Transarterial Chemoembolization and Radioembolization
Study Description
- Treatment of hepatic metastatic disease
- Treatment of primary hepatic malignancy (HCC) in patients who are not transplant candidates or who are currently on UNOS transplant list.
- Angiographic procedure under fluoroscopic guidance.
- Minimally invasive, requiring only common femoral arterial access and IV access.
- Overnight admission for pain/nausea control on IR service (Chemoembolization).
- Radioembolization patients usually are discharged the same day of the procedure.
- Recurrent or progressive disease can be treated over multiple sessions.
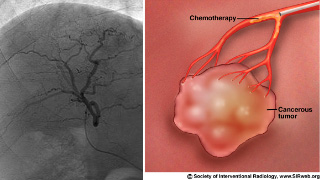
Chemoembolization involves precisely sized drug eluting beads (ion exchange resin with ionically bound drug) which are deposited into the arteries feeding a tumor. The beads themselves block arteries feeding the tumor and the chemotherapy is delivered over time (weeks) locally to the tumor. This results in very high concentrations of chemotherapy agent in and around the tumor with very low systemic concentrations.
Radioembolization is a similar procedure as very tiny spheres loaded with a particle emitter (yttrium 90) are deposited into the liver to irridate metastatic deposits. Used for radiosensitive tumors.

Patient Selection and Indications
- For locoregional treatment and control of primary hepatic malignancies (HCC) and for hepatic metastatic disease (including melanoma, colorectal, lung, etc.).
- Primarily for control of metastatic disease confined to liver.
- May be performed concurrently with systemic chemotherapy.
Patient Preparation
The patient should be referred to Quantum Radiology Interventional Section for assessment of imaging history and physical exam. A thorough review of imaging history, medical history and therapy will be performed and the patient will be scheduled by Quantum for any required laboratory tests (BMP, PT/PTT, CBC) if not already performed within the last 30 days. The patient will then be scheduled for the procedure at a Wellstar facility (Kennestone, Cobb, Douglas).
Contraindications
- History of reaction to chemotherapy agents used (doxorubicin, irinotecan)
- Jaundice
- Occluded portal vein
- Hepatofugal portal vein flow
- Poor liver function
- Creatinine > 2 mg/dL
- Bilirubin > 5 mg/dL
- Hgb < 8 g/dL
- WBC < 2.5K/ uL
- Platelet < 60K/uL
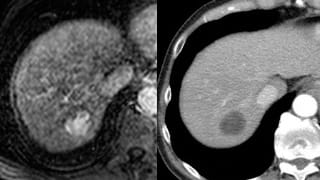
Reporting and Outcomes
A follow up scan should be performed six weeks after the procedure and may be scheduled through the referring physician’s office or by Quantum Interventional. It will be read by a Quantum Diagnostic Radiologist with special training in evaluating post chemoembolization/radioembolization scans. Repeat treatments may be needed depending on tumor response.
Chemoembolization and radioembolization is well tolerated and multiple randomized trials have shown marked survival benefit over other treatment modalities in multiple types of hepatic metastasis as well as in HCC.

