questions about the vaccine’s effect on pregnancy or fertility, a discussion with your women’s health provider could help you make an informed decision together. A phone call or virtual visit with your caregiver is a safe and easy way to get more answers about the COVID-19 vaccine.
American College of Obstetricians and Gynecologists (ACOG) is the foremost professional membership organization for obstetricians and gynecologists. It is comprised of over 60,000 members (board-certified OBGYNs) spanning the entire career lifecycle.
Society for Maternal Fetal Medicine (SMFM) is the professional society made up of OBGYNs with advanced training and focus on high-risk pregnancies and conditions.
American Society for Reproductive Medicine (ASRM) is the professional society made up of OBGYNs with advanced training and focus on infertility.
Academy of Breastfeeding Medicine (ABM) is a global community of medical doctors with diverse backgrounds and specialties creating a network of experts and advocates to drive breastfeeding medicine forward.

Vital Valentines: Celebrating Our Healthcare Heroes
You may be wondering why Valentine’s Day has become such a big deal for a healthcare system like Wellstar. It’s because we aren’t sending our heartfelt thanks and virtual hugs to just anyone. This year, we believe our healthcare heroes deserve all the love and appreciation.
At Wellstar, people are at the heart of everything we do. Our mission is to enhance the health and well-being of every person we serve, and nothing would be possible without the continued commitment of our team members.
Whether they are fighting the virus on the frontlines or working behind the scenes to keep our facilities sparkling clean, each and every team member plays a vital role at Wellstar Health System.
From February 10-14th, we want to honor Wellstar healthcare heroes as “Vital Valentines”—those dedicated to delivering world-class care to Georgia. Our team members always put the health and safety of our patients and communities first, even through the difficulties of the COVID-19 pandemic.
Instead of backing down from the challenges over the past year, our team members have rolled up their sleeves, taken on new responsibilities and shown fearless leadership to continue the life-saving work we do every day.
Please join us in celebrating the selfless commitment of Wellstar’s “Vital Valentines” as we continue to move forward into a new era of hope and healing.
Have you had a standout experience with a Wellstar team member? Tell us how our team has gone above and beyond. Simply write a sweet social post on Facebook, Twitter or Instagram using the hashtags #WellstarHealthSystem and #VitalValentine.
For more feel-good stories about our “Vital Valentines,” follow Wellstar Health System on Facebook, Twitter, Instagram and LinkedIn.

Well Starts with Healthy Hearts
It’s impossible to count all the ways your heart supports you in a single day. Whether it’s checking out a new trail, gardening or simply playing with your kids, every beat of your heart helps you do all the activities you enjoy most.
That’s why it’s so vital to take care of your cardiovascular health—and doing so is easier than you might think. According to Wellstar medical experts, consistency is the key.
“To keep your heart in top shape, make gradual changes sustained over a lifetime,” said Dr. Vivek Nautiyal, Wellstar medical director of preventative cardiology. “Investing in your heart health can be as simple as going for a walk after work, trying a healthy recipe or scheduling that wellness exam you may have been delaying.”
Remember to start small—by just taking a few simple steps, you can keep your heart going strong.
Getting a heart screening is a great way to care for your cardiac health. The Know Your Heart screening program helps catch potential heart problems early, so you can live life to the fullest. Through this testing, you can learn your risk of heart disease and other serious conditions, such as high blood pressure or high cholesterol.
After the screening, you will receive an individualized health report with all the latest stats about your heart. Our team will go over the results with you one-on-one and recommend lifestyle modifications to help you be the healthiest you.
Call (770) 956-STAR (7827) or visit the Know Your Heart page for more information.
Along with monitoring your overall well-being, your primary care provider can help catch potential heart problems early.
“At your annual wellness exam, your provider can assess your risk of certain heart conditions, such as heart disease or high blood pressure,” Dr. Nautiyal explained.
Your provider will check the Foundational 4 numbers that are the cornerstone of general wellness and heart health, including:
“Your provider can help create a personalized plan to keep your heart healthy, which may include diet, exercise or other lifestyle modifications,” Dr. Nautiyal shared. “If you need expert cardiovascular care, they can also refer you to a heart specialist right away.”
When it comes to staying ahead of potential health issues, Dr. Nautiyal also shared the importance of being aware of your family history and cardiovascular stats.
“Be sure to know your cholesterol numbers and seek a preventative cardiology consultation if you have a family history of premature heart attacks, coronary disease or stroke—especially at an age below 55 years old,” Dr. Nautiyal said.
Learn more about the advanced heart care services offered at Wellstar.

High-Tech Cancer Care at Wellstar
At Wellstar, we treat more than patients. We treat people—friends, family, neighbors—who are wholly unique. That’s why our cancer specialists never use a “one-size-fits-all” approach when it comes to your care.
As soon as you are diagnosed with cancer, we provide expert and tailored care that can make all the difference in your treatment and recovery. Our multidisciplinary oncology teams rely on the latest research, innovative treatments and world-class technology to target tumors with precision.
No matter your diagnosis or stage of disease, our cancer experts can create the best and most effective treatment plan for you.
Our dedicated oncology team includes board-certified oncology physicians and surgeons, nurse navigators, registered dietitians and genetic specialists, who are ready to fight alongside you at the first signs of cancer.
Whether you live in the metro Atlanta or West Georgia area, Wellstar makes it easy to find expert care. We have specialized cancer treatment centers close to home, including the newly-renovated Enoch Callaway Cancer Center at Wellstar West Georgia Medical Center and Specialty Teams and Treatment (STAT) Clinics at Wellstar Cobb Hospital, Wellstar Kennestone Hospital and Wellstar North Fulton Hospital.
Here, patients get a customized care plan for their unique cancer diagnosis quickly, instead of waiting weeks or months for treatment.
At the STAT Clinics, each patient has a face-to-face meeting with their oncology team on one day, at one appointment. This multidisciplinary approach helps you get the right treatment for your unique diagnosis as soon as possible.
Wellstar offers a wide range of advanced and minimally-invasive treatment options, such as:
As part of the Mayo Clinic Care network, your trusted Wellstar doctors can combine their understanding of your unique medical needs with Mayo Clinic expertise so that you get exactly the care you need, close to home.
Whether you have just been diagnosed with cancer or are looking for a second opinion, Wellstar’s expert oncology team can help you get back to life faster.

Comprehensive Cancer Care at Wellstar
Wellstar believes not one cancer diagnosis is ever the same.
That’s because each and every person is unique, from their body, genetic makeup, medical history and lifestyle. No matter your cancer diagnosis or stage of disease, our oncology experts create a care plan that is custom-fit for you.
From metro Atlanta to West Georgia, our comprehensive cancer network provides patients with world-class technology, leading expertise and multidisciplinary care through every stage of their cancer treatment.
Wellstar health experts aim to catch cancer early, so you can have the best outcome possible. An annual visit with your primary care provider (PCP) can help you stay ahead of many major diseases, including cancer.
During a wellness exam, our PCPs use preventative health screenings—such as mammograms, colonoscopies and prostate exams—to spot cancer or other potential diseases faster, often before symptoms even appear. Screenings for lung cancer are also available, often ordered for those who have a history of smoking or may have been exposed to carcinogens.
That means we can save more patients’ lives like Frank Ryan, who defeated cancer twice, and Phyliss Davis, who beat breast cancer after being diagnosed during a routine mammogram.
If your family has a history of cancer, a genetic risk assessment can help determine the possibility of you developing the disease and the likelihood of passing the genes to children.
Wellstar invests in state-of-the-art technology to diagnose and treat cancer quickly and effectively. Our patients have access to a wide range of minimally-invasive and cutting-edge cancer treatments, including intraoperative radiation therapy (IORT), stereotactic ablative radiotherapy (SABR) and CyberKnife robotic surgery.
At Wellstar, we understand no person with cancer is exactly alike. That’s why our multidisciplinary team of experts will develop the right treatment for you, considering your unique diagnosis as well as your medical history, health concerns, lifestyle and personal beliefs.
At select Wellstar locations, patients have access to our Specialty Teams and Treatment (STAT) Clinics. Here, people with cancer receive personalized, world-class care while being fast-tracked from diagnosis to treatment in record time.
As part of the Mayo Clinic Care network, your trusted Wellstar doctors can combine their understanding of your unique medical needs with Mayo Clinic expertise so that you get exactly the care you need, close to home.
Any time your doctor wants to confirm a treatment plan or request a second opinion, they can consult directly with Mayo Clinic's top specialists on your condition.
People with cancer can find support from the Wellstar oncology team, including nurse navigators, oncology registered dietitians, psychologists, psychiatrists, social workers and financial counselors.
Cancer and certain treatments can often have physical, psychological or cognitive side effects that may impact your daily life. Cancer rehabilitation and integrated therapies—including acupuncture, yoga and meditation—can help you live your fullest, healthiest life by lessening the side effects of cancer and treatment.
Whether have recently been diagnosed with cancer or are entering remission, education and support are essential. Wellstar offers cancer-related support groups and educational opportunities, such as nutrition and fitness classes, to help you cope.
At Wellstar, you never have to brave cancer alone. Our dedicated oncology team will provide continued, compassionate care for every step of your diagnosis, treatment and recovery.

Expert Stroke Care at Wellstar
No stroke is ever the same. That’s because people—their brains, their nervous systems, their genetics—are all different. At Wellstar, we provide world-class stroke care for each and every patient when they need it most.
During a life-threatening stroke, parts of the brain may become damaged, causing long-term disability, permanent injury or even death. Our trained team understands how getting fast, expert stroke care can mean the difference between life, death or lasting damage.
Wellstar has one of the largest stroke networks in Georgia, so you’ll receive high-quality care wherever you go. Count on our medical experts to treat your stroke as quickly and safely as possible.

PhylissCare
As the matriarch of her family, Phyliss Davis has always taken care of everyone before herself. Between a busy schedule and devoting time to her granddaughter Wynter, Phyliss made a habit of putting her own health on the back-burner.
Hoping to check another job off her to-do list, she finally squeezed a routine wellness appointment onto her calendar. But when Phyliss’ medical chart showed no recent mammogram, her primary care physician grew concerned.
"When my doctor asked how long it had been since my last mammogram, I didn’t want to admit that I hadn’t had one in years," Phyliss said, remembering how the medical professional urged her to get a breast exam as soon as possible. "Because I didn’t have a family history of breast cancer, I thought I didn’t have to worry."
Luckily, Phyliss came in at just the right time. Her mammogram caught a concerning lump that couldn’t be seen with the naked eye. Following a biopsy, she was diagnosed with breast cancer.
Throughout her cancer journey, the grandmother would learn the importance of taking care of her own health and body. And soon, she would truly understand the words her mother told her as a child: "An ounce of prevention is worth a pound of cure."

JohnCare
It seems "defeat" just isn't in John Cashen's vocabulary. A survivor in more ways than one, John has overcome not only a catastrophic natural disaster, but also fought cancer with unyielding resilience.
In 2005, as flood waters from Hurricane Katrina rose and threatened his New Orleans home, John took an axe to his attic's ceiling, climbed atop his roof and tied himself to his chimney so he wouldn't be swept away. Days later, no help had arrived, so John untied himself and swam to an overpass where he was rescued by a helicopter. He joined the rest of his family in Georgia.
Since then, John has become a proud citizen of LaGrange. A master of everything Mardi Gras, John runs a local krewe and is a natural at building parade floats from the foundation up. But when he was diagnosed with lung cancer in 2019, he summoned his fighting spirit, squared his shoulders, and faced his cancer journey head on.

Wellstar Recognized as Cancer Treatment Leader
Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, announced that the Wellstar Cancer Network was recently recognized nationally as a cancer treatment leader. Honored with an Outstanding Achievement Award from the American College of Surgeons Commission on Cancer and designated as a Care Continuum Center of Excellence by the GO2 Foundation for Lung Cancer, the Wellstar Cancer Network continues to pioneer innovative cancer treatments and technologies to improve outcomes and quality of life for patients.
“Wellstar Health System is dedicated to providing patients with the highest quality of compassionate and personalized care,” said Dr. Michael Andrews, Chief Cancer Officer of the Wellstar Cancer Network. “We are extremely proud of the Wellstar Cancer Network and our team of highly skilled physicians, nurses and oncology support services who excel at treating the spectrum of cancer illnesses with the most advanced, patient-centric technologies and treatments. We are focused on enhancing the health and well-being of everyone we serve, with a commitment to delivering world-class cancer care.”
Wellstar earned an Outstanding Achievement Award for the third consecutive cycle from the American College of Surgeons Commission on Cancer (CoC). The highest honor in the United States awarded to a cancer program, the Wellstar Cancer Network was recognized for achieving excellence in providing care to cancer patients. Award recipients must have received commendation ratings in all seven commendation standards and receive a compliance rating for each of the 27 remaining cancer program standards.

Don't Forget Your Flu Shot
At Wellstar, we believe prevention is the best way to protect yourself from a potential flu infection. That’s why it’s important for you and your family to get a flu shot every year.
This year, your loved ones age 12 and older may also choose to get the COVID-19 vaccine to help protect their health.
As we continue to navigate the COVID-19 pandemic, we know it may be confusing to tell the difference between the flu and COVID-19. If you are unsure if you are experiencing flu or COVID-19 symptoms, please see the comparison section below.
Influenza (flu) and COVID-19 are both viral respiratory illnesses and share many common signs and symptoms. Both illnesses are contagious and can be spread through person-to-person contact, although COVID-19 can spread to other people more easily and quickly than the flu. New variants of COVID-19, such as the Delta variant, are more contagious and spreading quickly across the U.S.
Since the flu and COVID-19 have many similar symptoms and traits, it may be difficult to determine which respiratory illness you may be experiencing. According to the Centers for Disease Control (CDC), there are key differences between the two illnesses:
Similarities
*Note: Not everyone with the flu will have a fever. Children under the age of 5 may also be at higher risk of contracting the flu.
Differences
Seasonal flu shots are widely available to the public. With the COVID-19 vaccine now available for people age 12 and older, you and many of your loved ones can choose to be vaccinated to help keep our community safe. Find a location near you through the DPH website or at a local retail pharmacy.
Compared to the flu, people with COVID-19 may often:
Diagnostic testing may be the best way to determine if you are currently infected with COVID-19 or may have had a past infection of the virus.
For more information about COVID-19 testing, click here.
Compared to COVID-19 and even the flu, people with common colds usually experience milder than the other infections. Typically, colds do not result in serious health problems or complications, such as pneumonia or bacterial infections.
People with colds are more likely to have stuffy or runny noses. In general, experiencing fever, chills and headaches are uncommon.
For more detailed information, call (770) 956-STAR (7827) or visit our COVID-19 resource page.

BelindaCare
Belinda Momon has been making music her whole life, encouraging elementary students to build good character, serving as band director, playing percussion and traveling with her church choir. There’s little that can stop this lifelong teacher and Douglas resident.
When Belinda was diagnosed with breast cancer, she knew she could fight it with the same passion she always applied to music. And her victory over the disease became her most important composition.
It all began as a pact between two sisters. After losing their mother to cancer, Belinda and her sister vowed to get mammograms every year. In 2017, everything looked normal until Belinda found a lump.
It was a Friday evening, and Belinda wasted no time and saw her physician.
At Wellstar Douglas Medical Center's Imaging Center, the new mammogram confirmed she had cancer, underscoring the importance of paying attention to your body and discussing any changes with your doctor.
“My sister battled with breast cancer twice. She said ‘if I can get through this, you can get through this,’” Belinda remembers. “I felt encouraged.”
Belinda, who had just wrapped up her 30th year teaching, now had to draw up the same courage she had always instilled in her students.
“There’s so much life that I still need to live,” she said. “I’m not allowing breast cancer to stop me.”
As Belinda started her fight against cancer, she met a nurse navigator at Wellstar Douglas Medical Center who survived breast cancer herself. The nurse helped her make connections and appointments with cancer specialists. At Wellstar, personal connection is at the core of every physician, nurse and team member, extending beyond the walls of our hospitals.
Belinda began chemotherapy treatment to shrink the tumor before surgery. She went to Wellstar Kennestone Regional Medical Center for a mastectomy — a full removal of the breast tissue and lymph nodes. Here, all her previous exams were readily available thanks to Wellstar’s electronic medical record, allowing for a seamless transition between facilities.
In the months following her surgery, Belinda underwent a daily schedule of radiation on the Wellstar Cobb Medical Center campus in Austell. The treatment drained her energy, but not her determination to live life to the fullest.

LlenCare
Llen Ryan has been the rock of her family’s household for more than 50 years, from raising children alongside her husband Frank and watching her grandchildren grow up.
When she started feeling constant back pain six years ago, she knew she wouldn’t give up her independence and exercise routine without a fight. The thought of stopping her daily walks around Kennesaw Mountain bothered her as much as the physical pain itself.
“I couldn’t walk. I was on the couch for a long time, months, because that would help ease the pain somewhat,” Llen said, expressing her frustration with the debilitating back pain. “I couldn’t stand using a cane or a walker anymore.”
That’s when she met Dr. Franklin Lin, a board-certified neurosurgeon and spine surgeon who helped her take the first steps toward better health.
“When I first met Llen, her chronic back pain had begun interfering with her everyday life. She was starting to have difficulty doing the activities she enjoyed,” Dr. Lin recalled.
“After evaluating her condition, it became clear she was suffering from spinal stenosis, a narrowing of the spaces between the spine,” Dr. Lin said, explaining how the condition can be caused by wear and tear over time. “Patients with spinal stenosis can often feel tingling, numbness and a ‘pinching’ sensation in the spine, which can be very painful.”

ZacCare
Looking at Zac DiGiorgio today, you wouldn't know he almost lost his life — twice.
Like any typical guy in his early 20’s, Zac was always on the move. He liked to keep himself busy and lead an active lifestyle.
So naturally, when his parents needed their shutters replaced, Zac was the first to volunteer. With a drill in hand, he climbed up the ladder to replace the old hardware and change out the shutters.
Moments later, everything changed in the blink of an eye.
A terrifying crash sounded from outside the home. Zac’s father, Chris DiGiorgio, rushed out the front door to see a parent’s worst nightmare: his 23-year-old son face down in the driveway, having a seizure.
After shouting to his wife to call 911, Chris was at his son’s side. He cradled Zac on the concrete driveway, trying to steady his body from the convulsions.
“I really didn't know what was happening,” Chris recalled. “I knew he was having a seizure, but I didn't know if he had any other injuries or anything else going on.”
But one thing was clear: Zac had plummeted to the ground from the top of the ladder, smacking the right side of his head hard on the concrete.
The severity of the fall triggered a seizure, often characterized by body spasms or unconsciousness. However, these episodes can also have cognitive and emotional effects, such as fear or anxiety.
In Zac’s case, he became extremely agitated. After waking from the initial seizure, he argued with his dad and fought against his hold. Even when the first responders arrived, he refused to get on the stretcher and instead walked himself to the ambulance.
With lights flashing and sirens blaring, the ambulance raced towards Wellstar Kennestone Hospital. On the way, Zac complained of pain in his shoulder from a broken collar bone. But after experiencing another seizure on the short eight-minute drive, it was clear much more was going on inside his body.
After being admitted, it would be weeks before Zac awoke again in the hospital — with no memory of the accident.

AshleyCare
September hasn't always been Ashley Irwin’s favorite month. Years ago, that time of year when the leaves changed into bright, warm colors held some of the darkest moments of her life.
In 2011, a 28-year-old Ashley was battling a particularly bad bout of Crohn’s disease, an inflammatory illness that can cause painful and often debilitating abdominal and bowel issues.
After the intense flare-up, Ashley was settling in at home again with the assistance of her mother. She was determined to regain her independence and get back on track.
But it wasn’t long before the sharp sensation of a migraine hit her full force. Pushing through the pain, she tried to check her email for any new messages, though it was nearly impossible to type in her username and password.
“As I sat in front of the computer, I couldn’t even remember my last name to log in to my email account—no matter how hard I tried,” Ashley recalled the terrifying moment.
Almost immediately, Ashley’s mother noticed her confusion, and stepped in to assess the situation and double-check her daughter’s cognitive abilities.
“My mom asked me, ‘Who am I? What’s my name?’ In my head, I knew she was my mother, but I just couldn’t connect the dots and express it,” Ashley said, describing her confusion and difficulty thinking. “At that moment, I couldn’t tell you her name or her relationship to me.”
Worried, the mother and daughter rushed to the Emergency Department at Wellstar Kennestone Regional Medical Center for immediate medical treatment. After being evaluated, it was clear that Ashley was dealing with much more than just a bad headache—she was having a stroke.

Make Well Happen
At Wellstar, we know not one person’s life has gone untouched by the COVID-19 pandemic.
Across Georgia — and throughout the world — we’ve had to continue to fight the virus as new variants emerge. But through every challenge and triumph, we’ve all been in this together.
However, hearing the same news reports and safety information over and over can become tiresome. It’s possible to forget what our community has been working towards… but now is not the time to tune out.
Wellness is a two-way street, and it’s up to all of us to make well happen.
That’s because just as much as saving lives and fighting illness happens every day at our Wellstar healthcare facilities, staying well starts with you. When you focus on the wellness of your world — yourself, family and friends — you have a profound impact on people everywhere.
When you join the movement to make well happen, you become a wellness warrior.
As you dedicate yourself to doing your part, Wellstar continues to keep the people and communities we serve safe every day. We have been working hard to make well happen, across all of our hospitals, health parks, urgent care centers and hundreds of medical offices.
Wellstar is ready to protect your health amid the COVID-19 pandemic and beyond. We’re dedicated to delivering safe, expert care to our patients, no matter what their medical concerns may be.
From suiting up in PPE to ensuring our facilities stay sparkling clean, our team members have put additional measures in place to protect you from infection. To learn more, visit our COVID-19 resource page.
As we fight on the frontlines to keep Georgia well, we also look to you. You are a change-maker. When you do your part, we all work together to make well happen.

Wholehearted Healthcare
Johnny “Bow” Matthews was preparing for bed when he felt a tightness in his chest he just couldn’t shake.
He tried to sleep, but chest pains wouldn’t let him drift off. He attempted to wake his wife, Deidra, but she wouldn’t budge.
The mother of two had been up and about all day, from preparing breakfast early in the morning to putting the kids in bed after dinner.
“I told her, ‘Hey, something’s wrong,’ but she was sleeping too deeply and wasn’t comprehending.”
Bow couldn’t afford to wait. As the pain and discomfort worsened, he dressed and drove to the emergency department at Wellstar Cobb Medical Center.

MatthewsCare
Most people can’t wait to leave the hospital. Deidra and Bow Matthews, however, weren’t quite ready on their discharge day.
Deidra had just delivered Chase, a beautiful girl. Holding that tiny, fragile baby in their arms, both new parents felt nervous about what to do next. But the nursing staff at Wellstar Cobb Hospital surrounded them with unfailing support and helped the Matthews family gain more confidence in holding, feeding and swaddling their new bundle of joy.

Heart of the Band
As the tuba player in his band, Frank sets the bass tone for every other instrument, for every song.
“I enjoy being in the New Horizons Band at Kennesaw State University. There, I’m part of a community who loves and supports one another,” Frank said. “I love playing the tuba because I can visualize the people who played before me. And it constantly reminds me that being part of a community makes life worthwhile.” So, when his heart lost its pace, skipping beats and banging against his chest, he knew there was something wrong with the most important instrument in his body.
“I was working out on the elliptical at Wellstar Health Place, and the heart rate monitor on the machine was jumping to 200 beats per minute. I knew something was wrong,” Frank said. “I was already a patient of Dr. Paul Simonoff’s, so I called his office and he took me in right away.”
“Frank’s heart was racing,” said Dr. Simonoff. “He was also experiencing heart palpitations, fatigue and shortness of breath. That’s when I discovered his heart was out of rhythm.” Dr. Simonoff diagnosed him with atrial fibrillation (AFib), which occurs when the upper chambers of the heart—known as atria—beat irregularly and fail to pump blood efficiently to the rest of the body.
The symptoms of AFib are sporadic. You might notice a skipped heartbeat, and then feel a thud or thump, followed by your heart racing for an extended period. You might feel fluttering or jumping, mimicking the effects of a heart attack.
“Dr. Simonoff had to do other diagnoses and perform more tests before I could receive electrical cardioversion shock treatment,” Frank said. Electrical cardioversion shock treatment is a procedure that restores a normal heart rhythm in people with certain types of abnormal heartbeats, Dr. Simonoff explained.
“It often takes only one shock to restore the heart to a regular rhythm,” Dr. Simonoff said, noting that the patient is under general anesthesia during the procedure. “They’re asleep and don’t feel a thing. They’ll wake up from the procedure and ask, ‘So, when are we getting started?,’ and it’s all done. Their heart is already back in rhythm.”
“I haven’t had a problem ever since then, and I’ve been taking my medication to prevent it from happening,” Frank announced. “It’s fully under control.” Dr. Simonoff sees these symptoms frequently and knew that the AFib Clinic at Wellstar Kennestone Regional Medical Center could help Frank. This highly-specialized team provides a thorough clinical evaluation of patients with AFib.
To this day, this is still the only comprehensive and dedicated atrial fibrillation clinic in Georgia. Frank now manages his AFib with medication, regular exercise and checkups. “Frank is doing great,” Dr. Simonoff smiled. “I see him on regularly and his heart has remained a steady rhythm. Our goal is to have patients like Frank be as healthy as possible so they can get back to their lives.”
Thankfully, Frank resumed his place in the New Horizons Band without skipping a beat.
“I don't think we are thankful enough to our doctors or to people who work in healthcare. We are here because they're there,” said Frank. “We’re here because they've done their job and they're dedicated.”

COVID-19: Back to School
At Wellstar, we are here to support your children’s health and safety this school season.
In the wake of COVID-19, returning to school has posed new challenges. For many students, in-person education means scoring A’s while also learning how to stay safe. Some schools have opted for virtual learning, with parents taking on the dual role of caretaker and teacher.
This year, protecting your child’s health is more important than ever. To help them head back to school feeling their best, be sure to schedule a wellness exam with their pediatrician and follow our other helpful tips.
Whether your child is attending school in-person or online, it’s important to teach them the proper steps to protect their health. That’s why Wellstar has created a simple, back-to-school song to make safety easy and fun.
It’s almost too cool for school. Check out the song here and you can even join in on the fun by sharing the video of your child’s rendition on social media.

COVID-19: Keeping Young Adults Safe
At Wellstar, we know many people — especially teens and young adults in their 20s and 30s — may be experiencing ‘COVID fatigue’ after more than a year of the pandemic. However, as COVID-19 cases and new variants of the virus emerge, we must work together to keep the community safe.
During this time, protecting your health means protecting your personal freedom in the future. If you would like to hang out with friends or go on vacation when it’s safe, then it’s important to follow preventative health measures now.
If we all work together now, we can help slow the spread of COVID-19 and get back to normal activities, safely.
Use these helpful tips to keep yourself and others in the community safe:
For more resources and information about how to protect your health during the pandemic, visit our COVID-19 resource page.

Wellstar Kennestone's New Emergency Department is Now Open
At Wellstar, not one patient, symptom or treatment plan is the same—even in an emergency. Now, the new, state-of-the-art emergency department (ED) at Wellstar Kennestone Regional Medical Center delivers quality and compassionate care to every patient, every time.
Located just north of metro Atlanta, this 263,000 sq. ft. medical facility is one of the largest and busiest EDs in the nation and:

Frank&LlenCare
When you first glance at Frank and Ellenora "Llen" Ryan, the word "fighter" likely isn't the top quality that pops into mind.
Between the two of them, they have defeated cancer twice, overcome debilitating spine pain and triumphed over a cardiology episode. Now, they’re fighting Parkinson’s disease with the same energy, confidence and heart.

COVID-19: Taking Care of Your Mental Health
In the wake of the coronavirus COVID-19 outbreak, many people may feel anxiety or stress. Handling strong emotions is a normal response, according to Wellstar health experts.
“Things are changing very rapidly,” says Dr. Chirag Patel, Wellstar Medical Director of Population Health. “This virus is new, and Wellstar has been preparing and taking care of the communities we serve. We also encourage people to take care of themselves physically and mentally.”
According to the CDC, reactions during the outbreak can include:
Figuring out ways to cope with anxiety and stress can help you, your loved ones and your community. If stress begins to interfere with your daily life, reach out to your healthcare provider.
For more information, please see the CDC's website on managing stress in children, adults and medical caregivers.

COVID-19: Summer Safety
At Wellstar, we are committed to keeping you and your family safe every day. As we transition to the summer months, it’s important to continue health precautions to help slow the spread of COVID-19.
With COVID-19 cases on the rise, it’s important to be smart when venturing into public businesses and shared spaces, such as hiking trails, parks and pools. According to Wellstar health experts, the increased activity and contact with others could lead to an increase in COVID-19 cases.
“Although summer can be a relaxing time for us all, it’s not time to become lax with preventative health measures,” said Dr. Chirag Patel, Wellstar Medical Director of Population Health. “Unfortunately, many of our favorite summertime activities, such as visiting the beach or park, can bring large groups of people together and put you or your loved ones at a higher risk for infection.”
“While enjoying the sunshine and fresh air this summer, it’s important to use common sense when venturing into public spaces,” Dr. Patel explained. “People should continue taking extra safety precautions such as social distancing and frequent handwashing. If we’re not careful, the community could see a spike in COVID-19 cases.”
Protect your health and have fun this summer season. Start by getting the COVID-19 vaccine to keep yourself, your loved ones and the community safe.
Here is an easy way to remember how to stay safe:
Before you leave for an outing, don’t forget to take a personal summer safety “go” bag for each member of your family that includes:
For more resources and information about how to protect your health during the pandemic, visit our COVID-19 resource page.

Wellstar Kennestone Receives Georgia Oglethorpe Award for Organizational Excellence
Wellstar Health System, one of Georgia’s largest and most integrated healthcare systems, today announced Wellstar Kennestone Hospital was named the recipient of the prestigious Georgia Oglethorpe Award for 2020, Georgia’s highest level of recognition for organizational performance excellence. Presented by the Florida Sterling Council, the award recognizes organizations and businesses “that have successfully achieved performance excellence within their management and operations.” This award announcement falls on the 70th anniversary of the hospital—a significant milestone in community care.
Due to its high standard for excellence, the Georgia Oglethorpe Award represents one of the most significant levels of recognition an organization can receive. Recipients of the Georgia Oglethorpe Award are examples for excellence for other organizations.
This award is presented after rigorous evaluation to recognize organizations that have achieved management and operations performance excellence. Only 89 organizations have earned awards since 1992 from the Florida Sterling Council—the organization that orchestrates the Georgia Oglethorpe Award. The awards are “presented annually to high performing, role-model organizations, both private and public, that demonstrate superior management approaches and role model results,” according to the Florida Sterling Council.
Founded in 1950, Wellstar Kennestone Hospital is a 633-bed hospital, anchoring the regional medical center located in Marietta, Georgia, and is part of the nationally recognized non-profit Wellstar Health System. The hospital serves hundreds of thousands of visitors each year and consistently demonstrates high performance levels across all metrics, including quality, safety, satisfaction, and operations.
Wellstar invests consistently in new innovations that help address vital healthcare needs, such as Georgia’s first CyberKnife®, TomoTherapy® and da Vinci® robotic surgical systems.
As one of only three Level II trauma centers in Metro Atlanta, and part of the state’s largest trauma network, Wellstar Kennestone operates the second busiest emergency department (ED) in Georgia and the eighth busiest ED in the U.S., caring for more than 138,000 patients per year. The new ED is slated to open late June 2020 and will be one of the top two largest and busiest EDs in the nation, serving up to 600 patients per day and 220,000 patients each year at full capacity, doubling the current trauma and emergency capacity. The 263,000-square-foot facility will include dedicated isolation and decontamination rooms that can be used for patients who present with infectious disease, behavioral health, or chemical contamination issues and multiple entrances for different levels of patient severity. Offering a dedicated pediatric ED and many industry-leading features and processes, the new ED dramatically enhances access for Georgians to vital healthcare needs and will be a model for best practices in emergency services, both for the region and nationally.
Today, Wellstar Kennestone Hospital is honored to celebrate its 70th anniversary. The hospital was founded in 1950 to serve the needs of the rapidly growing Cobb County community, which had tripled in the ten years prior. The May 21, 1950 edition of the Marietta Daily Journal stated the facilities “are said to be among the best available in hospital circles in the Southeast”—a fact that stands true today. For the last 70 years, the hospital has been a pinnacle in the Marietta community and is a destination hospital for North Georgia and neighboring states.
“Every birthday that we celebrate not only signifies our maturity in age but also our advancement in serving our community,” said Mary Chatman, executive vice president of Wellstar Health System and president of Wellstar Kennestone Hospital and Wellstar Windy Hill Hospital. “We, the more than 5,000 employees of Wellstar Kennestone Hospital, are proud to be the healthcare choice for many patients, from the beginning of life, when we celebrate birth, to the end of life, when we demonstrate dignity.”
The hospital’s longest-tenured team member and unofficial historian, Joyce McMurrain, has worked at Kennestone for almost 55 years. Joyce began her career as a staff nurse in the maternity unit and has served in many roles. McMurrain is currently the nurse manager for professional practice and helps to guide rising senior nursing students. “One of my proudest accomplishments is helping Wellstar to re-shape and re-structure women's health services,” said McMurrain. “The hospital moved from a traditional maternity model to a modern family-centered approach that provides women greater access, support, decision-making in the delivery process, childbirth, and care.” She credits her longevity to her credo of believing that we are all connected and that service makes a significant difference in people's lives.
Chatman and McMurrain join Wellstar Kennestone Hospital team members in celebrating this significant milestone 70th anniversary, knowing that the hospital will continue to provide compassionate care for the communities it serves for years to come.

COVID-19: Caring for Children
Wellstar is committed to providing the best and safest care possible to children. Across our health parks, pediatric offices, pediatric emergency departments and dedicated pediatric center, we’ve put extra precautions in place to prevent the spread of infections such as COVID-19 so children can thrive.
When it comes to pediatric surgery, we are committed to providing safe care. Therefore, each child will receive a pre-op COVID-19 test, and we’ve developed this helpful resource for parents so they know what they and their child can expect.
We understand many children may be going through a difficult time during the COVID-19 pandemic, and many may experience anxiety and stress—especially if they can’t visit a loved one in the hospital. Wellstar has created some talking points for parents to help them explain to children why they must not visit at this time.
Additionally, if parents are struggling to keep kids feeling connected during the pandemic, our pediatric experts have developed these great ideas for engaging kids at home.
According to the Centers for Disease Control and Prevention (CDC), children are as likely as adults to contract COVID-19. Some children — especially those with underlying medical conditions — can get severely ill from COVID-19 and may require hospitalization.
The key to slowing the spread of COVID-19 is to limit contact as much as possible. While adults make up the majority of COVID-19 cases, children may be asymptomatic and may pass the virus to others. Children should have limited interaction with higher-risk individuals, such as older adults and those with underlying medical conditions.
If your children may be experiencing COVID-19 symptoms, contact your healthcare provider and keep your children at home and away from others as much as possible.

COVID-19: Caring for Yourself & Others
Wellstar is committed to keeping our communities safe and healthy amid COVID-19 and beyond.
At this time, it’s important to get the COVID-19 vaccine if you can to help protect yourself and others. Be sure to continue following the 3Ws — wear a mask, wash your hands and watch your distance.
COVID-19 is a respiratory illness. The most commonly reported symptoms are:
Other symptoms can include:
“We are finding that 80 percent of COVID-19 cases are mild and can be handled at home,” says Dr. Danny Branstetter, Wellstar Infectious Disease Specialist. “It’s when symptoms worsen and become unmanageable that people will need clinical medical attention. You can also speak with your healthcare provider about potential outpatient treatment, especially if you are a high-risk individual.”
If symptoms get worse, call an emergency department, urgent care, primary care provider or your local health department ahead of time to receive guidance on coming in for testing and treatment.
The CDC advises that caregivers who have had close contact with a confirmed case or someone under investigation for COVID-19 should closely monitor their own health. If you develop symptoms, call your healthcare provider right away.
“It’s important to care for a loved one, but do it safely,” says Dr. Branstetter. “While symptoms of COVID-19 are similar to those of the flu or common cold, we have to remember that this is a new virus and we are still learning about it. The highest levels of research are being conducted to combat this disease, so caregivers at home must exercise caution to protect themselves and others.”
Your healthcare provider and public health staff will evaluate whether you can be cared for at home. If it is determined that you can be isolated at home, you will be monitored by staff from your local or state health department. You should follow these steps until a healthcare provider or local or state health department says you can return to your normal activities.
For more information, visit the CDC.gov.

SeniorCare: How to Cope with COVID-19
Adults age 65 and older are at a higher risk of contracting severe illnesses, including coronavirus (COVID-19). That’s why it’s especially important for older adults to take preventative health measures during a pandemic.
At this time, it’s important for seniors to get the COVID-19 vaccine to protect their health. Be sure to continue to follow the 3Ws — wear a mask, wash your hands and watch your distance.
Under normal circumstances, older adults may experience loneliness and depression. But with the cancellation of many community events and disruption of everyday activities due to COVID-19, the senior population can feel even more isolated.
“Typically, when we reach retirement, we tend to form daily and weekly routines that become very important to us and ensure we are socializing with others and living a fulfilling life,” said Dr. Jeffrey L. Tharp, Wellstar Health System Chief of Primary Care and Medicine Service Line.
“Now that our elderly are practicing social distancing, they no longer have these outlets. This may lead to further downstream effects, such as exercise limitation, nutritional deficiencies and lack of compliance with medical appointments and treatments,” Dr. Tharp explained.
As stress and anxiety about the outbreak increases, seniors may also experience changes in sleep patterns and worsening signs of depression and dementia.
According to the Centers for Disease Control and Prevention (CDC), there are several ways seniors can stay happy and healthy during this difficult time:
For more information, please visit our article about taking care of your mental health.
During this challenging time, friends and family can be an important support system for seniors. Even while social distancing to keep elderly loved ones safe, people can still find ways to connect with them.
Here are some easy ways to help older adults cope with the stress:
Finding ways to help elderly loved ones cope with anxiety and stress can help them stay healthy and hopeful. If you notice stress beginning to interfere with your loved one’s daily life, encourage them to reach out to their healthcare provider.
For more information, please visit the CDC’s website on keeping older adults safe both physically and mentally.

BrettCare
After working in construction for more than 20 years, Brett Faucett knows all about the right building blocks. Piece by piece, a building comes together, but if one brick falls out of line, the whole system can crumble.
That’s why Brett knew something was wrong when the numbness started in his left arm. It came and went several times before he ended up behind the wheel of his car.
Sitting at an intersection, Brett was at a crossroads. He could turn right, attend his out-of-town business meeting, and ignore the sinking feeling inside. Or he could turn left and drive straight to the Emergency Department at Wellstar Kennestone Hospital.
“It’s really hard when you plan on going to work and you know people are counting on you. It’s hard to make that left turn and listen to your body.”
Brett took a deep breath and turned the wheel toward the hospital, forever changing the course of his life.
Wellstar Reveals What Georgians Want from their Healthcare System... and it's Personal
The healthcare landscape and the needs of patients and communities, both throughout Georgia and across the country, are ever changing. Wellstar Health System—nationally ranked and locally recognized for its high-quality care, inclusive culture, and exceptional doctors and team members—actively listens to the people in the communities it serves to best understand and respond to what they want, need, and expect from their healthcare provider.
Actively and regularly listening ensures that Wellstar is evolving alongside its patients and communities, providing not only responsive care to emergent needs, but also ongoing, quality, and personalized care at every age and stage of life. Wellstar spent the last 18 months on a renewed listening journey, interviewing more than 8,000 Georgians, including team members, community partners, patients, and consumers, with the objective of informing strategy and taking action to best serve the healthcare needs of the people they serve.
“Enhancing the health and well-being of people requires pausing—and listening—to what consumers and communities tell us they want, need, and expect for their healthcare journey,” said Candice Saunders, FACHE, president and CEO of Wellstar Health System. “Much of what we hear and learn from our ongoing research is exactly what we strive to deliver to every patient, every time: compassionate, quality care. Over the last year and a half, we heard directly from people across the state that they want to feel valued as a unique person and in control of their healthcare decisions—in partnership with their providers. This insight not only validates our approach to patient care, it guided us to take action and renew our commitment to excellence with a personalized and integrated approach that is more than healthcare."
”Combining these research insights with patient feedback, as well as critical regional insights from its 2019 Community Health Needs Assessment with the Georgia Health Policy Center, Wellstar refined its mission, vision, and values and launched a new brand identity. Today, the not-for-profit announced the launch of its new system-wide brand campaign—“More Than Healthcare. PeopleCare.”
“Many people are asking ‘why now?’, and the answer is that our focus over the past few years has been fully integrating our healthcare service offerings across our entire system to ensure that our patients and communities have access to the care they need and deserve across the entire Wellstar footprint,” said Saunders. “Now, we want to make it clear to everyone we serve that being one of the largest and most integrated healthcare systems in Georgia equips us to provide a full spectrum of world-class health services from birth to end of life. This approach also applies to our team members. We are people taking care of people, and we want to ensure that everyone considers Wellstar a place where individuals can advance their careers and feel appreciated.”
Wellstar now has 11 hospitals; 250+ medical office locations; 9 cancer centers; 55 rehabilitation centers; 3 hospice facilities; 1 retirement village; 21 imaging centers; 15 urgent care locations; and 5 health parks. By doubling in size—growing its services, footprint and capabilities—Wellstar has grown its ability to meet the evolving healthcare needs of patients and communities across Georgia.
By taking the time to listen and understand the individual needs of the communities they serve throughout Georgia, Wellstar is recreating the standard for Georgia healthcare by:
“When you’re 39 years old, you never think you’ll be dealing with something like a heart attack,” said Brett Faucett, a husband and father of two, who drove himself to Wellstar Kennestone Hospital after his arm went numb in the shower. Upon arrival, he was rushed to the operating room for a 99-percent blocked artery. A few years later, it happened again, and he was treated at Wellstar Atlanta Medical Center.
“When you’re in a situation like that, your world is flipped upside down. My family has a dad and a husband because of Wellstar—they saved my life,” said Faucett.
The new brand campaign “More Than Healthcare. PeopleCare.” is centered on real Wellstar patient stories that demonstrate the health system’s commitment to providing personal care that takes each person’s unique life story into account across the continuum of his or her personal healthcare journey – from inpatient to outpatient, pediatric to adult, birth to end of life. For more PeopleCare stories, visit wellstar.org/peoplecare.
Wellstar puts patients and communities in the driver’s seat by listening and providing an extensive choice of facilities and a wide breadth of services so that patients have access to all the options they need to make the best, most informed healthcare decisions. Each Wellstar hospital and healthcare facility offers an access point to a compassionate care team and a wide range of service lines that work in concert to provide personalized care for each patient’s needs.
“There’s no better time than the beginning of the year to reflect, refocus, and rebrand so that patients and communities know who we are and what we do,” said Dave Preston, senior vice president of Brand Experience and Communications at Wellstar. “Our new brand campaign, ‘More Than Healthcare. PeopleCare.’ features real-life patient stories that illustrate Wellstar’s commitment to providing high-quality, tailored care that meets their individual needs at every age and stage of life.”
Wellstar isn’t growing just for growth’s sake. The system has served one out of six Georgians, and patients in 148 out of 159 counties across the state. Wellstar is the only health system in Georgia with a network of Level 1, Level 2, and Level 3 trauma centers located in metro Atlanta to serve the most critical patients with a range of emergency care options. Today, Wellstar Kennestone Hospital operates the busiest emergency department in all of Georgia. The new emergency department will open this year, serving as a beacon for access to emergency care for Georgians. The 263,000 square foot building will connect directly to Wellstar Kennestone Hospital and will hold 166 exam rooms. Upon its completion, it will be the second largest emergency department in the nation.
In addition to its new emergency department, the health system recently opened Wellstar Avalon Health Park, the fifth of its kind, giving patients in greater Atlanta easier access to a variety of high-quality, personalized healthcare services available at one convenient location. The Wellstar health park model gives patients access to primary care physicians and specialist appointments, outpatient procedures, urgent care, physical therapy and imaging in a single building.
The health priorities of the communities Wellstar serves are reflected in the 12 service lines that set the strategy of delivering effective, evidence-based care to their patients. All service lines are led by physician and nurse leaders who work with their team members to develop and deliver tailored care plans that tap the expertise of clinicians in an integrated and personalized manner, depending on specific patient needs.
Wellstar has been able to successfully evolve because of its unwavering commitment to listening to its patients. Truly personal, quality care means its patients have choices and access to the right care, at the right place, and at the right time.
Wellstar’s passion for people extends far beyond its system and into the communities it serves. The health system collaborates with more than 450 community partners to bring important initiatives into its service areas across Georgia.
Being a not-for-profit health system enables Wellstar to offer care when and where it matters most. In 2019, Wellstar provided more than $784 million in charity care, unreimbursed care, and community programs. In 2019, the Community Health Needs Assessment Wellstar conducted in partnership with the Georgia Health Policy Center identified six specific care gaps within the community: food insecurity, opioids and behavioral health, women’s health, cancer, suicide and access to primary care. To address and help fill these gaps, Wellstar convened a group of system-wide experts and community partners to provide services, equipment, prevention and wellness programs such as free mammograms, school health programs, hospital chapels, healing gardens, and more. For example, Wellstar partnered with local organizations to provide first books to every baby born in 2020 at Wellstar Kennestone and Wellstar Douglas Hospitals.
“We have been a partner with Wellstar Health System for more than 20 years,” said Dr. Dwight "Ike" Reighard, president/CEO MUST Ministries and senior pastor of Piedmont Church. “From supporting our 41 food pantries through food drives, including MUST in their annual Day of Service to address food inequities, and supporting the various health needs of our clients, to sponsoring programs like the annual Gobble Jog and the MUST annual Giving Gala, Wellstar has been a steadfast partner, helping us to be a beacon of hope and place of refuge for our neighbors in need with compassion and love. This wouldn’t be possible without community support from partners like Wellstar.
”By taking the time to actively listen, Wellstar’s knowledge has grown, its collaborations have grown, and its capacity to provide integrated, quality care where and when its patients need it most has grown. “More Than Healthcare. PeopleCare.” reflects Wellstar’s commitment to always listening and being there for patients in their hour of need and beyond; understanding the underlying factors that may affect their overall health; and creating processes, programs, and initiatives that promote the personalized care and well-being of every person they serve.

Wellstar is more than healthcare
Not one health journey is the same. That's because people—their health, their bodies, their stories—are all different.
At Wellstar, we know the most important factor in every health decision—you. That’s why we provide personalized care for everyone, whether that’s discussing with your primary care provider daily changes you can make to improve your wellness, navigating a difficult diagnosis with an effective treatment plan or emergency surgery to save your life.
We're here for everyone; for Frank and Llen Ryan, who have received comprehensive, multi-specialty care through all the ups and downs so they can live longer and stronger.
We're here alongside Johnny "Bow" Matthews, who improved his health through diet and exercise after having a heart attack, and for his wife Deidra who delivered two healthy babies. We lead the charge for a two-time heart attack survivor Brett Faucett and his whole family.

Lifesaving Wound Care Treatment in a Family Atmosphere
Two-time breast cancer survivor Heidi Bohlmann was accustomed to successfully facing health challenges. But when stomach pain brought the Roswell resident to Wellstar North Fulton Hospital’s Emergency Department (ED), she faced her ultimate challenge: a torn small intestine, which led to a life-threatening infection.
“I remember being in the ED, then waking up in a hospital room 11 days later with machines all around me,” said Bohlmann, 58. “My family from Wisconsin was there. No one was sure I would pull through.”
Bohlmann underwent surgery to repair her perforated bowel, which included creating a hole in her abdomen so the contents of her small intestine could empty into an external pouch. Called an ileostomy, the procedure allows the intestine to heal.
Wellstar Moving Forward with New Branding
Healthcare is always changing, always evolving. For over 25 years, we’ve made moving forward our mission, whether that’s investing in the most advanced treatments, bringing on only the best and brightest physicians, or giving back to the community we serve.
Now, Wellstar is offering the quality healthcare you’ve come to depend on with a fresh look and feel. Updating our visual identity is the next step in our journey of providing world-class healthcare to every person, every time.
Together, we are one health system over 24,000 members strong, from 11 hospitals, more than 250 medical offices, 9 cancer centers, 21 imaging centers, 5 health parks, and 15 urgent care centers. As the largest healthcare system in Georgia, Wellstar’s new branding represents all these moving parts seamlessly working together.
People are at the center of everything we do and every decision we make. We’re committed to pursuing better care for everyone, whether you’re just starting a family, fighting a chronic illness or staying healthy for retirement. To reflect this, the stylized, medical cross in our new logo embodies the human life cycle. Strong and steady, it moves with confidence and clear direction.
While our outward expression may be changing, we pride ourselves on delivering the same quality of care to you and your family. With our trademark purple, we continue our promise to be there for the biggest moments of your life. This color shows the respect and humility we have for serving the members of our community and staying attuned to the needs of others.
As always, we want to be the most valued and trusted partner in your health journey. In times of hardship, the community often turns to healthcare systems for shelter, care, and support. With the addition of a cool shade of blue to our color palette, it brings balance and new life to Wellstar. Deeply reassuring, this represents stability and calmness in moments of uncertainty.
At Wellstar, we know our patients come from all walks of life and all backgrounds. We provide personalized care for everyone, making an impact on the lives of real people every day.
We are Wellstar—and we are here every step of the way—for you.

Wellstar Paulding Hospital Celebrates Fifth Anniversary
The new Wellstar Paulding Hospital is turning five this September. It was our first opportunity to design a hospital from the ground up, and it became one of the first hospitals in the country to use a geothermal energy system, which uses the heat from below the Earth’s surface to heat and cool the facility.
Paulding Hospital features 112 private inpatient rooms, 40 emergency exam and pediatric emergency exam rooms, seven surgical suites, two GI-specific surgical suites, a bronchoscopy suite and decentralized nursing stations.
The hospital recently celebrated an extraordinary accomplishment when it received the coveted Florida Sterling Georgia Oglethorpe Award, which recognizes the hospital’s exceedingly high performance in patient safety, workforce engagement, and financial stewardship.
Over the years, Paulding kept expanding its list of services, bringing much-needed care close to home. One of these offerings is a state-of-the-art catheterization lab, where patients can get treatment for heart attacks and coronary artery disease. The lab opened in 2017, providing care to patients who previously had to travel to either Cobb or Douglas counties for this same life-saving treatment.
“Wellstar’s philosophy has been to deliver high-quality care to the community,” said Harvey Sacks, MD, who served as Paulding County’s sole cardiologist for several decades. “Bringing interventional cardiology here allows people to be treated near home, and makes it easier for their families to be with them at the hospital. Having family with the patient is an important part of healing.”
That same year Wellstar Paulding was also recognized for innovation and excellence in clinical care for patients with COPD and diabetes. The hospital won second place for its focus on diabetes care, which led to better controlling blood sugar for patients with diabetes while in the hospital. Wellstar Paulding Hospital also won third place for lowering readmission rates for patients with COPD.

New Emergency Equipment to Save Lives
Wellstar Spalding Regional Hospital has begun replacing their emergency medical services (EMS) trucks with innovatively designed trucks to better serve residents in Spalding County. Easily recognizable, the first two of the bright red and white trucks with large purple lettering are now on the streets providing the latest in life-saving technologies for Spalding County, and backup emergency response care for Henry, Lamar, Butts and Pike counties.
The larger of the two EMS trucks is a tall, diesel-driven critical care vehicle equipped with advanced cardiac equipment. The truck also has the capacity to transport up to three patients at one time and is outfitted for neonatal transport. Additionally, it could be used to transport air flight crews to and from the scene and the hospital.
Both trucks feature innovative monitors and mobile hotspots to advance EMS’ use of telemedicine, linking the paramedic, physician and patient while en route to the hospital. Wellstar Spalding Regional EMS was the first to launch this webcam capacity in Georgia.
Each truck is also part of an Infectious Disease Transport Network, the only one between Atlanta and Macon. As members of this network, Wellstar Spalding Regional’s award-winning team of EMS paramedics and EMTs are specially trained and can turn either truck into an “isopod” isolation unit for emerging infectious diseases.
To reduce the number of paramedic back injuries caused by heavy lifting, the trucks incorporate new automated stretchers. These units provide support for emergency personnel by removing the need to lift a 75-pound stretcher along with the weight of the patient. This equipment is well-positioned to save EMS personnel from debilitating back injuries and lengthy rehabilitations, the number one cause of career ending disability in the EMS industry. Considered the safest in the industry, the stretchers also incorporate safety lockdowns from front to back, ensuring the patient is secure while in the truck.
Spalding Regional’s EMS paramedics and EMT’s provided input on the unique internal design to maximize efficiency and safety. For example, the trucks have been fitted with an automated lift to load and unload the large, extremely heavy, oxygen tanks that assist patients experiencing difficulty breathing. Jonathon Johnson, Director of Wellstar Spalding Regional’s EMS is proud of his team.
“Paramedics and EMT’s play a vital role in any system of care, often the first line of medical care for critical patients. This new equipment expands the safety for our patients and our personnel, and continues our long history of dedication and commitment to improvement of patient care in this community.”
Wellstar EMS is available 24/7 and responds to more than 16,500 calls annually with each truck in the fleet running between 200 and 250 hours each month. Each new truck costs the hospital between $150k and $180k. This first new critical care vehicle was purchased and outfitted through a gift from the Dundee Community Association to the Wellstar Foundation.
To keep up with the community’s high-demand, Spalding Regional has plans to replace seven additional trucks and add one more Critical Care truck to its fleet. Donations to the Foundation help. Every dollar designated to Spalding Regional funds much-needed projects that support the health and well-being of the local community. To make a tax-deductible donation, visit wellstar.org/give or call (770) 956-GIVE (4483).

Wellstar Paulding Improves Patient Safety
Wellstar Paulding Hospital’s ICU staff recently celebrated their success at improving patient safety by eliminating catheter-associated urinary tract infections (CAUTI). They have been five years without a CAUTI in the ICU.
Urinary tract infection (UTI) is one of the most common types of healthcare-associated infections, accounting for more than 12 percent of infections reported by acute care hospitals, according to the CDC. Paulding’s ICU and infection control staff joined efforts to decrease the number of CAUTIs.
Some of the interventions were simple policy and process changes, while others required equipment changes. But it was the engagement of the front-line nursing staff that proved crucial to the efforts, which included:
Wellstar Paulding Hospital also celebrated another accomplishment recently. It won the Florida Sterling Georgia Oglethorpe Award, which recognizes the hospital’s exceedingly high performance in patient safety, workforce engagement, and financial stewardship.

Robotic Surgeries Get Patients Back to Their Lives Sooner
No one wants surgery. But when it’s necessary, it makes sense to choose the least invasive, most highly advanced type, if possible. And for a wide variety of surgeries, it is possible. At Wellstar North Fulton Hospital, a team of highly skilled robotic surgeons is using the most advanced technology available to help patients get back to their lives sooner than ever.
“Our team of robotic physicians has collectively performed more than 6,000 surgeries,” said Scott Miller, MD, North Fulton Hospital’s medical director of robotic surgery. “And our specially trained anesthesia team has also provided care to thousands of patients. At North Fulton, we offer the highest level of robotic surgery expertise.”
Robotic surgery specialties at North Fulton Hospital include colorectal, general, gynecologic (oncologic and benign), thoracic, trauma and urologic. And the surgeries are performed by clinical leaders. Dr. Miller, a urologist, was the first surgeon in Georgia to robotically remove a prostate. Named to Atlanta Magazine’s list of Top Doctors for 10 consecutive years, he has also been recognized for the past decade as a “National Top Doctor” by established research firm Castle Connolly Medical Ltd. The list aims to identify the top one percent of specialists and sub-specialists in the US.
Dr. Miller explains that with robot-assisted surgery, the surgical system is operated by a physician sitting a few feet away from the patient. Using a high-powered camera, the surgeon guides the arms of the robot that holds surgical tools, which are inserted into the patient through small incisions. With robotic surgery, the surgeon’s movements are more precise, according to Dr. Miller.
“Robotics allow greater range of motion, and thanks to the magnified, three-dimensional image of the surgical field, we can see the patient’s anatomy in better detail,” he said. “It’s the difference between looking through a window and actually walking into a room.“
With the smaller incisions we make during robotic surgery, there’s less blood loss, less post-operative pain, less scarring, quicker recovery and a lower risk of complications,” adds Dr. Miller, who emphasizes another benefit unique to Wellstar North Fulton Hospital: personal, compassionate care.
“The surgeon you first meet with will be the physician who performs your surgery, and sees you postoperatively. We each personally care for our patients, from start to finish.”
Gregory Coffman, MD General, Trauma and Colorectal
Shelley Dunson-Allen, MD Obstetrics & Gynecology
Caroline Gibbons, MD Gynecology
Scott Miller, MD Urology
Theolyn Price, MD Thoracic
Wellstar Is Now Official Health System Partner of Kennesaw State Athletics
Wellstar Health System has entered into a multi-year sponsorship agreement with The Kennesaw State University Department of Athletics. Wellstar’s investment will provide significant support to KSU’s Department of Athletics and its student-athletes.
Wellstar and Kennesaw State University have a long and active history of collaboration. On Jan. 7, Wellstar also announced that the Wellstar Medical Group will operate the university’s Student Health Services. With a new focus on the health of KSU students and our community, Wellstar is proud to become the “Official Health System Partner of Kennesaw State Athletics.” Through this relationship, we will further Wellstar’s vision—to deliver world-class healthcare, and our mission to improve community health.
In addition to becoming the “Official Heath System Partner of Kennesaw State Athletics,” the sponsorship includes sponsorship signage at Fifth Third Bank Stadium, KSU Convocation Center, Bailey Park and Stillwell Stadium, advertising in game programs, during television and radio broadcasts and on KSUOwls.com, the Department of Athletics’ official website.