MR of the Uterus
Study Description
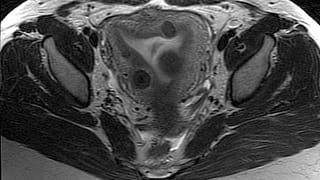
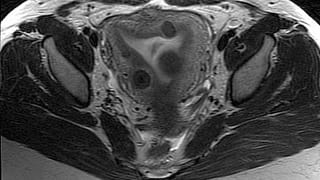
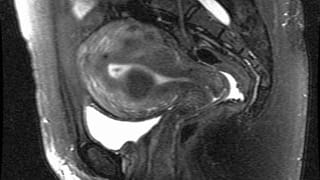
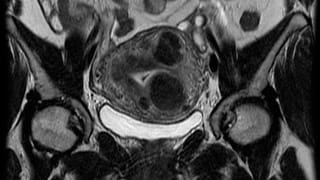
In MR of the uterus for leiomyomas, high-resolution images are obtained in multiple planes. The junctional zone is assessed to exclude adenomyosis, a condition which can often mimic leiomyomas. All leiomyomas are catalogued, with attention to subendometrial lesions, pedunculated lesions, and very large or degenerated fibroids. Imaging is usually performed with intravenous contrast to permit assessment of leiomyoma vascularity, an important predictor of success of uterine fibroid embolization.
Data from the examination can then be used to determine suitability for different interventions such as:
- Uterine fibroid embolization
- Myomectomy
- Hysterectomy
If exam is being done for infertility or if a uterine anomaly is suspected, oblique imaging planes centered on uterus are also obtained. Pulse sequences are optimized to highlight uterine anatomy, providing detailed information that is less operator dependent than ultrasound and more definitive than hysterosalpingogram. MRI is the exam of choice for evaluating uterine anomalies, especially for differentiating septate from bicornuate uterus.
The entire pelvis is imaged to permit evaluation of the parametrium, adnexa, bladder, urethra, pelvic vessels and lymph nodes. In cases of a massively enlarged, leiomyomatous uterus, some of the abdomen may be imaged as well.
Patient Selection and Indications
Common patient symptoms include:
- Low back or pelvic pain
- Painful intercourse
- Pelvic pressure or fullness
- Heavy or extremely painful menses
- Abnormal physical exam or unexplained uterine enlargement
- Frequent urination
- Constipation
Exam may also be performed for:
- Triage of known, symptomatic uterine leiomyoma
- Evaluation of response of leiomyoma to therapy
- Differentiation of leiomyoma from other lesions often seen on ultrasound or CT
- Adenomyosis
- Endometrial Polyp
- Endometrial cancer
Infertility or suspected uterine anomaly on another imaging exam. Uterine anomaly may have implications for carrying pregnancy to term. Conditions such as septate uterus may be corrected surgically with dramatically improved fertility.
Patient Preparation
Standard MRI Precautions should be employed. No patient preparation is necessary.
Gadolinium is given to assess vascularity, the presence of fibrotic tissue, and to help exclude tumor. In patients allergic to gadolinium or in those with renal failure who are at risk for NSF, a non–contrast version of the study can be performed.
The majority of the test is performed with the patient free breathing, but breath holds of short duration may be required depending on the patient’s body habitus and degree of pelvic motion with normal respiration.
Reporting and Outcomes
By using high magnetic field strengths up to 3 Tesla as well as specialty MRI coils, WellStar can offer higher resolution images without prolonging scan times. By obtaining detailed patient histories before each examination, we can select a specialized protocol to address the clinical question. Quantum radiology’s strong relationship with referring clinicians from obstetricians and gynecologists, to oncologist, urologists, and colorectal surgeons enables us to cater to their specific concerns, correlate imaging findings with surgical pathology, and continually improve our performance.
MRI provides soft-tissue contrast superior to competing modalities. It provides an extremely sensitive depiction of fluid and edema. The addition of Gadolinium increases detection of subtle inflammation and small masses, and allows assessment of multiple vascular phases.
As other portions of the pelvis are imaged during MR of the uterus, pathology in other organs may often be detected incidentally. A comprehensive report detailing findings is provided to the referring clinician. If urgent findings are encountered, these are relayed in real time by telephone. A copy of the examination and report is furnished to the patient upon request. The exam may also be reviewed directly with the radiologist in the radiology department at a Wellstar facility.